
Книги по МРТ КТ на английском языке / Neuro Imaging Redcases
.pdf
188 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
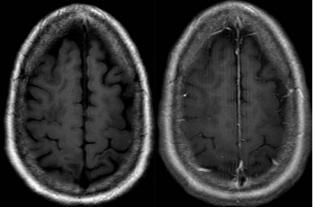
A  B
B  C
C 
 D
D
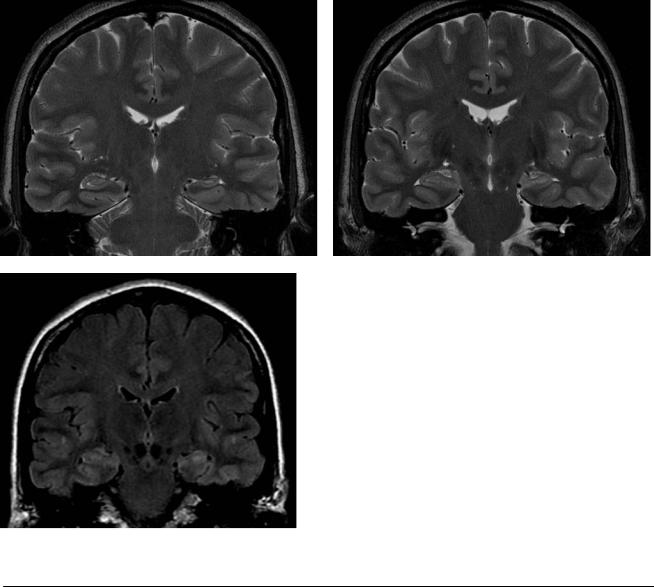
(A)Axial computed tomography (CT) at the level of the pons shows dilatation of the 4th ventricle (asterisk). Note the prominence of the left temporal horn.
(B)At the level of the midbrain, a large aqueduct (black arrow) and splaying of the hypothalamic structures (white arrows) are demonstrated. (C) There is fusiform dilatation of the 3rd ventricle (asterisk) and a round configuration of the frontal and occipital horns (white arrows). Note the small size of the sylvian fissures relative to the enlarged ventricles. (D) At the level of the corona radiata, there is only minimal sulcal enlargement (arrow).
■ Di erential Diagnosis
•Normal-pressure hydrocephalus (NPH): This is one of the few treatable causes of dementia. There is dilatation of the entire ventricular system without commensurate sulcal dilatation.
•Di use cerebral atrophy: This is associated with volume loss of the cortex and white matter, resulting in enlargement of the ventricles and sulci. The 3rd ventricle is usually not dilated, and there is no splaying of the hypothalamic structures.
•Obstructive hydrocephalus: This is indicated by dilatation of the ventricular system above the level of an intraor extraventricular lesion. The obstruction is proximal to the 4th ventricular outlets.
■Essential Facts
•Clinical findings of NPH include gait di culty, cognitive decline, incontinence of urine, and enlarged ventricles.
•Hydrocephalus is not secondary to such conditions as head trauma, intracerebral hemorrhage, and meningitis.
•CT and magnetic resonance imaging show ventriculomegaly with minimal or no sulcal enlargement and minimal or absent periventricular increased signal on T2-weighted images, indicating a chronic process.
¸Pearls & ˚ Pitfalls
¸Since it was first described, the definition of NPH has
been expanded. Initially, it was considered to be idiopathic; at present, any form of chronic communicating hydrocephalus and even a few noncommunicating forms, such as aqueductal stenosis, are included.
˚All the cardinal features of NPH (gait di culty, cognitive decline, incontinence of urine, and enlarged ventricles) are common in the elderly and have many causes.
189
Case 95
A
■ Clinical Presentation
A patient who has a history of lung cancer treated with chemotherapy now presents with headache and altered mentation.
