
- •Dedication
- •Editors and Contributors
- •Foreword
- •Preface
- •Contents
- •PREPARING FOR THE SURGERY CLERKSHIP
- •SURGICAL NOTES
- •COMMON ABBREVIATIONS YOU SHOULD KNOW
- •RETRACTORS (YOU WILL GET TO KNOW THEM WELL!)
- •SUTURE MATERIALS
- •WOUND CLOSURE
- •KNOTS AND EARS
- •INSTRUMENT TIE
- •TWO-HAND TIE
- •COMMON PROCEDURES
- •NASOGASTRIC TUBE (NGT) PROCEDURES
- •CHEST TUBES
- •NASOGASTRIC TUBES (NGT)
- •FOLEY CATHETER
- •CENTRAL LINES
- •MISCELLANEOUS
- •THIRD SPACING
- •COMMON IV REPLACEMENT FLUIDS (ALL VALUES ARE PER LITER)
- •CALCULATION OF MAINTENANCE FLUIDS
- •ELECTROLYTE IMBALANCES
- •ANTIBIOTICS
- •STEROIDS
- •HEPARIN
- •WARFARIN (COUMADIN®)
- •MISCELLANEOUS AGENTS
- •NARCOTICS
- •MISCELLANEOUS
- •ATELECTASIS
- •POSTOPERATIVE RESPIRATORY FAILURE
- •PULMONARY EMBOLISM
- •ASPIRATION PNEUMONIA
- •GASTROINTESTINAL COMPLICATIONS
- •ENDOCRINE COMPLICATIONS
- •CARDIOVASCULAR COMPLICATIONS
- •MISCELLANEOUS
- •HYPOVOLEMIC SHOCK
- •SEPTIC SHOCK
- •CARDIOGENIC SHOCK
- •NEUROGENIC SHOCK
- •MISCELLANEOUS
- •URINARY TRACT INFECTION (UTI)
- •CENTRAL LINE INFECTIONS
- •WOUND INFECTION (SURGICAL SITE INFECTION)
- •NECROTIZING FASCIITIS
- •CLOSTRIDIAL MYOSITIS
- •SUPPURATIVE HIDRADENITIS
- •PSEUDOMEMBRANOUS COLITIS
- •PROPHYLACTIC ANTIBIOTICS
- •PAROTITIS
- •MISCELLANEOUS
- •CHEST
- •ABDOMEN
- •MALIGNANT HYPERTHERMIA
- •MISCELLANEOUS
- •OVERVIEW
- •CHOLECYSTOKININ (CCK)
- •SECRETIN
- •GASTRIN
- •SOMATOSTATIN
- •MISCELLANEOUS
- •GROIN HERNIAS
- •HERNIA REVIEW QUESTIONS
- •ESOPHAGEAL HIATAL HERNIAS
- •PRIMARY SURVEY
- •SECONDARY SURVEY
- •TRAUMA STUDIES
- •PENETRATING NECK INJURIES
- •MISCELLANEOUS TRAUMA FACTS
- •PEPTIC ULCER DISEASE (PUD)
- •DUODENAL ULCERS
- •GASTRIC ULCERS
- •PERFORATED PEPTIC ULCER
- •TYPES OF SURGERIES
- •STRESS GASTRITIS
- •MALLORY-WEISS SYNDROME
- •ESOPHAGEAL VARICEAL BLEEDING
- •BOERHAAVE’S SYNDROME
- •ANATOMY
- •GASTRIC PHYSIOLOGY
- •GASTROESOPHAGEAL REFLUX DISEASE (GERD)
- •GASTRIC CANCER
- •GIST
- •MALTOMA
- •GASTRIC VOLVULUS
- •SMALL BOWEL
- •APPENDICITIS
- •CLASSIC INTRAOPERATIVE QUESTIONS
- •APPENDICEAL TUMORS
- •SPECIFIC TYPES OF FISTULAS
- •ANATOMY
- •COLORECTAL CARCINOMA
- •COLONIC AND RECTAL POLYPS
- •POLYPOSIS SYNDROMES
- •DIVERTICULAR DISEASE OF THE COLON
- •ANATOMY
- •ANAL CANCER
- •ANATOMY
- •TUMORS OF THE LIVER
- •ABSCESSES OF THE LIVER
- •HEMOBILIA
- •ANATOMY
- •PHYSIOLOGY
- •PATHOPHYSIOLOGY
- •DIAGNOSTIC STUDIES
- •BILIARY SURGERY
- •OBSTRUCTIVE JAUNDICE
- •CHOLELITHIASIS
- •ACUTE CHOLECYSTITIS
- •ACUTE ACALCULOUS CHOLECYSTITIS
- •CHOLANGITIS
- •SCLEROSING CHOLANGITIS
- •GALLSTONE ILEUS
- •CARCINOMA OF THE GALLBLADDER
- •CHOLANGIOCARCINOMA
- •MISCELLANEOUS CONDITIONS
- •PANCREATITIS
- •PANCREATIC ABSCESS
- •PANCREATIC NECROSIS
