
- •Foreword I
- •Foreword II
- •Preface
- •Contents
- •1 Abscesses – Pyogenic Type
- •3 Cyst I – Typical Small
- •4 Cyst II – Typical Large with MR-CT Correlation
- •5 Cyst III – Multiple Small Lesions with MR-CT-US Comparison
- •6 Cyst IV – Adult Polycystic Liver Disease
- •7 Cystadenoma / Cystadenocarcinoma
- •8 Hemangioma I – Typical Small
- •10 Hemangioma III – Typical Giant
- •11 Hemangioma IV – Giant Type with a Large Central Scar
- •13 Hemangioma VI – Multiple with Perilesional Enhancement
- •14 Hemorrhage
- •16 Mucinous Metastasis – Mimicking an Hemangioma
- •17 Colorectal Metastases I – Typical Lesion
- •18 Colorectal Metastases II – Typical Multiple Lesions
- •19 Colorectal Metastases III – Metastasis Versus Cyst
- •20 Colorectal Metastases IV – Metastasis Versus Hemangiomas
- •21 Liver Metastases V – Large, Mucinous, Mimicking a Primary Liver Lesion
- •24 Breast Carcinoma Liver Metastases
- •25 Kahler’s Disease (Multiple Myeloma) Liver Metastases
- •26 Melanoma Liver Metastases I – Focal Type
- •27 Melanoma Liver Metastases II – Diffuse Type
- •28 Neuroendocrine Tumor I – Typical Liver Metastases
- •29 Neuroendocrine Tumor II – Pancreas Tumor Metastases
- •30 Neuroendocrine Tumor III – Gastrinoma Liver Metastases
- •31 Neuroendocrine Tumor IV – Carcinoid Tumor Liver Metastases
- •32 Neuroendocrine Tumor V – Peritoneal Spread
- •34 Renal Cell Carcinoma Liver Metastasis
- •35 Cirrhosis I – Liver Morphology
- •36 Cirrhosis II – Regenerative Nodules and Confluent Fibrosis
- •37 Cirrhosis III – Dysplastic Nodules
- •38 Cirrhosis IV – Dysplastic Nodules – HCC Transition
- •39 Cirrhosis V – Cyst in a Cirrhotic Liver
- •40 Cirrhosis VI – Multiple Cysts in a Cirrhotic Liver
- •41 Cirrhosis VII – Hemangioma in a Cirrhotic Liver
- •42 HCC in Cirrhosis I – Typical Small with Pathologic Correlation
- •43 HCC in Cirrhosis II – Small With and Without a Tumor Capsule
- •44 HCC in Cirrhosis III – Nodule-in-Nodule Appearance
- •45 HCC in Cirrhosis IV – Mosaic Pattern with Pathologic Correlation
- •47 HCC in Cirrhosis VI – Mosaic Pattern with Fatty Infiltration
- •48 HCC in Cirrhosis VII – Large Growing Lesion with Portal Invasion
- •49 HCC in Cirrhosis VIII – Segmental Diffuse with Portal Vein Thrombosis
- •50 HCC in Cirrhosis IX – Multiple Lesions Growing on Follow-up
- •51 HCC in Cirrhosis X – Capsular Retraction and Suspected Diaphragm Invasion
- •52 HCC in Cirrhosis XI – Diffuse Within the Entire Liver with Portal Vein Thrombosis
- •53 HCC in Cirrhosis XII – With Intrahepatic Bile Duct Dilatation
- •54 Focal Nodular Hyperplasia I – Typical with Large Central Scar and Septa
- •55 Focal Nodular Hyperplasia II – Typical with Pathologic Correlation
- •57 Focal Nodular Hyperplasia IV – Multiple FNH Syndrome
- •58 Focal Nodular Hyperplasia V – Fatty FNH with Concurrent Fatty Adenoma
- •59 Focal Nodular Hyperplasia VI – Atypical with T2 Dark Central Scar
- •60 Hepatic Angiomyolipoma – MR-CT Comparison
- •61 Hepatic Lipoma – MR-CT-US Comparison
- •62 Hepatocellular Adenoma I – Typical with Pathologic Correlation
- •63 Hepatocellular Adenoma II – Large Exophytic with Pathologic Correlation
- •64 Hepatocellular Adenoma III – Typical Fat-Containing
- •65 Hepatocellular Adenoma IV – With Large Hemorrhage