Further Work-up
B  C
C 
 D
D
190 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
A  B
B 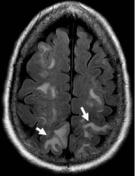 C
C 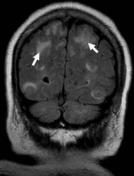
 D
D
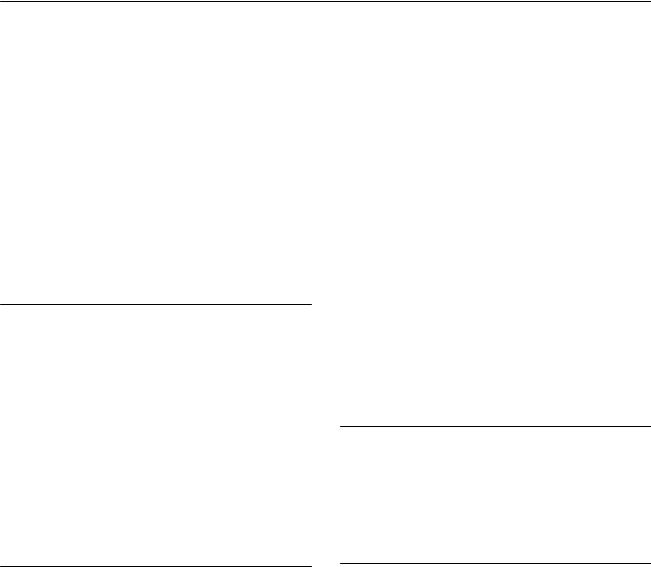
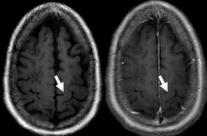
(A) Axial computed tomography (CT) of the brain shows areas of low attenuation in the subcortical white matter of both parietal lobes, without mass e ect (arrows). (B) Axial fluid-attenuated inversion recovery (FLAIR) image demonstrates vasogenic edema in the frontal and parietal subcortical white matter bilaterally (arrows). (C) Coronal FLAIR image demonstrates vasogenic edema in the frontal and parietal subcortical white matter bilaterally (arrows).
(D) Axial T1-weighted images (WIs) before and after gadolinium injection fail to demonstrate contrast enhancement (arrows).
■ Di erential Diagnosis
•Posterior reversible encephalopathy syndrome (PRES):
Vasogenic edema is seen in the subcortical white mater of both parietal and occipital regions. There is no abnormal enhancement or significant mass e ect.
•Watershed cerebral infarctions: Cytotoxic edema would be evident on the di usion-WIs. Watershed infarcts involve the deep white matter in a “rosary of pearls” pattern, or the cortex at the junction of the anterior and middle cerebral artery territories or the middle and posterior cerebral artery territories.
•Brain metastasis: Vasogenic edema is caused by multiple focal enhancing lesions. There is no predilection for watershed zones.
•Focal/patchy areas of edema may also be seen in the basal ganglia, brainstem, and deep white matter (external/internal capsules).
•The edema usually reverses completely.
•Hemorrhage (focal hematoma, isolated sulcal/subarachnoid blood or protein) is seen in ~15% of patients.
■ Other Imaging Findings
•At catheter angiography and MR angiography, di use vasoconstriction, focal vasoconstriction, vasodilatation, and even a string-of-beads appearance have been noted in PRES, consistent with what is typically described as vasospasm or arteritis.
■ Essential Facts
•PRES is the result of neurotoxicity-induced vasogenic edema.
•Associated conditions:
•Toxemia of pregnancy (preeclampsia/eclampsia)
•After transplant
•Immunosuppression (cyclosporine, tacrolimus)
•Infection, sepsis, shock
•Autoimmune diseases
•After cancer chemotherapy
•Other conditions: dialysis/erythropoietin, triple-H (hypertensive, hypervolemic, hemodilution) therapy
•On CT/magnetic resonance (MR) imaging, the brain typically demonstrates symmetric focal regions of hemispheric edema, more commonly involving the parietal and occipital lobes, followed by the frontal lobes, the inferior temporal-occipital junction, and the cerebellum.
¸Pearls & ˚ Pitfalls
¸Three di erent hemispheric patterns may be encoun-
tered with similar frequency:
¸Holohemispheric
¸Superior frontal sulcal
¸Primary parietal-occipital
¸These likely represent areas of watershed blood supply from the middle, anterior, and posterior cerebral arteries.