- •PANCREATIC PSEUDOCYST
- •PANCREATIC CARCINOMA
- •MISCELLANEOUS
- •ANATOMY OF THE BREAST AND AXILLA
- •BREAST CANCER
- •DCIS
- •LCIS
- •MISCELLANEOUS
- •MALE BREAST CANCER
- •BENIGN BREAST DISEASE
- •CYSTOSARCOMA PHYLLODES
- •FIBROADENOMA
- •FIBROCYSTIC DISEASE
- •MASTITIS
- •BREAST ABSCESS
- •MALE GYNECOMASTIA
- •ADRENAL GLAND
- •ADDISON’S DISEASE
- •INSULINOMA
- •GLUCAGONOMA
- •SOMATOSTATINOMA
- •ZOLLINGER-ELLISON SYNDROME (ZES)
- •MULTIPLE ENDOCRINE NEOPLASIA
- •THYROID DISEASE
- •ANATOMY
- •PHYSIOLOGY
- •HYPERPARATHYROIDISM (HPTH)
- •PARATHYROID CARCINOMA
- •SOFT TISSUE SARCOMAS
- •LYMPHOMA
- •SQUAMOUS CELL CARCINOMA
- •BASAL CELL CARCINOMA
- •MISCELLANEOUS SKIN LESIONS
- •STAGING
- •INTENSIVE CARE UNIT (ICU) BASICS
- •INTENSIVE CARE UNIT FORMULAS AND TERMS YOU SHOULD KNOW
- •SICU DRUGS
- •INTENSIVE CARE PHYSIOLOGY
- •HEMODYNAMIC MONITORING
- •MECHANICAL VENTILATION
- •PERIPHERAL VASCULAR DISEASE
- •LOWER EXTREMITY AMPUTATIONS
- •ACUTE ARTERIAL OCCLUSION
- •ABDOMINAL AORTIC ANEURYSMS
- •MESENTERIC ISCHEMIA
- •MEDIAN ARCUATE LIGAMENT SYNDROME
- •CAROTID VASCULAR DISEASE
- •CLASSIC CEA INTRAOP QUESTIONS
- •SUBCLAVIAN STEAL SYNDROME
- •RENAL ARTERY STENOSIS
- •SPLENIC ARTERY ANEURYSM
- •POPLITEAL ARTERY ANEURYSM
- •MISCELLANEOUS
- •PEDIATRIC IV FLUIDS AND NUTRITION
- •PEDIATRIC BLOOD VOLUMES
- •FETAL CIRCULATION
- •ECMO
- •NECK
- •ASPIRATED FOREIGN BODY (FB)
- •CHEST
- •PULMONARY SEQUESTRATION
- •ABDOMEN
- •INGUINAL HERNIA
- •UMBILICAL HERNIA
- •GERD
- •CONGENITAL PYLORIC STENOSIS
- •DUODENAL ATRESIA
- •MECONIUM ILEUS
- •MECONIUM PERITONITIS
- •MECONIUM PLUG SYNDROME
- •ANORECTAL MALFORMATIONS
- •HIRSCHSPRUNG’S DISEASE
- •MALROTATION AND MIDGUT VOLVULUS
- •OMPHALOCELE
- •GASTROSCHISIS
- •POWER REVIEW OF OMPHALOCELE AND GASTROSCHISIS
- •APPENDICITIS
- •INTUSSUSCEPTION
- •MECKEL’S DIVERTICULUM
- •NECROTIZING ENTEROCOLITIS
- •BILIARY TRACT
- •TUMORS
- •PEDIATRIC TRAUMA
- •OTHER PEDIATRIC SURGERY QUESTIONS
- •POWER REVIEW
- •WOUND HEALING
- •SKIN GRAFTS
- •FLAPS
- •SENSORY SUPPLY TO THE HAND
- •CARPAL TUNNEL SYNDROME
- •ANATOMY
- •MISCELLANEOUS
- •NOSE AND PARANASAL SINUSES
- •ORAL CAVITY AND PHARYNX
- •FACIAL FRACTURES
- •ENT WARD QUESTIONS
- •RAPID-FIRE REVIEW OF MOST COMMON CAUSES OF ENT INFECTIONS
- •THORACIC OUTLET SYNDROME (TOS)
- •CHEST WALL TUMORS
- •DISEASES OF THE PLEURA
- •DISEASES OF THE LUNGS
- •DISEASES OF THE MEDIASTINUM
- •DISEASES OF THE ESOPHAGUS
- •ACQUIRED HEART DISEASE
- •CONGENITAL HEART DISEASE
- •CARDIAC TUMORS
- •DISEASES OF THE GREAT VESSELS
- •MISCELLANEOUS
- •BASIC IMMUNOLOGY
- •CELLS
- •IMMUNOSUPPRESSION
- •OVERVIEW OF IMMUNOSUPPRESSION MECHANISMS
- •MATCHING OF DONOR AND RECIPIENT
- •REJECTION
- •ORGAN PRESERVATION
