
- •Foreword I
- •Foreword II
- •Preface
- •Contents
- •1 Abscesses – Pyogenic Type
- •3 Cyst I – Typical Small
- •4 Cyst II – Typical Large with MR-CT Correlation
- •5 Cyst III – Multiple Small Lesions with MR-CT-US Comparison
- •6 Cyst IV – Adult Polycystic Liver Disease
- •7 Cystadenoma / Cystadenocarcinoma
- •8 Hemangioma I – Typical Small
- •10 Hemangioma III – Typical Giant
- •11 Hemangioma IV – Giant Type with a Large Central Scar
- •13 Hemangioma VI – Multiple with Perilesional Enhancement
- •14 Hemorrhage
- •16 Mucinous Metastasis – Mimicking an Hemangioma
- •17 Colorectal Metastases I – Typical Lesion
- •18 Colorectal Metastases II – Typical Multiple Lesions
- •19 Colorectal Metastases III – Metastasis Versus Cyst
- •20 Colorectal Metastases IV – Metastasis Versus Hemangiomas
- •21 Liver Metastases V – Large, Mucinous, Mimicking a Primary Liver Lesion
- •24 Breast Carcinoma Liver Metastases
- •25 Kahler’s Disease (Multiple Myeloma) Liver Metastases
- •26 Melanoma Liver Metastases I – Focal Type
- •27 Melanoma Liver Metastases II – Diffuse Type
- •28 Neuroendocrine Tumor I – Typical Liver Metastases
- •29 Neuroendocrine Tumor II – Pancreas Tumor Metastases
- •30 Neuroendocrine Tumor III – Gastrinoma Liver Metastases
- •31 Neuroendocrine Tumor IV – Carcinoid Tumor Liver Metastases
- •32 Neuroendocrine Tumor V – Peritoneal Spread
- •34 Renal Cell Carcinoma Liver Metastasis
- •35 Cirrhosis I – Liver Morphology
- •36 Cirrhosis II – Regenerative Nodules and Confluent Fibrosis
- •37 Cirrhosis III – Dysplastic Nodules
- •38 Cirrhosis IV – Dysplastic Nodules – HCC Transition
- •39 Cirrhosis V – Cyst in a Cirrhotic Liver
- •40 Cirrhosis VI – Multiple Cysts in a Cirrhotic Liver
- •41 Cirrhosis VII – Hemangioma in a Cirrhotic Liver
- •42 HCC in Cirrhosis I – Typical Small with Pathologic Correlation
- •43 HCC in Cirrhosis II – Small With and Without a Tumor Capsule
- •44 HCC in Cirrhosis III – Nodule-in-Nodule Appearance
- •45 HCC in Cirrhosis IV – Mosaic Pattern with Pathologic Correlation
- •47 HCC in Cirrhosis VI – Mosaic Pattern with Fatty Infiltration
- •48 HCC in Cirrhosis VII – Large Growing Lesion with Portal Invasion
- •49 HCC in Cirrhosis VIII – Segmental Diffuse with Portal Vein Thrombosis
- •50 HCC in Cirrhosis IX – Multiple Lesions Growing on Follow-up
- •51 HCC in Cirrhosis X – Capsular Retraction and Suspected Diaphragm Invasion
- •52 HCC in Cirrhosis XI – Diffuse Within the Entire Liver with Portal Vein Thrombosis
- •53 HCC in Cirrhosis XII – With Intrahepatic Bile Duct Dilatation
- •54 Focal Nodular Hyperplasia I – Typical with Large Central Scar and Septa
- •55 Focal Nodular Hyperplasia II – Typical with Pathologic Correlation
- •57 Focal Nodular Hyperplasia IV – Multiple FNH Syndrome
- •58 Focal Nodular Hyperplasia V – Fatty FNH with Concurrent Fatty Adenoma
- •59 Focal Nodular Hyperplasia VI – Atypical with T2 Dark Central Scar
- •60 Hepatic Angiomyolipoma – MR-CT Comparison
- •61 Hepatic Lipoma – MR-CT-US Comparison
- •62 Hepatocellular Adenoma I – Typical with Pathologic Correlation
- •63 Hepatocellular Adenoma II – Large Exophytic with Pathologic Correlation
- •64 Hepatocellular Adenoma III – Typical Fat-Containing
- •65 Hepatocellular Adenoma IV – With Large Hemorrhage
- •77 Intrahepatic Cholangiocarcinoma – With Pathologic Correlation
- •78 Telangiectatic Hepatocellular Lesion
- •79 Focal Fatty Infiltration Mimicking Metastases
- •80 Focal Fatty Sparing Mimicking Liver Lesions
- •81 Hemosiderosis – Iron Deposition, Acquired Type
- •82 Hemochromatosis – Severe Type
- •83 Hemochromatosis with Solitary HCC
- •84 Hemochromatosis with Multiple HCC
- •85 Thalassemia with Iron Deposition
- •86 Arterioportal Shunt I – Early Enhancing Lesion in a Cirrhotic Liver
- •89 Budd-Chiari Syndrome II – Gradual Deformation of the Liver