˚Focal areas of restricted di usion (likely representing infarction or tissue injury with cytotoxic edema) are uncommon (11–26%) and may be associated with an adverse outcome.

191
Case 96
A 
 B
B
C 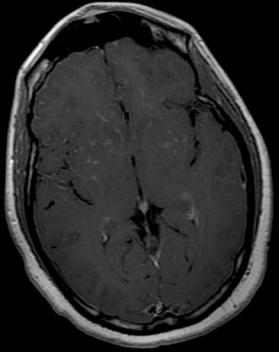
 D
D
■ Clinical Presentation
A 43-year-old African-American man with a chronic lung condition presenting with the new onset of seizures.
192 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
A B C D
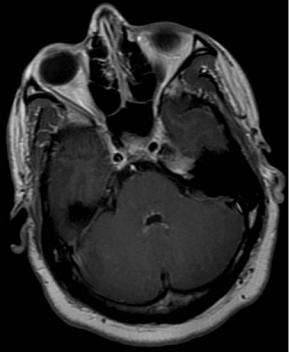
(A) Sagittal T1-weighted images (WIs) before and after contrast demonstrate extensive linear leptomeningeal enhancement in the thoracic region (white arrows). (B) Nodular enhancement around the 4th ventricle is demonstrated in the postcontrast axial T1WI (arrowheads). (C) Postcontrast axial T1WI shows the distribution of linear and nodular areas of enhancement in the basal ganglia following the Virchow-Robin spaces (arrows), which is indicative of leptomeningeal involvement. (D) On a postcontrast axial T1WI, leptomeningeal enhancement is also noted in the frontal convexities (arrows).
■ Di erential Diagnosis
•Leptomeningeal neurosarcoidosis: Sarcoidosis is a diagnosis of exclusion. It is characterized by nodular or linear enhancement of the cortical sulci, perivascular spaces, and cisterns around the base of the brain.
•Leptomeningeal carcinomatosis: Di use seeding of the leptomeninges by tumor metastases is known as denominated leptomeningeal carcinomatosis or leptomeningeal disease. It is commonly found in breast carcinoma, lung carcinoma, and melanoma in adults, and in hematogenous malignancies and primitive neuroectodermal tumor in children.
•Tuberculous meningitis: In countries with a high incidence of tuberculosis, tuberculous meningitis is typically a disease of young children that develops 3 to 6 months after primary infection. In countries with a low incidence of tuberculosis, tuberculous meningitis commonly a ects adults and frequently arises after the reactivation of a dormant subcortical or meningeal focus. Imaging findings include dural thickening, calcifications, meningeal enhancement (predominantly basal), infarcts, and communicating hydrocephalus.
■Essential Facts
•Sarcoidosis is an idiopathic systemic disease histologically characterized by the formation of noncaseating granulomas.
•The clinical presentation includes cranial neuropathy (especially of the optic and facial nerves) and neuroendocrine disorders (e.g., secondary diabetes insipidus); it is symptomatic in fewer than 10% of patients.
•Leptomeningeal enhancement is predominantly basal.
•Small enhancing nodules are seen on the surface of the brain and in the perivascular spaces.
•Di use dural thickening or a focal dural mass shows homogeneous contrast enhancement. These lesions are commonly dark on T2WIs.
•Spinal neurosarcoidosis may a ect the cord and nerve roots, the intradural-extramedullary space, the intracana- licular-extradural space, and the vertebral bodies and intervertebral disks.
•Leptomeningeal involvement manifests as thin linear leptomeningeal enhancement or small nodules.
■ Other Imaging Findings
•Magnetic resonance imaging:
•Periventricular and deep white matter T2 hyperintensities
•Multiple or solitary parenchymal masses with a ringlike appearance; enhancement when biologically active
•Chiasmatic lesions visualized as foci of increased signal intensity on fluid-attenuated inversion recovery images
•Loss of high T1 signal in the neurohypophysis
•Intramedullary sarcoidosis: nonspecific appearance; fusiform enlargement of the spinal cord in the cervical or upper thoracic levels; high T2 signal, low T1 signal, and patchy enhancement after contrast administration
¸Pearls & ˚ Pitfalls
¸Leptomeningeal sarcoidosis can be distinguished from
dural disease by involvement of the cortical sulci, perivascular spaces, cranial nerves, and cisterns around the base of the brain.