- •77 Intrahepatic Cholangiocarcinoma – With Pathologic Correlation
- •78 Telangiectatic Hepatocellular Lesion
- •79 Focal Fatty Infiltration Mimicking Metastases
- •80 Focal Fatty Sparing Mimicking Liver Lesions
- •81 Hemosiderosis – Iron Deposition, Acquired Type
- •82 Hemochromatosis – Severe Type
- •83 Hemochromatosis with Solitary HCC
- •84 Hemochromatosis with Multiple HCC
- •85 Thalassemia with Iron Deposition
- •86 Arterioportal Shunt I – Early Enhancing Lesion in a Cirrhotic Liver
- •89 Budd-Chiari Syndrome II – Gradual Deformation of the Liver
- •90 Budd-Chiari Syndrome III – Nodules Mimicking Malignancy
- •92 Caroli’s Disease I – Intrahepatic with Segmental Changes
- •93 Caroli’s Disease II – Involvement of the Liver and Kidneys
- •95 Choledocholithiasis (Bile Duct Stones)
- •96 Gallbladder Carcinoma I – Versus Gallbladder Wall Edema
- •97 Gallbladder Carcinoma II – Hepatoid Type of Adenocarcinoma
- •98 Hilar Cholangiocarcinoma I – Typical
- •99 Hilar Cholangiocarcinoma II – Intrahepatic Mass
- •100 Hilar Cholangiocarcinoma III – Partially Extrahepatic Tumor
- •101 Hilar Cholangiocarcinoma IV – Metal Stent with Interval Growth
- •102 Hilar Cholangiocarcinoma V – Biliary Dilatation Mimicking Klatskin Tumor at CT
- •103 Primary Sclerosing Cholangitis I – Cholangitis and Segmental Atrophy
- •104 Primary Sclerosing Cholangitis II – With Intrahepatic Cholestasis
- •105 Primary Sclerosing Cholangitis III – With Intrahepatic Stones
- •106 Primary Sclerosing Cholangitis IV – With Biliary Cirrhosis
- •107 Primary Sclerosing Cholangitis V – With Intrahepatic Cholangiocarcinoma
- •108 Primary Sclerosing Cholangitis VI – With Hilar Cholangiocarcinoma
- •109 T2 Bright Liver Lesions
- •110 T1 Bright Liver Lesions
- •111 T2 Bright Central Scar
- •112 Lesions in Fatty Liver
- •113 Appendix I: MR Imaging Technique and Protocol
- •114 Appendix II: Liver Segmental and Vascular Anatomy
- •Subject Index

228 Part V – Biliary Tree Abnormalities
107Primary Sclerosing Cholangitis V – With Intrahepatic Cholangiocarcinoma
Primary sclerosing cholangitis (PSC) is a chronic liver disease, characterized by inflammation, destruction and fibrosis of the intrahepatic as well as extrahepatic bile ducts, which eventually results in biliary cirrhosis. The diagnosis is based on a combination of cholestatic liver tests, a characteristic appearance at MRCP – stenotic areas alternating with areas of dilatation – and if necessary a liver biopsy specimen showing periportal inflammation, bile duct destruction, cholestasis, and fibrosis. The disease is usually progressive and the only known treatment for advanced, decompensated disease is orthotopic liver transplantation. Cholangiocarcinoma is a well-known complication of PSC. Currently, there are no simple criteria that determine whether a stricture is benign or malignant in patients with PSC. Although lifetime risks in excess of 30 % have been reported, the risk in most studies is around 10 %. Cholangiocarcinoma may be the first sign of PSC; it can also be found within 2 years after PSC is diagnosed. Ultrasound, CT, and cholangiogram are ineffective in the detection of cholangiocarcinoma in the setting of PSC. We recommend surveillance with MRI/ MRCP in combination with serum cancer antigen (CA 19 – 9).