- •KIDNEY TRANSPLANT
- •LIVER TRANSPLANT
- •PANCREAS TRANSPLANT
- •HEART TRANSPLANT
- •INTESTINAL TRANSPLANTATION
- •LUNG TRANSPLANT
- •TRANSPLANT COMPLICATIONS
- •ORTHOPAEDIC TERMS
- •TRAUMA GENERAL PRINCIPLES
- •FRACTURES
- •ORTHOPAEDIC TRAUMA
- •DISLOCATIONS
- •THE KNEE
- •ACHILLES TENDON RUPTURE
- •ROTATOR CUFF
- •MISCELLANEOUS
- •ORTHOPAEDIC INFECTIONS
- •ORTHOPAEDIC TUMORS
- •ARTHRITIS
- •PEDIATRIC ORTHOPAEDICS
- •HEAD TRAUMA
- •SPINAL CORD TRAUMA
- •TUMORS
- •VASCULAR NEUROSURGERY
- •SPINE
- •PEDIATRIC NEUROSURGERY
- •SCROTAL ANATOMY
- •UROLOGIC DIFFERENTIAL DIAGNOSIS
- •RENAL CELL CARCINOMA (RCC)
- •BLADDER CANCER
- •PROSTATE CANCER
- •BENIGN PROSTATIC HYPERPLASIA
- •TESTICULAR CANCER
- •TESTICULAR TORSION
- •EPIDIDYMITIS
- •PRIAPISM
- •ERECTILE DYSFUNCTION
- •CALCULUS DISEASE
- •INCONTINENCE
- •URINARY TRACT INFECTION (UTI)
- •MISCELLANEOUS UROLOGY QUESTIONS
- •Rapid Fire Power Review
- •TOP 100 CLINICAL SURGICAL MICROVIGNETTES
- •Figure Credits
- •Index

Chapter 40 / Upper GI Bleeding 269
What is the problem with shunts?
Decreased portal pressure, but increased encephalopathy
BOERHAAVE’S SYNDROME
What is it? |
Postemetic esophageal rupture |
Who was Dr. Boerhaave? |
Dutch physician who first described the |
|
syndrome in the Dutch Grand Admiral |
|
Van Wassenaer in 1724 |
Why is the esophagus |
No serosa |
susceptible to perforation |
|
and more likely to break |
|
down an anastomosis? |
|
What is the most common |
Posterolateral aspect of the esophagus (on |
location? |
the left), 3 to 5 cm above the GE junction |
What is the cause of rupture? |
Increased intraluminal pressure, usually |
|
caused by violent retching and vomiting |
What is the associated risk |
Esophageal reflux disease (50%) |
factor? |
|
What are the symptoms? |
Pain postemesis (may radiate to the back, |
|
dysphagia) |
What are the signs? |
Left pneumothorax, Hamman’s sign, left |
|
pleural effusion, subcutaneous/mediastinal |
|
emphysema, fever, tachypnea, tachycardia, |
|
signs of infection by 24 hours, neck crepitus, |
|
widened mediastinum on CXR |
What is Mackler’s triad? |
1. Emesis |
|
2. Lower chest pain |
|
3. Cervical emphysema (subQ air) |
What is Hamman’s sign? |
“Mediastinal crunch or clicking” |
|
produced by the heart beating against |
|
air-filled tissues |
How is the diagnosis made? |
History, physical examination, CXR, |
|
esophagram with water-soluble contrast |
270 Section II / General Surgery
What is the treatment?
What is the mortality rate if less than 24 hours until surgery for perforated esophagus?
What is the mortality rate if more than 24 hours until surgery for perforated esophagus?
Overall, what is the most common cause of esophageal perforation?