¸ Sarcoidosis is a diagnosis of exclusion.
˚Enhancing parenchymal lesions contiguous with enhancing meningeal areas may be mistaken for a meningioma.
193
Case 97
A B
C
■ Clinical Presentation
A 25-year-old with epilepsy.
194 |
RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
|
A |
B |
|
C |
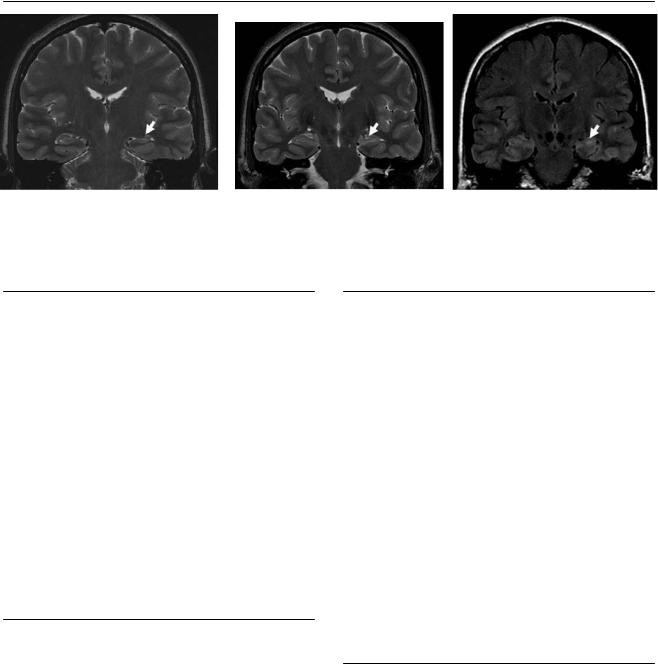
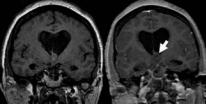
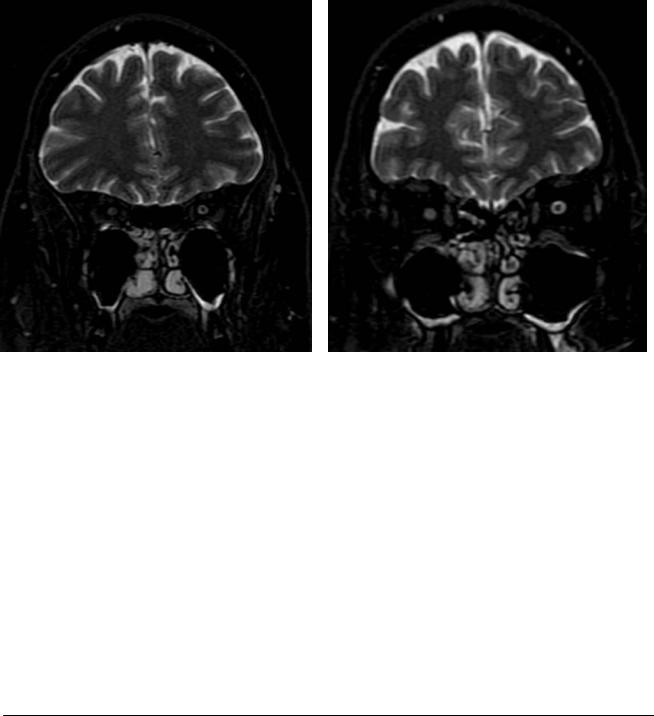
(A,B) Coronal T2-weighted images (WIs) perpendicular to the long axis of the hippocampus show decreased height of the left hippocampus in comparison with the right and mild architectural distortion (arrows). (C) Fluid-attenuated inversion recovery coronal image at the level of the hippocampal head shows increased signal on the left in comparison with the right and with the remainder of the temporal cortex (arrow).