Literature
1.Ahrendt SA, Pitt HA, Nakeeb A, et al. (1999) Diagnosis and management of cholangiocarcinoma in primary sclerosing cholangitis. J Gastrointest Surg 3:357 – 367
2.Kaya M, de Groen PC, Angulo P, et al. (2001) Treatment of cholangiocarcinoma complicating primary sclerosing cholangitis: the Mayo Clinic experience. Am J Gastroenterol 96:1164 – 1169
3.Goss JA, Shackleton CR, Farmer DG, et al. (1997) Orthotopic liver transplantation for primary sclerosing cholangitis. A 12-year single center experience. Ann Surg 225:472 – 478
4.de Groen PC, Gores GJ, LaRusso NF, et al. (1999) Biliary tract cancers. NEJM 341:1368 – 1378
MR Imaging Findings
State-of-the-art MR imaging, including MRCP and dynamic gado- linium-enhanced sequences, allows early detection of intrahepatic cholangiocarcinoma. Small lesions have predominantly high signal on the T2-weighted sequences. After injection of gadolinium, the lesion typically shows irregular ring-shaped heterogeneous enhancement and washout in the delayed phase. The lesions may show rapid interval growth with even more pronounced arterial enhancement and delayed washout (Figs. 107.1 – 107.3). Comprehensive MR imaging, including MRCP sequences, is essential for the surveillance of patients with PSC.
107 Primary Sclerosing Cholangitis V – With Intrahepatic Cholangiocarcinoma 229
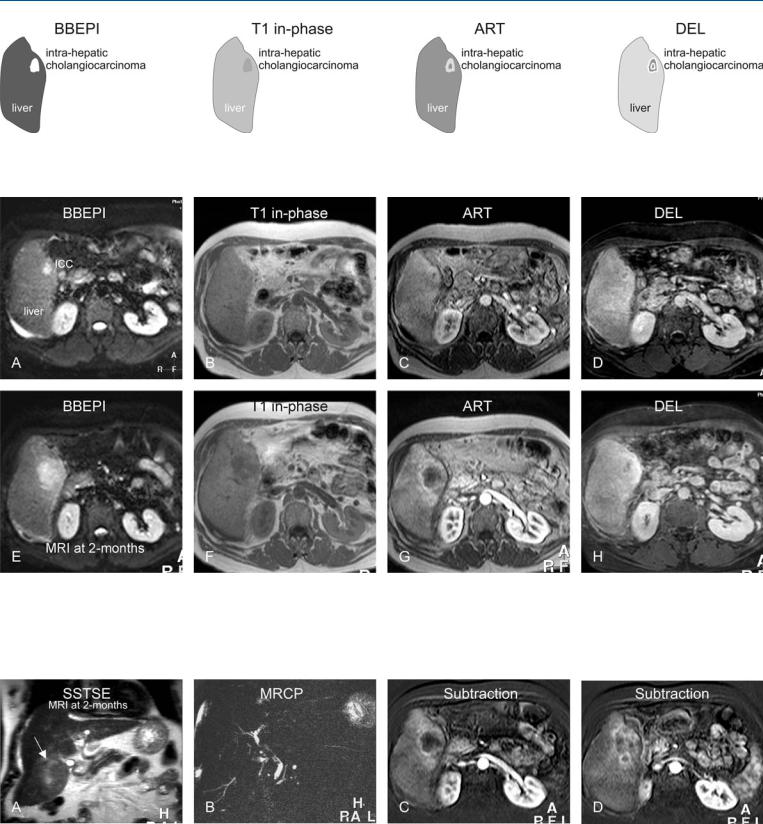
Fig. 107.1. Primary sclerosing cholangitis (PSC) complicated by cirrhosis and an intrahepatic cholangiocarcinoma (ICC), drawings. BBEPI: small ICC is brighter
Fig. 107.2. Primary sclerosing cholangitis (PSC) complicated by cirrhosis and an intrahepatic cholangiocarcinoma (ICC), MRI findings. A Axial BBEPI image (BBEPI): ICC is hyperintense to the liver. B Axial in-phase image (T1 inphase): ICC is hypointense to the liver. C Axial arterial phase image (ART): ICC shows irregular ring-shaped enhancement. D Axial delayed phase im-
than the liver; T1 in-phase: ICC is hypointense to the liver; ART: ICC shows irregular ring-shaped enhancement; DEL: ICC becomes heterogeneous
age (DEL): ICC becomes heterogeneous. E–H MRI at 2 months follow-up: ICC has increased in size and enhancement. Note also in the arterial phase image increased enhancement of the liver surrounding the larger lesion, suggesting more widespread disease
Fig. 107.3. PSC complicated by cirrhosis and an intrahepatic cholangiocarcinoma (ICC), MRI findings at 2 months follow-up (continued). A Coronal SSTSE image shows a cirrhotic liver with a large ICC that is slightly hyperintense to the
liver (arrow). B MRCP shows typical appearance of the biliary tree with PSC. C, D Subtraction of the arterial phase images at two anatomic levels shows the ICC growing along the bile ducts toward the liver hilum

230 Part V – Biliary Tree Abnormalities
108Primary Sclerosing Cholangitis VI – With Hilar Cholangiocarcinoma
Biliary tract cancer is the second most common primary hepatobiliary cancer, after hepatocellular cancer. Approximately 7500 new cases of biliary tract cancer are diagnosed per year; about 5000 of these are gallbladder cancer, and between 2000 and 3000 are bileduct cancers. Currently, the term „cholangiocarcinoma“ includes intrahepatic, perihilar, and distal extrahepatic tumors of the bile ducts. Perihilar tumors involving the bifurcation of the hepatic duct are also called Klatskin tumors, from Klatskin’s original description in 1965. Clinical and biochemical presentation of PSC patients with and without CC does not differ during the year before cancer diagnosis. Liver transplantation is carried out, even in the presence of incidental CC. However, the presence of CC with PSC is associated with poor recipient survival. Recurrent PSC occurs in approximately 9 % of cases after liver transplantation but does not affect patient survival. MR imaging with MRCP is the modality of choice in patients with PSC who need surveillance for hilar cholangiocarcinoma.
