
- •Preface
- •Acknowledgements
- •Contents
- •The Team
- •The Instruments
- •Patient Positioning
- •Setup for Upper Abdominal Surgery
- •Setup for Lower Abdominal Surgery
- •The Working Environment
- •Appraisal of Surgical Instruments
- •Trocars
- •Other Instrumental Requirements
- •Troubleshooting Loss of Pneumoperitoneum
- •Principles of Hemostasis
- •Control of Bleeding of Unnamed Vessels
- •Control of Bleeding of a Main Named Vessel
- •Selected Further Reading
- •2 Cholecystectomy
- •Impacted Stone (Hydrops, Empyema, Early Mirizzi)
- •Adhesions Due to Previous Upper Midline Laparotomy
- •Selected Further Reading
- •Selected Further Reading
- •The Need for Specialized Equipment
- •Access to the Liver
- •Maneuvers Common to All Laparoscopic Liver Surgery
- •Resection of Liver Tumors
- •Limited Resection of Minor Lesions
- •Left Lateral Segmentectomy
- •Right Hepatectomy
- •Patient Selection
- •Principles of Surgical Therapy in the Management of Gastroesophageal Reflux Disease
- •Patient Positioning
- •Technique
- •Postoperative Course
- •Management of Complications
- •Paraesophageal Hernia
- •Esophageal Myotomy for Achalasia
- •Vagotomies
- •Bilateral Truncal Vagotomy
- •Highly Selective Vagotomy
- •Lesser Curvature Seromyotomy and Posterior Truncal Vagotomy
- •Selected Further Reading
- •Pyloroplasty
- •Vagotomy with Antrectomy or any Distal Gastrectomy
- •Port Placement
- •Technique
- •Locating the Perforation
- •Abdominal Washout
- •Closure of the Perforation with an Omental Patch
- •Postoperative Course
- •Selected Further Reading
- •7 Appendectomy
- •OR Setup and Port Placement
- •Technique
- •Gangrenous or Perforated Appendicitis
- •Laparoscopic Assisted Appendectomy
- •Left Hemicolectomy
- •Reversing the Hartmann Procedure
- •Selected Further Reading
- •Selected Further Reading
- •Transabdominal Preperitoneal Repair (TAPP)
- •Patient and Port Positioning
- •Dissection of the Preperitoneal Space
- •Dissection of the Cord Structures and the Vas Deferens
- •Placement of the Mesh and Fixation
- •Closure of the Peritoneum
- •Indications
- •Technique
- •Positioning
- •Pneumoperitoneum
- •Port Placement
- •Adhesiolysis
- •Measurement of the Hernia Defect
- •Placement of Mesh
- •Difficult Ventral or Incisional Hernias
- •Pain Following Laparoscopic Ventral or Incisional Hernia Repair
- •Preoperative Requirements and Workup
- •Patient Positioning
- •Port Placement
- •Surgical Anatomy
- •Surgical Principles
- •Technique
- •Division of the Short Gastric Vessels and Exposure of the Tail of the Pancreas
- •Division of the Hilar Vessels and Phrenic Attachments
- •Extraction of the Spleen in a Bag
- •Final Steps of the Procedure
- •Control of an Unnamed Vessel
- •Control of a Major Vessel
- •Splenic Injury
- •Maneuver of Last Resort During Bleeding of the Hilar Vessels
- •Distal Splenopancreatectomy
- •Selected Further Reading
- •13 Adrenalectomy
- •Principles
- •Patient Positioning
- •Technique
- •Immediate Postoperative Complications
- •Late Postoperative Complications
- •Laparoscopic Adjustable Band
- •Technique
- •Complications
- •Laparoscopic Sleeve Gastrectomy
- •Selected Further Reading
- •Laparoscopic Cholecystectomy
- •Laparoscopic Appendectomy
- •Laparoscopic Inguinal Hernia Repair
- •Selected Further Reading
- •Monitors
- •OR Table
- •Trocar Placement and Triangulation
- •Equipment
- •Needle Holders
- •Graspers
- •Suture Material
- •Intracorporeal Knot-Tying
- •Interrupted Stitch
- •Running Stitch
- •Pirouette
- •Extracorporeal Knot-Tying
- •Roeder’s Knot
- •Endoloop
- •Troubleshooting
- •Lost Needle
- •Short Suture
- •Subject Index
Laparoscopic Adjustable Band |
239 |
Anastomotic Ulcers. Anastomotic ulcers are usually secondary to a pouch larger than 30 cm3 with increased acid secretion, a gastro-gastric fistula are found in a patient who continues to smoke postoperatively. In most cases, ulcers can be treated with proton pump inhibitors and cessation of smoking; however, if the ulcer results in perforation, the patient needs to be taken to the operating room. A Graham’s patch with or without closure of the hole is the treatment of choice. If the symptoms persist, another option is to redo the anastomosis after the inflammation has subsided.
Stricture. Constant vomiting and intolerance to food, more commonly than dumping syndrome, is due to stricture at the gastrojejunostomy. It usually manifests itself at the end of the second postoperative month. A postoperative stricture is normally diagnosed with endoscopy revealing an anastomosis less than 8 mm in diameter; this can often be treated with a single dilatation to a diameter of 1.5 cm, although a second dilatation is occasionally needed. In our experience, once we added an additional 7–8 mm to the diameter of the anastomosis by starting the gastojenostomy 1 cm above the inferolateral corner of the pouch, no strictures have been seen (Fig. 14.23).
OR Set Up
The patient can be placed in either the supine or lithotomy position. The benefit of the supine position is a faster set up and decreased risk of pressure on the thighs from the buttock holders. If the patient is placed in lithotomy position, the OR set up is exactly as for the Nissen procedure with one monitor above the patient’s head and one on the left side of the patient.
Technique
We use a five-trocar technique for the lap band (Fig.14.37).The trocar placement is the same as in the fundoplication. The first step is retraction of the left lobe of the liver. In the case of a very large accessory left hepatic artery barring the pars flaccida, it is possible to dissect the artery on either side to avoid ligating it. In the case of an artery that blocks access to the hiatus, it is possible to clamp the artery and monitor the effect on the liver. If there is no ischemia, the artery can be divided. The avascular aspect of the pars flacida is opened lateral to the nerve of Latarjet (Fig. 14.38). The membrane lying over the medial edge right crus is opened very low, near the crural decussation (Fig. 14.39), and by gently using a grasper from left to right, a small window is created under the esophagus and below the left crus (Fig. 14.40). We do not like to insert instruments blindly behind the esophagus, as is commonly performed rather, we prefer to see this window created under direct vision to avoid injury to the esophagus. The angle of His is opened using the harmonic shears. A special dissector is placed in this window (Fig.14.41).At this point,a fifteen millimeter trocar allows the insertion of the Realize Band (Ethicon Endo-Surgery Inc, Cincinatti, OH) (Fig. 14.42). The knotted thread is placed in the special dissector, and this permits the band to be pulled behind the esophagus and closed just under the decussation (14.43).All these cases are done using the pars flaccida technique to minimize slippage.Once the band is closed making sure that the buckle is facing toward the liver and the angulation is ideal at 45 degrees towards the left (Fig. 14.44), the stomach is used to imbricate the band to further minimize the slippage.
Laparoscopic
Adjustable
Band