■ Di erential Diagnosis
•Mesial temporal sclerosis (MTS): Atrophy of one or both hippocampal formations is indicative of MTS. There is increased T2 signal and architectural distortion. The abnormalities may involve other areas of the temporal lobe.
•Herpes encephalitis: This is the most common type of sporadic viral encephalitis, with a predilection for the temporal lobes. Magnetic resonance imaging (MRI) shows T2 hyperintensity corresponding to edematous changes in the temporal lobes, inferior frontal lobes, and insula, with a predilection for the medial temporal lobes. Foci of hemorrhage occasionally can be observed on MRI.
•Cortical dysplasia: This is defined as a focal abnormal arrangement of neurons and glia in the cortex. Images show distortion in the gray–white matter junction with thickening of the cortex. Mild T2 hyperintensity of the gray matter (cortex) is present. The temporal lobe is most frequently involved, followed by the frontal and occipital lobes.
■Essential Facts
•MTS is the most frequently observed abnormality in temporal lobe epilepsy (TLE).
•Neuronal loss and gliosis, involving principally the hippocampus and/or the amygdala and occasionally extending to other mesial temporal structures (entorhinal cortex and parahippocampal gyrus) or even throughout the temporal lobe, is common.
•Whether MTS is the cause or result of TLE is controversial.
•Patients with TLE often have a history of an initial precipitating injury, usually before the age of 5 years.
•Status epilepticus, especially complicated febrile convulsions, have been associated with hippocampal damage and unilateral sclerosis.
■ Other Imaging Findings
•MRI:
•Thin (1–3 mm) oblique coronal images orthogonal to the long axis of the hippocampus are required.
•Findings include hippocampal atrophy, increased signal on T2WIs, loss of internal structure, and decreased signal on T1WIs.
•Additional abnormalities include loss of hippocampal head digitations, enlarged temporal horn, and increased T2 signal in the ipsilateral anterior temporal lobe. The a ected hippocampus shows architectural distortion. MTS can also present with atrophy of the ipsilateral amygdala or asymmetry of the fornix.
•Ictal single-photon emission computed tomography (SPECT), with the use of tracers that accumulate and remain “fixed” in di erent areas of the brain proportional to the regional cerebral blood flow at the time of injection, is an important tool for localizing seizures in a presurgical evaluation.
•Interictal SPECT in focal epilepsy has shown areas of low perfusion in some patients, mainly those with TLE.
¸Pearls & ˚ Pitfalls
¸In 15 to 20% of cases of MTS, another potentially epilep-
togenic anomaly is found outside the hippocampus (dual pathology).
¸The most common types of lesions outside the hippocampus are developmental abnormalities, such as cortical dysgenesis and gliotic lesions acquired in early
childhood.
˚Dilatation of the ipsilateral temporal horn is found to be associated with hippocampal atrophy. Sometimes, temporal horn dilatation is more severe on the side opposite the sclerotic hippocampus. This may be a falsely lateralizing finding.

195
Case 98
A
■ Clinical Presentation
A 39-year-old woman with intermittent positional headache.
