
- •Dedication
- •Editors and Contributors
- •Foreword
- •Preface
- •Contents
- •PREPARING FOR THE SURGERY CLERKSHIP
- •SURGICAL NOTES
- •COMMON ABBREVIATIONS YOU SHOULD KNOW
- •RETRACTORS (YOU WILL GET TO KNOW THEM WELL!)
- •SUTURE MATERIALS
- •WOUND CLOSURE
- •KNOTS AND EARS
- •INSTRUMENT TIE
- •TWO-HAND TIE
- •COMMON PROCEDURES
- •NASOGASTRIC TUBE (NGT) PROCEDURES
- •CHEST TUBES
- •NASOGASTRIC TUBES (NGT)
- •FOLEY CATHETER
- •CENTRAL LINES
- •MISCELLANEOUS
- •THIRD SPACING
- •COMMON IV REPLACEMENT FLUIDS (ALL VALUES ARE PER LITER)
- •CALCULATION OF MAINTENANCE FLUIDS
- •ELECTROLYTE IMBALANCES
- •ANTIBIOTICS
- •STEROIDS
- •HEPARIN
- •WARFARIN (COUMADIN®)
- •MISCELLANEOUS AGENTS
- •NARCOTICS
- •MISCELLANEOUS
- •ATELECTASIS
- •POSTOPERATIVE RESPIRATORY FAILURE
- •PULMONARY EMBOLISM
- •ASPIRATION PNEUMONIA
- •GASTROINTESTINAL COMPLICATIONS
- •ENDOCRINE COMPLICATIONS
- •CARDIOVASCULAR COMPLICATIONS
- •MISCELLANEOUS
- •HYPOVOLEMIC SHOCK
- •SEPTIC SHOCK
- •CARDIOGENIC SHOCK
- •NEUROGENIC SHOCK
- •MISCELLANEOUS
- •URINARY TRACT INFECTION (UTI)
- •CENTRAL LINE INFECTIONS
- •WOUND INFECTION (SURGICAL SITE INFECTION)
- •NECROTIZING FASCIITIS
- •CLOSTRIDIAL MYOSITIS
- •SUPPURATIVE HIDRADENITIS
- •PSEUDOMEMBRANOUS COLITIS
- •PROPHYLACTIC ANTIBIOTICS
- •PAROTITIS
- •MISCELLANEOUS
- •CHEST
- •ABDOMEN
- •MALIGNANT HYPERTHERMIA
- •MISCELLANEOUS
- •OVERVIEW
- •CHOLECYSTOKININ (CCK)
- •SECRETIN
- •GASTRIN
- •SOMATOSTATIN
- •MISCELLANEOUS
- •GROIN HERNIAS
- •HERNIA REVIEW QUESTIONS
- •ESOPHAGEAL HIATAL HERNIAS
- •PRIMARY SURVEY
- •SECONDARY SURVEY
- •TRAUMA STUDIES
- •PENETRATING NECK INJURIES
- •MISCELLANEOUS TRAUMA FACTS
- •PEPTIC ULCER DISEASE (PUD)
- •DUODENAL ULCERS
- •GASTRIC ULCERS
- •PERFORATED PEPTIC ULCER
- •TYPES OF SURGERIES
- •STRESS GASTRITIS
- •MALLORY-WEISS SYNDROME
- •ESOPHAGEAL VARICEAL BLEEDING
- •BOERHAAVE’S SYNDROME
- •ANATOMY
- •GASTRIC PHYSIOLOGY
- •GASTROESOPHAGEAL REFLUX DISEASE (GERD)
- •GASTRIC CANCER
- •GIST
- •MALTOMA
- •GASTRIC VOLVULUS
- •SMALL BOWEL
- •APPENDICITIS
- •CLASSIC INTRAOPERATIVE QUESTIONS
- •APPENDICEAL TUMORS
- •SPECIFIC TYPES OF FISTULAS
- •ANATOMY
- •COLORECTAL CARCINOMA
- •COLONIC AND RECTAL POLYPS
- •POLYPOSIS SYNDROMES
- •DIVERTICULAR DISEASE OF THE COLON
- •ANATOMY
- •ANAL CANCER
- •ANATOMY
- •TUMORS OF THE LIVER
- •ABSCESSES OF THE LIVER