240 |
Chapter 14 Bariatric Surgery |
S
CA
|
10E |
|
5 |
|
5 |
|
15 |
||
|
D |
|||
A |
10 |
B |
||
FA |
||||
|
||||
|
C |
|
||
|
|
|
Fig. 14.37 Trocar position for lap band surgery. C camera; A left hand of surgeon; B right hand of surgeon and site of introduction of the port (15 mm); D assistant’s grasper; E liver retractor. S surgeon; CA camera assistant; FA first assistant
Left margin of stomach
under fat layer
Caudate lobe of liver under pars accida
Fig. 14.38 Opening the avascular aspet of the pars flaccida (“Pars Flaccida” technique)
Laparoscopic Adjustable Band |
241 |
Rt. crus under lateral fat of stomach
Caudate lobe
Fig. 14.39 Incision of the peritoneal layer over the right crus of the diaphragm
Rt. crus
L. crus
Fig. 14.40 Dissection and creation of the retroesophageal tunnel under the left crus, near the
decussation of the crura

242 |
Chapter 14 Bariatric Surgery |
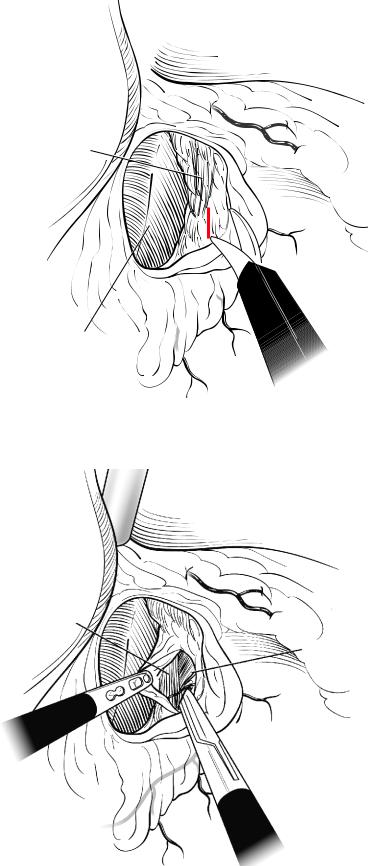
Fig. 14.41 The Goldfinger dissector is passed through the retroesophageal tunnel
Fig. 14.42 Passage of the band in the retroesophageal tunnel

Laparoscopic Adjustable Band |
243 |
Fig. 14.43 Band placed according to the “Pars Flaccida” technique
Fig. 14.44 The band is closed and the buckle is placed towards the caudate lobe of the liver, thus leaving the inflated chamber on the gastric wall