Further Work-up
B C
D
196 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
A 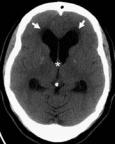 B
B  C
C 
 D
D
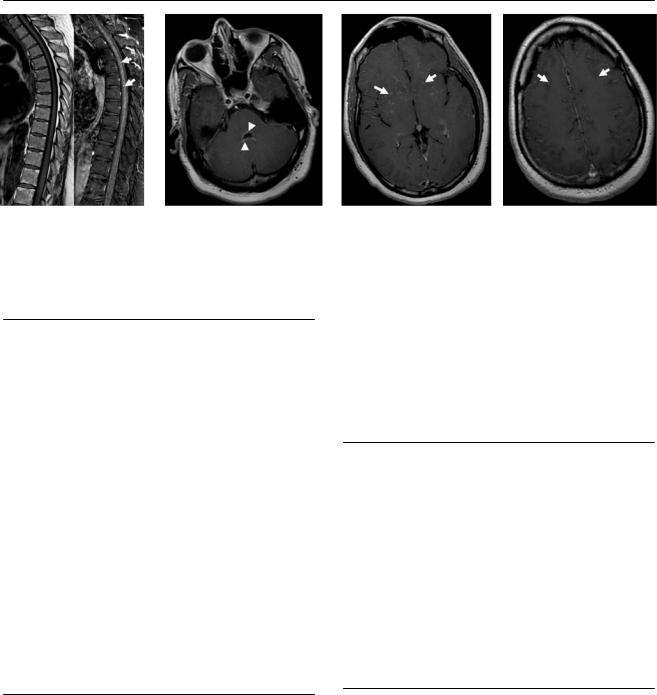
(A) Axial computed tomography (CT) demonstrates enlarged frontal horns and transependymal fluid leak (white arrows), which is indicative of hydrocephalus. There is a mass with attenuation similar to that of white matter in the vicinity of the foramen of Monro (asterisk). (B) Coronal T2-weighted image (WI) shows a mass in the superior aspect of the 3rd ventricle (arrow), with a central intermediate signal and a thin rim of low signal. (C) On the sagittal T1WI, the lesion has increased signal intensity (arrow). The lateral ventricles are dilated, whereas the 3rd and 4th are not. (D) Coronal T1WIs before and after contrast show no enhancement of the mass (arrow).
■ Di erential Diagnosis
•Colloid cyst of the 3rd ventricle: Remnants of Rathke cleft forming a well-defined round mass in the vicinity of the foramen of Monro are indicative of this diagnosis. Obstructive hydrocephalus is common. There is no enhancement after gadolinium injection.
•Central neurocytoma: This is a relatively benign tumor arising from neuronal precursor elements. Imaging studies show a well-defined, lobulated intraventricular mass growing near the foramen of Monro or septum pellucidum. There is mild to moderate enhancement. Calcifications and cystic changes are common. Most patients are young adults and can present with symptoms of ventricular obstruction.
•Intraventricular hemorrhage: Intraventricular clots may be found in the dependant portion of the ventricle or attached to the ventricular walls. The signal intensity may vary depending on the age of the blood products they contain.
■ Other Imaging Findings
•On CT scans, the lesions are often hyperdense.
•A thin rim of enhancement after the administration of iodinated contrast material is thought to represent the cyst capsule.
•The magnetic resonance imaging appearance is variable.
¸Pearls & ˚ Pitfalls
¸Because of the attachment of the cyst to the 3rd ven-
tricular roof, the lesion may be pendulous, resulting in intermittent foraminal obstruction.
˚ Rarely, colloid cysts may present with rim enhancement.
■ Essential Facts
•Colloid cysts are rare intracranial lesions.
•Clinical symptoms may be intermittent, self-resolving, and nonspecific.
•Headache is often the presenting symptom. It is described as brief (lasting seconds to minutes) and is initiated, exacerbated, or relieved by a change in position.
•Some colloid cysts result in the acute onset of hydrocephalus and may lead to sudden death.
•A round or oval mass is present in the anterior aspect of the 3rd ventricle.
•Treatment options include simple shunting of both lateral ventricles, open surgical removal, and percutaneous aspiration (simple cyst aspiration, stereotactic aspiration, endoscopic procedure).
197
Case 99
A B
C 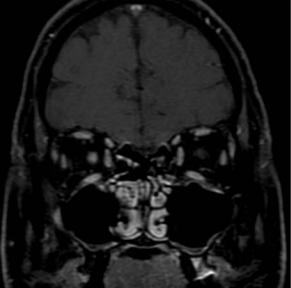
 D
D
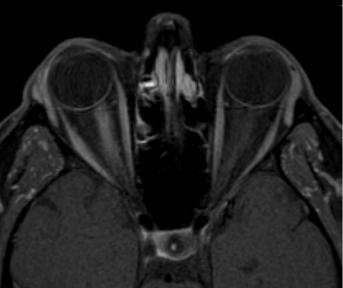
■ Clinical Presentation
A 42-year-old woman presenting with unilateral pain, decreased visual acuity, and loss of color vision.