- •HEMOBILIA
- •ANATOMY
- •PHYSIOLOGY
- •PATHOPHYSIOLOGY
- •DIAGNOSTIC STUDIES
- •BILIARY SURGERY
- •OBSTRUCTIVE JAUNDICE
- •CHOLELITHIASIS
- •ACUTE CHOLECYSTITIS
- •ACUTE ACALCULOUS CHOLECYSTITIS
- •CHOLANGITIS
- •SCLEROSING CHOLANGITIS
- •GALLSTONE ILEUS
- •CARCINOMA OF THE GALLBLADDER
- •CHOLANGIOCARCINOMA
- •MISCELLANEOUS CONDITIONS
- •PANCREATITIS
- •PANCREATIC ABSCESS
- •PANCREATIC NECROSIS
- •PANCREATIC PSEUDOCYST
- •PANCREATIC CARCINOMA
- •MISCELLANEOUS
- •ANATOMY OF THE BREAST AND AXILLA
- •BREAST CANCER
- •DCIS
- •LCIS
- •MISCELLANEOUS
- •MALE BREAST CANCER
- •BENIGN BREAST DISEASE
- •CYSTOSARCOMA PHYLLODES
- •FIBROADENOMA
- •FIBROCYSTIC DISEASE
- •MASTITIS
- •BREAST ABSCESS
- •MALE GYNECOMASTIA
- •ADRENAL GLAND
- •ADDISON’S DISEASE
- •INSULINOMA
- •GLUCAGONOMA
- •SOMATOSTATINOMA
- •ZOLLINGER-ELLISON SYNDROME (ZES)
- •MULTIPLE ENDOCRINE NEOPLASIA
- •THYROID DISEASE
- •ANATOMY
- •PHYSIOLOGY
- •HYPERPARATHYROIDISM (HPTH)
- •PARATHYROID CARCINOMA
- •SOFT TISSUE SARCOMAS
- •LYMPHOMA
- •SQUAMOUS CELL CARCINOMA
- •BASAL CELL CARCINOMA
- •MISCELLANEOUS SKIN LESIONS
- •STAGING
- •INTENSIVE CARE UNIT (ICU) BASICS
- •INTENSIVE CARE UNIT FORMULAS AND TERMS YOU SHOULD KNOW
- •SICU DRUGS
- •INTENSIVE CARE PHYSIOLOGY
- •HEMODYNAMIC MONITORING
- •MECHANICAL VENTILATION
- •PERIPHERAL VASCULAR DISEASE
- •LOWER EXTREMITY AMPUTATIONS
- •ACUTE ARTERIAL OCCLUSION
- •ABDOMINAL AORTIC ANEURYSMS
- •MESENTERIC ISCHEMIA
- •MEDIAN ARCUATE LIGAMENT SYNDROME
- •CAROTID VASCULAR DISEASE
- •CLASSIC CEA INTRAOP QUESTIONS
- •SUBCLAVIAN STEAL SYNDROME
- •RENAL ARTERY STENOSIS
- •SPLENIC ARTERY ANEURYSM
- •POPLITEAL ARTERY ANEURYSM
- •MISCELLANEOUS
- •PEDIATRIC IV FLUIDS AND NUTRITION
- •PEDIATRIC BLOOD VOLUMES
- •FETAL CIRCULATION
- •ECMO
- •NECK
- •ASPIRATED FOREIGN BODY (FB)
- •CHEST
- •PULMONARY SEQUESTRATION
- •ABDOMEN
- •INGUINAL HERNIA
- •UMBILICAL HERNIA
- •GERD
- •CONGENITAL PYLORIC STENOSIS
- •DUODENAL ATRESIA
- •MECONIUM ILEUS
- •MECONIUM PERITONITIS
- •MECONIUM PLUG SYNDROME
- •ANORECTAL MALFORMATIONS
- •HIRSCHSPRUNG’S DISEASE
- •MALROTATION AND MIDGUT VOLVULUS
- •OMPHALOCELE
- •GASTROSCHISIS
- •POWER REVIEW OF OMPHALOCELE AND GASTROSCHISIS
- •APPENDICITIS
- •INTUSSUSCEPTION
- •MECKEL’S DIVERTICULUM
- •NECROTIZING ENTEROCOLITIS
- •BILIARY TRACT
- •TUMORS
- •PEDIATRIC TRAUMA
- •OTHER PEDIATRIC SURGERY QUESTIONS