Literature
1.Bergquist A, Glaumann H, Persson B, et al. (1998) Risk factors and clinical presentation of hepatobiliary carcinoma in patients with primary sclerosing cholangitis: a case-control study. Hepatology 27:311 – 316
2.Goss JA, Shackleton CR, Farmer DG, et al. (1997) Orthotopic liver transplantation for primary sclerosing cholangitis. A 12-year single center experience. Ann Surg 225:472 – 478
3.de Groen PC, Gores GJ, LaRusso NF, et al. (1999) Biliary tract cancers. NEJM 341:1368 – 1378
MR Imaging Findings
In the setting of PSC and CC, the intrahepatic biliary dilatation will be minimal, which hampers the diagnosis if only MRCP (fluid-sen- sitive) sequence is performed. MR imaging with multiple T1and T2-weighted sequences, as well as dynamic gadolinium-enhanced imaging, is essential for diagnosis. At MR imaging, hilar CC may show a relatively low signal intensity mass surrounding the hilar region. The low signal is likely caused by desmoplasia within the tumor. The tumor will typically show minimal enhancement. MR imaging also allows the evaluation of liver metastases (Figs. 108.1 – 108.3).

108 Primary Sclerosing Cholangitis VI – With Hilar Cholangiocarcinoma 231
Fig. 108.1. Primary sclerosing cholangitis (PSC) complicated by a hilar cholangiocarcinoma (Klatskin), drawings. T2 fatsat: Klatskin is slightly hypointense to the liver; SSTSE: Klatskin tumor is hypointense to the liver and contains an
Fig. 108.2. Primary sclerosing cholangitis (PSC) complicated by a hilar cholangiocarcinoma (CC), MRI findings. A Axial TSE image (T2 fatsat): CC is slightly hypointense to the liver. B Axial SSTSE image (SSTSE): CC is hypointense to the liver and contains an endoprosthesis (central dot of high signal). C Axial arterial phase image (ART): CC shows faint heterogeneous enhancement. D Axial delayed phase image (DEL): CC is slightly more enhanced than the liver. E Axial TSE image (T2 fatsat) at a higher anatomic level shows a focal
endo-prosthesis (central dot of high signal); ART: Klatskin shows faint heterogeneous enhancement; DEL: Klatskin is slightly more enhanced than the liver
lesion consistent with a metastasis (arrow). F A detailed view of the axial SSTSE image (SSTSE): CC is clearly hypointense to the liver with abruptly ending bile ducts. G A detailed view of the axial arterial phase image (ART): CC shows faint heterogeneous enhancement. H Drawing shows typical appearance of the bile ducts with PSC that end abruptly due to the hilar cholangiocarcinoma
Fig. 108.3. PSC complicated by a hilar cholangiocarcinoma, ERCP versus MRCP. A, B Endoscopic retrograde cholangiopancreatography (ERCP) shows findings with suspicion of a hilar malignancy. C, D MRCP (as a part of the MRI
examination shown above) confirms the ERCP findings. Additional MRI sequences are essential for a comprehensive evaluation

Part VI
Differential Diagnosis |
VI |