- •90 Budd-Chiari Syndrome III – Nodules Mimicking Malignancy
- •92 Caroli’s Disease I – Intrahepatic with Segmental Changes
- •93 Caroli’s Disease II – Involvement of the Liver and Kidneys
- •95 Choledocholithiasis (Bile Duct Stones)
- •96 Gallbladder Carcinoma I – Versus Gallbladder Wall Edema
- •97 Gallbladder Carcinoma II – Hepatoid Type of Adenocarcinoma
- •98 Hilar Cholangiocarcinoma I – Typical
- •99 Hilar Cholangiocarcinoma II – Intrahepatic Mass
- •100 Hilar Cholangiocarcinoma III – Partially Extrahepatic Tumor
- •101 Hilar Cholangiocarcinoma IV – Metal Stent with Interval Growth
- •102 Hilar Cholangiocarcinoma V – Biliary Dilatation Mimicking Klatskin Tumor at CT
- •103 Primary Sclerosing Cholangitis I – Cholangitis and Segmental Atrophy
- •104 Primary Sclerosing Cholangitis II – With Intrahepatic Cholestasis
- •105 Primary Sclerosing Cholangitis III – With Intrahepatic Stones
- •106 Primary Sclerosing Cholangitis IV – With Biliary Cirrhosis
- •107 Primary Sclerosing Cholangitis V – With Intrahepatic Cholangiocarcinoma
- •108 Primary Sclerosing Cholangitis VI – With Hilar Cholangiocarcinoma
- •109 T2 Bright Liver Lesions
- •110 T1 Bright Liver Lesions
- •111 T2 Bright Central Scar
- •112 Lesions in Fatty Liver
- •113 Appendix I: MR Imaging Technique and Protocol
- •114 Appendix II: Liver Segmental and Vascular Anatomy
- •Subject Index

52 Part IIB – Metastases: Non-Colorectal
24 Breast Carcinoma Liver Metastases
Metastatic breast cancer is the most advanced stage (stage IV) of breast cancer. Most commonly it spreads to bone, followed by lung and liver. Approximately 25 % of breast cancers spread first to the bone. In 21 % of cases, the lung is the only site of metastases. The liver is the third most common site for breast cancer. Two-thirds of women with metastatic breast cancer eventually will have liver metastases. Benign lesions are however common in the general population. It is likely that liver lesions will be present on imaging studies in patients with newly diagnosed breast cancer. An unnecessary liver biopsy can be avoided with the application of the state-of-the- art MR imaging of the liver, which can characterize most of the benign lesions as well as the breast carcinoma metastases.
Literature
1.Noon TC, Semelka RC, Balci NC, et al. (1999) Common occurrence of benign liver lesions in patients with newly diagnosed breast cancer investigated by MRI for suspected liver metastases. JMRI 10:165 – 169
2.Braga L, Semelka RC, Pietrobon L, et al. (2004) Does hypervascularity of liver metastases as detected on MRI predict disease progression in breast cancer patients? AJR Am J Roentgenol 182:1207 – 1213
3.Zimmerman P, Lu DSK, Yang LY, et al. (2000) Hepatic metastases from breast carcinoma: comparison of noncontrast, arterial-dominant, and portal-dominant phase spiral CT. JCAT 24:197 – 203
MR Imaging Findings
At MR imaging, breast carcinoma metastases appear low signal intensity on T1-weighted images and moderately high signal intensity on T2-weighted images with fat suppression. On T2-weighted images, the breast carcinoma metastases in the liver may have a tar- get-like configuration, very similar to the colorectal carcinoma metastases. After administration of gadolinium, breast carcinoma metastases may show variable enhancement patterns including an irregular continuous ring-shaped enhancement in the arterial phase. This ring-shaped enhancement reveals the growing edge of the lesion. In the portal and delayed phase the metastases often show washout in the outer parts and a progressive enhancement toward the center of the lesions. Larger lesions may show heterogeneous enhancement. At computed tomography (CT), the breast carcinoma metastases in the liver have a non-specific appearance (Figs. 24.1 – 24.3).