- •POWER REVIEW
- •WOUND HEALING
- •SKIN GRAFTS
- •FLAPS
- •SENSORY SUPPLY TO THE HAND
- •CARPAL TUNNEL SYNDROME
- •ANATOMY
- •MISCELLANEOUS
- •NOSE AND PARANASAL SINUSES
- •ORAL CAVITY AND PHARYNX
- •FACIAL FRACTURES
- •ENT WARD QUESTIONS
- •RAPID-FIRE REVIEW OF MOST COMMON CAUSES OF ENT INFECTIONS
- •THORACIC OUTLET SYNDROME (TOS)
- •CHEST WALL TUMORS
- •DISEASES OF THE PLEURA
- •DISEASES OF THE LUNGS
- •DISEASES OF THE MEDIASTINUM
- •DISEASES OF THE ESOPHAGUS
- •ACQUIRED HEART DISEASE
- •CONGENITAL HEART DISEASE
- •CARDIAC TUMORS
- •DISEASES OF THE GREAT VESSELS
- •MISCELLANEOUS
- •BASIC IMMUNOLOGY
- •CELLS
- •IMMUNOSUPPRESSION
- •OVERVIEW OF IMMUNOSUPPRESSION MECHANISMS
- •MATCHING OF DONOR AND RECIPIENT
- •REJECTION
- •ORGAN PRESERVATION
- •KIDNEY TRANSPLANT
- •LIVER TRANSPLANT
- •PANCREAS TRANSPLANT
- •HEART TRANSPLANT
- •INTESTINAL TRANSPLANTATION
- •LUNG TRANSPLANT
- •TRANSPLANT COMPLICATIONS
- •ORTHOPAEDIC TERMS
- •TRAUMA GENERAL PRINCIPLES
- •FRACTURES
- •ORTHOPAEDIC TRAUMA
- •DISLOCATIONS
- •THE KNEE
- •ACHILLES TENDON RUPTURE
- •ROTATOR CUFF
- •MISCELLANEOUS
- •ORTHOPAEDIC INFECTIONS
- •ORTHOPAEDIC TUMORS
- •ARTHRITIS
- •PEDIATRIC ORTHOPAEDICS
- •HEAD TRAUMA
- •SPINAL CORD TRAUMA
- •TUMORS
- •VASCULAR NEUROSURGERY
- •SPINE
- •PEDIATRIC NEUROSURGERY
- •SCROTAL ANATOMY
- •UROLOGIC DIFFERENTIAL DIAGNOSIS
- •RENAL CELL CARCINOMA (RCC)
- •BLADDER CANCER
- •PROSTATE CANCER
- •BENIGN PROSTATIC HYPERPLASIA
- •TESTICULAR CANCER
- •TESTICULAR TORSION
- •EPIDIDYMITIS
- •PRIAPISM
- •ERECTILE DYSFUNCTION
- •CALCULUS DISEASE
- •INCONTINENCE
- •URINARY TRACT INFECTION (UTI)
- •MISCELLANEOUS UROLOGY QUESTIONS
- •Rapid Fire Power Review
- •TOP 100 CLINICAL SURGICAL MICROVIGNETTES
- •Figure Credits
- •Index

354 Section II / General Surgery
ABSCESSES OF THE LIVER
What is a liver abscess?
What are the types of liver abscess?
What is the most common location of abscess in the liver?
Abscess (collection of pus) in the liver parenchyma
Pyogenic (bacterial), parasitic (amebic), fungal
Right lobe left lobe
What are the sources? Direct spread from biliary tract infection or
Portal spread from GI infection (e.g., appendicitis, diverticulitis)
Systemic source (bacteremia)
Liver trauma (e.g., liver gunshot wound) Cryptogenic (unknown source)
What are the two most common types?