Surgery within 24 hours to drain the mediastinum and surgically close the perforation and placement of pleural patch; broad-spectrum antibiotics
15%
33%
Iatrogenic (most commonly cervical esophagus)
C h a p t e r 41 |
Stomach |
|
ANATOMY |
|
|
|
|
|
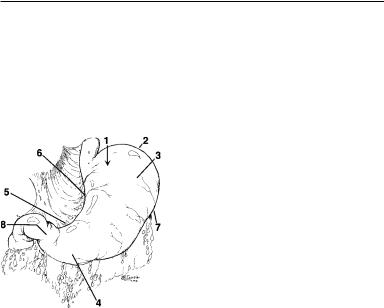
Identify the parts of the |
1. Cardia |
|
stomach: |
2. Fundus |
|
|
3. |
Body |
|
4. |
Antrum |
|
5. |
Incisura angularis |
|
6. |
Lesser curvature |
|
7. |
Greater curvature |
|
8. |
Pylorus |

Identify the blood supply to the stomach:
What space lies behind the stomach?
What is the opening into the lesser sac?
What are the folds of gastric mucosa called?
GASTRIC PHYSIOLOGY
Chapter 41 / Stomach 271
1.Left gastric artery
2.Right gastric artery
3.Right gastroepiploic artery
4.Left gastroepiploic artery
5.Short gastrics (from spleen)
Lesser sac; the pancreas lies behind the stomach
Foramen of Winslow
Rugae
Define the products of the following stomach cells:
Gastric parietal cells
Chief cells
Mucous neck cells
G cells
Where are G cells located?
What is pepsin?
What is intrinsic factor?
HCl
Intrinsic factor
PEPsinogen (Think: “a PEPpy chief”)
Bicarbonate
Mucus
Gastrin (Think: G cells Gastrin)
Antrum
Proteolytic enzyme that hydrolyzes peptide bonds
Protein secreted by the parietal cells that combines with vitamin B12 and allows for absorption in the terminal ileum

272 Section II / General Surgery
GASTROESOPHAGEAL REFLUX DISEASE (GERD)
What is it? |
Excessive reflux of gastric contents into |
|
the esophagus, “heartburn” |
What is pyrosis? |
Medical term for heartburn |
What are the causes? |
Decreased lower esophageal sphincter |
|
(LES) tone ( 50% of cases) |
|
Decreased esophageal motility to clear |
|
refluxed fluid |
|
Gastric outlet obstruction |
|
Hiatal hernia in 50% of patients |
What are the signs/ symptoms?
What disease must be ruled out when the symptoms of GERD are present?
What tests are included in the workup?
Heartburn, regurgitation, respiratory problems/pneumonia from aspiration of refluxed gastric contents; substernal pain
Coronary artery disease
EGD
UGI contrast study with esophagogram 24-hour acid analysis (pH probe in
esophagus) Manometry, EKG, CXR
What is the medical |
Small meals |
treatment? |
PPIs (proton-pump inhibitors) or |
|
H2 blockers |
|
Elevation of head at night and no meals |
|
prior to sleeping |
What are the indications for |
Intractability (failure of medical treatment) |
surgery? |
Respiratory problems as a result of reflux |
|
and aspiration of gastric contents (e.g., |
|
pneumonia) |
|
Severe esophageal injury (e.g., ulcers, |
|
hemorrhage, stricture, Barrett’s |
|
esophagus) |
What is Barrett’s esophagus? |
Columnar metaplasia from the normal |
|
squamous epithelium as a result of |
|
chronic irritation from reflux |

|
Chapter 41 / Stomach 273 |
What is the major concern |
Developing cancer |
with Barrett’s esophagus? |
|
What type of cancer devel- |
Adenocarcinoma |
ops in Barrett’s esophagus? |
|
What percentage of patients |
10% |
with GERD develops |
|
Barrett’s esophagus? |
|
What percentage of patients |
7% lifetime (5%–10%) |
with Barrett’s esophagus will |
|
develop adenocarcinoma? |
|
What is the treatment of |
Nonsurgical: endoscopic mucosal |
Barrett’s esophagus with |
resection and photodynamic therapy; |
dysplasia? |
other options include radiofrequency |
|
ablation, cryoablation (these methods |
|
are also often used for mucosal |
|
adenocarcinoma) |
Define the following |
|
surgical options for severe |
|
GERD: |
|
Lap Nissen |
360 fundoplication—2 cm long |
|
(laparoscopically) |
hrf
‘07

274 Section II / General Surgery |
|
Belsey mark IV |
240 to 270 fundoplication performed |
|
through a thoracic approach |
hr
f
‘07
Hill |
Arcuate ligament repair (close large |
|
esophageal hiatus) and gastropexy to |
|
diaphragm (suture stomach to diaphragm) |
7 0 ‘ f r h