Differential Diagnosis
MR imaging allows the differentiation of metastatic liver lesions from common benign liver lesions such as cysts, hemangiomas, focal nodular hyperplasia, and focal fatty infiltration. Breast carcinoma metastases may have similarities with other metastases including colorectal.
Management
The majority of treatments for metastatic breast cancer focus on alleviating symptoms and may include radiation therapy, chemotherapy, and hormone therapies.
24 Breast Carcinoma Liver Metastases 53
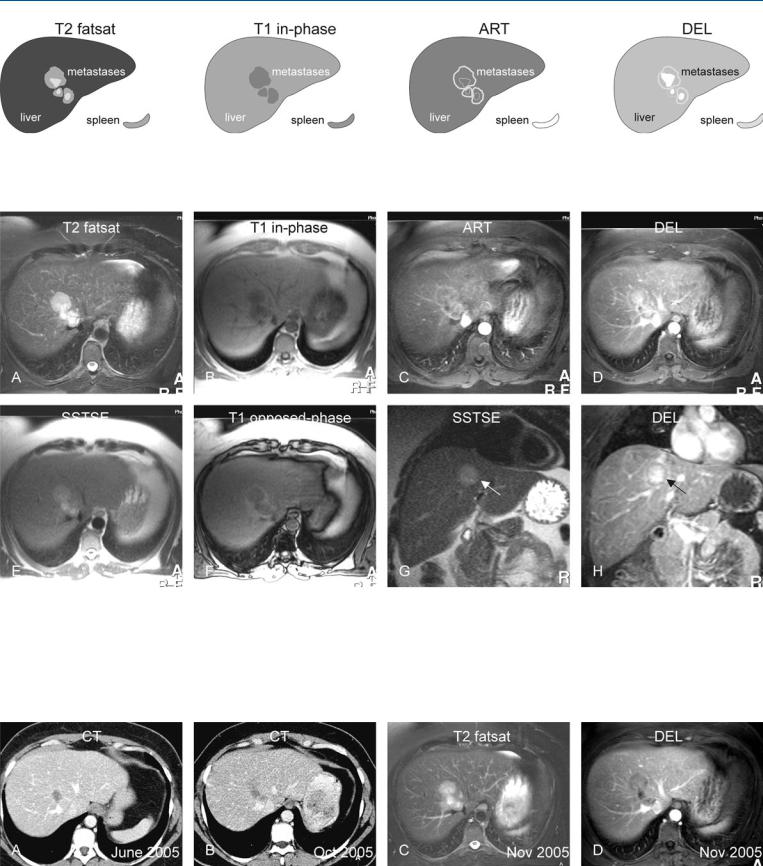
Fig. 24.1. Breast carcinoma metastases, drawings. T2 fatsat: three breast carcinoma metastases are moderately hyperintense with brighter central parts; T1 in-phase: metastases are slightly darker than the liver; ART: metastases
Fig. 24.2. Breast carcinoma metastases, MRI findings. A Axial fatsat T2-w turbo spin echo (TSE) image (T2 fatsat): Three breast carcinoma metastases are moderately hyperintense with brighter central parts, consistent with coagulative necrosis. B Axial in-phase gradient recalled echo (GRE) (T1 in-phase): Metastases are darker to the liver. C Axial arterial phase image (ART): Metastases show faint irregular ring-shaped enhancement. D Axial delayed phase image (DEL): Metastases show peripheral washout with enhanced
show faint ring-shaped enhancement; DEL: metastases show peripheral washout with enhanced central parts
central parts. E Axial single shot TSE (SSTSE) with longer echo time (TE): The solid parts of the lesions become darker than on the T2 fatsat image. F Axial opposed-phase T1-w GRE image (T1 opposed-phase): The liver shows signs of moderate fatty infiltration. G Coronal SSTSE (SSTSE): The largest lesion is well visible (arrow). H Coronal delayed phase image (DEL): The largest lesion shows peripheral washout with enhanced central parts (arrow)
Fig. 24.3. Breast carcinoma metastases, CT versus MRI findings. A Axial CT image shows a hypodense lesion which was considered to indicate suspected metastasis. B Axial CT image (5 months later) shows approximately three lesions which were considered more likely to indicate suspected metastases.