Bacterial (most common in the United States) and amebic (most common worldwide)
BACTERIAL LIVER ABSCESS
What are the three most common bacterial organisms affecting the liver?
What are the most common sources/causes of bacterial liver abscesses?
What are the signs/ symptoms?
What is the treatment?
Gram negatives: E. coli, Klebsiella, and Proteus
Cholangitis, diverticulitis, liver cancer, liver metastasis
Fever, chills, RUQ pain, leukocytosis, increased liver function tests (LFTs), jaundice, sepsis, weight loss
IV antibiotics (triple antibiotics with metronidazole), percutaneous drainage with CT scan or U/S guidance
What are the indications for operative drainage?
Multiple/loculated abscesses or if multiple percutaneous attempts have failed
|
Chapter 52 / Liver 355 |
AMEBIC LIVER ABSCESS |
|
|
|
What is the etiology? |
Entamoeba histolytica (typically reaches |
|
liver via portal vein from intestinal |
|
amebiasis) |
How does it spread? |
Fecal–oral transmission |
What are the risk factors? |
Patients from countries south of the |
|
U.S.–Mexican border, institutionalized |
|
patients, homosexual men, alcoholic |
|
patients |
What are the signs/ |
RUQ pain, fever, hepatomegaly, diarrhea |
symptoms? |
Note: chills are much less common with |
|
amebic abscesses than with pyogenic |
|
abscesses |
Which lobe is most |
Right lobe of the liver |
commonly involved? |
|
Classic description of |
“Anchovy paste” pus |
abscess contents? |
|
How is the diagnosis made? |
Lab tests, ultrasound, CT scan |
What lab tests should be |
Indirect hemagglutination titers for |
performed? |
Entamoeba antibodies elevated in 95% |
|
of cases, elevated LFTs |
What is the treatment? |
Metronidazole IV |
What are the indications for |
Refractory to metronidazole, bacterial |
percutaneous surgical |
co-infection, or peritoneal rupture |
drainage? |
|
What are the possible |
Erosion into the pericardial sac |
complications of large left |
(potentially fatal!) |
lobe liver amebic abscess? |
|
HYDATID LIVER CYST |
|
|
|
What is it? |
Usually a right lobe cyst filled with |
|
Echinococcus granulosus |
356 Section II / General Surgery |
|
What are the risk factors? |
Travel; exposure to dogs, sheep, and |
|
cattle (carriers) |
What are the signs/ |
RUQ abdominal pain, jaundice, |
symptoms? |
RUQ mass |
How is the diagnosis made? |
Indirect hemagglutination antibody test |
|
(serologic testing), Casoni skin test, |
|
ultrasound, CT, radiographic imaging |
What are the findings |
Possible calcified outline of cyst |
on AXR? |
|
What are the major risks? |
Erosion into the pleural cavity, |
|
pericardial sac, or biliary tree |
|
Rupture into the peritoneal cavity |
|
causing fatal anaphylaxis |
What is the risk of surgical removal of echinococcal (hydatid) cysts?
When should percutaneous drainage be performed?
What is the treatment?
Rupture or leakage of cyst contents into the abdomen may cause a fatal anaphylactic reaction
Never; may cause leaking into the peritoneal cavity and anaphylaxis
Mebendazole, followed by surgical resection; large cysts can be drained and then injected with toxic irrigant (scoliocide) into the cyst unless aspirate is bilious (which means there is a biliary connection) followed by cyst removal
Which toxic irrigations are |
Hypertonic saline, ethanol, or cetrimide |
|
used? |
|
|
HEMOBILIA |
|
|
|
|
|
What is it? |
Blood draining via the common bile duct |
|
|
into the duodenum |
|
What is the diagnostic triad? |
Triad: |
|
|
1. |
RUQ pain |
|
2. |
Guaiac positive/upper GI bleeding |
|
3. |
Jaundice |
What are the causes? |
Trauma with liver laceration, percutaneous |
|
|
transhepatic cholangiography (PTC), tumors |
|

Chapter 53 / Portal Hypertension 357
How is the diagnosis made? EGD (blood out of the ampulla of Vater), A-gram
What is the treatment? A-gram with embolization of the bleeding vessel
C h a p t e r 53
Portal
Hypertension
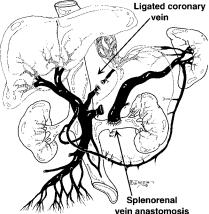
Identify the anatomy of the portal venous system:
1.Portal vein
2.Coronary vein
3.Splenic vein
4.IMV (inferior mesenteric vein)
5.SMV (superior mesenteric vein)
6.Superior hemorrhoidal vein
358 Section II / General Surgery
Describe drainage of blood from the superior hemorrhoidal vein.
Where does blood drain into from the IMV?
Where does the portal vein begin?
What are the (6) potential routes of portal–systemic collateral blood flow (as seen with portal hypertension)?
To the IMV, the splenic vein, and then the portal vein
Into the splenic vein
At the confluence of the splenic vein and the SMV
1.Umbilical vein
2.Coronary vein to esophageal venous plexuses
3.Retroperitoneal veins (veins of Retzius)
4.Diaphragm veins (veins of Sappey)
5.Superior hemorrhoidal vein to middle and inferior hemorrhoidal veins and then to the iliac vein
6.Splenic veins to the short gastric veins
What is the pathophysiology |
Elevated portal pressure resulting from |
of portal hypertension? |
resistance to portal flow |
What level of portal |
10 mm Hg |
pressure is normal? |
|
What is the etiology? |
Prehepatic—Thrombosis of portal vein/ |
|
atresia of portal vein |
|
Hepatic—Cirrhosis (distortion of |
|
normal parenchyma by regenerating |
|
hepatic nodules), hepatocellular |
|
carcinoma, fibrosis |
|
Posthepatic—Budd-Chiari syndrome: |
|
thrombosis of hepatic veins |
What is the most common |
Cirrhosis ( 90% of cases) |
cause of portal hypertension |
|
in the United States? |
|
How many patients with |
Surprisingly, 1 in 5 |
alcoholism develop |
|
cirrhosis? |
|

What percentage of patients with cirrhosis develop esophageal varices?
How many patients with cirrhosis develop portal hypertension?
What is the most common physical finding in patients with portal hypertension?
What are the associated CLINICAL findings in portal hypertension (4)?
Chapter 53 / Portal Hypertension 359
40%
Approximately two thirds
Splenomegaly (spleen enlargement)
1.Esophageal varices
2.Splenomegaly
3.Caput medusae (engorgement of periumbilical veins)
4.Hemorrhoids
Varices

 Splenomegaly
Splenomegaly
Caput medusae
Hemorrhoids
What other physical findings are associated with cirrhosis and portal hypertension?
What is the name of the periumbilical bruit heard with caput medusae?
Spider angioma, palmar erythema, ascites, truncal obesity and peripheral wasting, encephalopathy, asterixis (liver flap), gynecomastia, jaundice
Cruveilhier-Baumgarten bruit
360 Section II / General Surgery
What constitutes the portal– systemic collateral circulation in portal hypertension in the following conditions:
Esophageal varices?
Caput medusae?
Retroperitoneal varices?
Hemorrhoids?
Coronary vein backing up into the azygous system
Umbilical vein (via falciform ligament) draining into the epigastric veins
Small mesenteric veins (veins of Retzius) draining retroperitoneally into lumbar veins
Superior hemorrhoidal vein (which normally drains into the inferior mesenteric vein) backing up into the middle and inferior hemorrhoidal veins
What is the etiology? |
Cirrhosis (90%), schistosomiasis, |
|
hepatitis, Budd-Chiari syndrome, |
|
hemochromatosis, Wilson’s disease, |
|
portal vein thrombosis, tumors, splenic |
|
vein thrombosis |
What is the most common |
Schistosomiasis |
cause of portal hypertension |
|
outside North America? |
|
What is Budd-Chiari |
Thrombosis of the hepatic veins |
syndrome? |
|
What is the most feared |
Bleeding from esophageal varices |
complication of portal |
|
hypertension? |
|
What are esophageal |
Engorgement of the esophageal venous |
varices? |
plexuses secondary to increased collateral |
|
blood flow from the portal system as a |
|
result of portal hypertension |
What is the “rule of 2/3” of portal hypertension?