C Axial fat-sat TSE image (T2 fatsat) and D axial delayed phase image (DEL) show lesions with typical appearance of metastases, rendering the diagnosis with a much higher level of confidence

54 Part IIB – Metastases: Non-Colorectal
25 Kahler’s Disease (Multiple Myeloma) Liver Metastases
Kahler’s disease or multiple myeloma is a malignant proliferation of plasma cells usually located in the bone marrow. The extramedullary involvement occurs and is found in about 70 % of autopsy cases. Hepatic involvement in multiple myeloma has not been proven to have major therapeutic consequences. Liver tests may be abnormal and the liver lesions may mimic metastatic disease. It can also be clinically and biologically silent. Ultrasound (US)-guided biopsy may facilitate diagnosis. MR imaging may have some advantage because of the high prevalence of benign lesions in the general population and a relatively low specificity of CT and US for liver lesions. MR imaging should be considered in patients with multiple myeloma with suspicion of hepatic spread.
Literature
1.Chemlal K, Couvelard A, Grange MJ, et al. (1999) Nodular lesions of the liver revealing multiple myeloma. Leukemia Lymphoma 33:389 – 392
2.Nguyen BD, Dash N, Lupetin AR (1992) MR imaging of hepatic plasmacytoma: a case report. Clin Imag 16:98 – 101
3.Caturelli E, Squillante MM, Castalvetere M, et al. (1993) Myelomatous nodular lesions of the liver: diagnosis by ultrasound-guided fine needle biopsy. J Clin Ultras 21:133 – 137
4.Dohy H, Abe T, Takata N, et al. (1979) Successful hepatectomy for solitary plasmacytoma. N Engl J Med 300:1218 – 1219
5.Thiruvengadam R, Remedios BP, Goolsby HJ, et al. (1990) Multiple myeloma presenting as space-occupying lesions of the liver. Cancer 65:2784 – 2786
MR Imaging Findings
At MR imaging the lesions are hyperintense on T2-weighted images and typically hypointense on T1-weighted images. After injection of gadolinium, in the arterial phase, the central parts of the lesion will show intense enhancement. In the delayed phase, the entire lesion will be enhanced, with persistent enhancement in the later phases. On the T1-w opposed-phase imaging, diffuse fatty infiltration may be present in combination with perifocal fatty sparing due to the parenchymal or vascular compression. Extrahepatic lesions, particularly with bones, may be present. Such lesions show similar arterial enhancement to the liver lesions (Figs. 25.1, 25.2). MR imaging can visualize the vascularity as well as the interval growth. US is non-specific and the lesions may even mimic cysts in the setting of steatosis with increased echogenicity of the background liver (Fig. 25.3).
Differential Diagnosis
The differential diagnosis may include other hypervascular liver metastases, such neuroendocrine types.
Management
MR imaging may facilitate the diagnosis or help to distinguish the solid versus the non-solid lesions and avoid unnecessary biopsy in the setting of multiple myeloma with suspicion of hepatic dissemination. Treatment may include surgery.

25 Kahler’s Disease (Multiple Myeloma) Liver Metastases 55
Fig. 25.1. Metastases, hypervascular Kahler liver and skeletal lesions, drawings.
T2 fatsat: metastasis in the liver is very bright; T1 in-phase: metastasis is hypointense to the liver; ART: at least a part of the lesion shows intense
Fig. 25.2. Metastases, hypervascular Kahler liver and skeletal lesions, MRI findings. A Axial TSE image (T2 fatsat): Metastasis in the liver is very bright. B Axial in-phase image (T1 in-phase): Metastasis is hypointense to the liver. Ghost artifact from the aorta (open arrow). C Axial arterial phase image (ART): At least a part of the lesion shows intense enhancement. Note also the vertebral lesions (arrow). D Axial delayed phase image (DEL): Metastasis shows persistent enhancement of the entire lesion. E Axial SSTSE image
enhancement; DEL: metastasis shows persistent enhancement of the entire lesion
(T2 fatsat): Metastasis is relatively bright to the liver. F Axial opposed-phase image (T1 opposed-phase) shows fatty infiltration in a part of the liver (*). Note the fatty sparing, especially around the liver lesion. G Axial portal phase image (POR) shows persistent and perilesional enhancement of the liver metastasis as well as the vertebral lesions. H Subtraction image shows the enhanced liver and vertebral lesions
Fig. 25.3. Metastases, hypervascular Kahler liver and skeletal lesions, relative enhancement (computer-generated image); US and MRI findings (another patient). A Relative enhancement based on the arterial phase image shows most in-
tense enhancement in the center of the lesion. B–D US and MRI show liver and skeletal metastases in another patient