2/3 of patients with cirrhosis will develop portal hypertension
2/3 of patients with portal hypertension will develop esophageal varices
2/3 of patients with esophageal varices will bleed from the varices
In patients with cirrhosis and known varices who are suffering from upper GI bleeding, how often does that bleeding result from varices?
Chapter 53 / Portal Hypertension 361
Only 50% of the time
What are the signs/symptoms?
What is the mortality rate from an acute esophageal variceal bleed?
Hematemesis, melena, hematochezia
50%
What is the initial treatment of variceal bleeding?
As with all upper GI bleeding: large bore IVs 2, IV fluid, Foley catheter, type and cross blood, send labs, correct coagulopathy (vitamin K, fresh frozen plasma), / – intubation to protect from aspiration
What is the diagnostic test of choice?
EGD (upper GI endoscopy)
Remember, bleeding is the result of varices only half the time; must rule out ulcers, gastritis, etc.
If esophageal varices cause bleeding, what are the EGD treatment options?
1.Emergent endoscopic sclerotherapy: a sclerosing substance is injected into the esophageal varices under direct endoscopic vision
2.Endoscopic band ligation: elastic band ligation of varices
What are the pharmacologic options?
Somatostatin (Octreotide) or IV vasopressin (and nitroglycerin, to
avoid MI) to achieve vasoconstriction of the mesenteric vessels; if bleeding continues, consider balloon (Sengstaken-Blakemore tube) tamponade of the varices, -blocker
What is a SengstakenBlakemore tube?
What is the next therapy after the bleeding is controlled?
Tube with a gastric and esophageal balloon for tamponading an esophageal bleed (see page 268)
Repeat endoscopic sclerotherapy/banding
362 Section II / General Surgery |
|
What are the options |
Repeat sclerotherapy/banding and treat |
if sclerotherapy and |
conservatively |
conservative methods fail to |
TIPS |
stop the variceal bleeding or |
Surgical shunt (selective or partial) |
bleeding recurs? |
Liver transplantation |
What is a “selective” shunt? |
Shunt that selectively decompresses the |
|
varices without decompressing the portal |
|
vein |
What does the acronym |
Transjugular Intrahepatic Portosystemic |
TIPS stand for? |
Shunt |
What is a TIPS procedure? |
Angiographic radiologist places a small |
|
tube stent intrahepatically between the |
|
hepatic vein and a branch of the portal |
|
vein via a percutaneous jugular vein route |
What is a “partial shunt”?
What is a Warren shunt?
Shunt that directly decompresses the portal vein, but only partially
Distal splenorenal shunt with ligation of the coronary vein—elective shunt procedure associated with low incidence of encephalopathy in patients postoperatively because only the splenic flow is diverted to decompress the varices
What is a contraindication to the Warren “selective” shunt?
Define the following shunts: End-to-side portocaval shunt
Side-to-side portocaval shunt
Synthetic portocaval
H-graft
Chapter 53 / Portal Hypertension 363
Ascites
“Total shunt”—portal vein (end) to IVC (side)
Side of portal vein anastomosed to side of IVC—partially preserves portal flow (“partial shunt”)
“Partial shunt”—synthetic tube graft from the portal vein to the IVC
(good option for patients with alcoholism; associated with lower incidence
of encephalopathy and easier transplantation later)
Synthetic mesocaval |
Synthetic graft from the SMV to the IVC |
H-graft |
|
What is the most common perioperative cause of death following shunt procedure?
What is the major postoperative morbidity after a shunt procedure?
Hepatic failure, secondary to decreased blood flow (accounts for two thirds of deaths)
Increased incidence of hepatic encephalopathy because of decreased portal blood flow to the liver and decreased clearance of toxins/metabolites from the blood
What medication is infused |
Nitroglycerin IV drip |
to counteract the coronary |
|
artery vasoconstriction of IV |
|
vasopressin? |
|
What lab value roughly correlates with degree of encephalopathy?
What medications are used to treat hepatic encephalopathy?
Serum ammonia level (Note: Thought to correlate with but not cause encephalopathy)
Lactulose PO, with or without neomycin PO
