
Книги по МРТ КТ на английском языке / Neuro Imaging Redcases
.pdf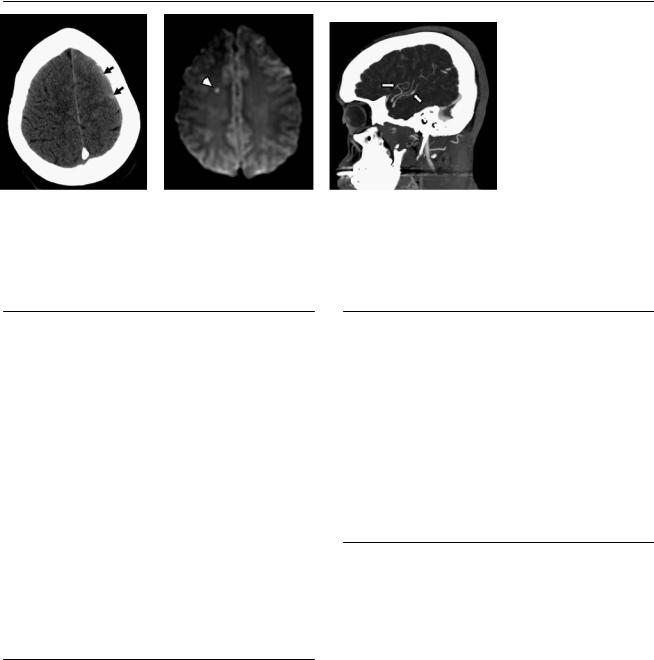
118 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
A B C 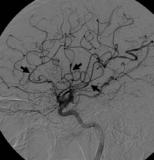 D
D
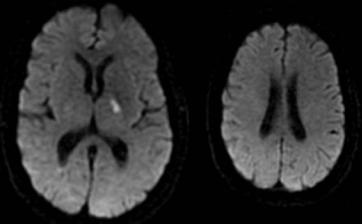
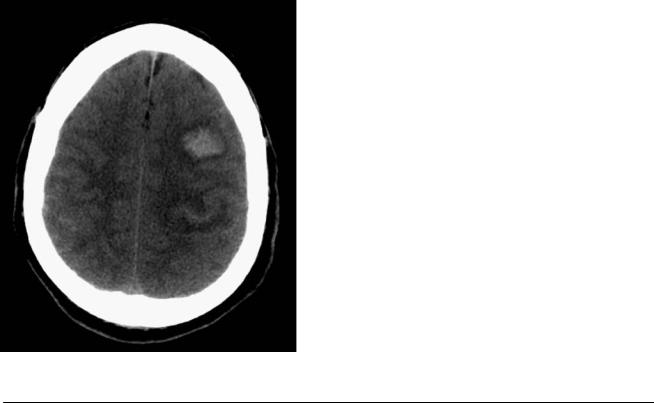
(A) Nonenhanced computed tomography (CT) of the brain demonstrates subarachnoid hemorrhage in the left frontal convexity (arrows). (B) Di usionweighted image shows a tiny focus of acute ischemia in the right centrum semiovale (arrowhead). Fluid-attenuated inversion recovery images (not shown) confirmed subarachnoid hemorrhage in the left convexity. (C) CT angiography, sagittal maximum-intensity-projection image, reveals a beaded appearance of some of the left middle cerebral artery (MCA) branches. (D) Lateral projection of a digital subtraction angiogram of the left internal carotid artery (ICA) shows multiple areas in the anterior cerebral artery and MCA branches with alternating segments of narrowing and dilatation (i.e., beading; arrows).
■ Di erential Diagnosis
•Central nervous system vasculitis: This is characterized by inflammation and necrosis of blood vessel walls. Causes can be infectious or noninfectious. The condition can be attributed to immune complex deposition (polyarteri-
tis nodosa, hypersensitivity vasculitis, collagen vascular disease) and can also be cell-mediated, as in giant cell arteritis (temporal arteritis, Takayasu arteritis, and granulomatous arteritis) or Wegener granulomatosis. Other causes include drug abuse, Kawasaki disease, neoplastic angiitis, and sarcoidosis.
•Fibromuscular dysplasia: Fibromuscular dysplasia is a nonatherosclerotic, noninflammatory arterial disease. It most commonly involves the renal and carotid arteries. Multifocal concentric luminal narrowing alternates with areas of mural dilatation (“string of beads”).
•Intracranial atherosclerosis: Although the angiographic
findings may be similar, multiple intracranial stenoses in a young patient are unlikely to be the result of atherosclerosis.
■Essential Facts
•Central nervous system vasculitis is a cause of stroke in young people.
•It may present with intracerebral or subarachnoid hemorrhage.
•Multiple infarcts of various ages are present in more than one vascular territory.
•Large-vessel vasculitis a ects the ICA, the M1 and A1 segments, the intracranial vertebral artery, the basilar artery, and the P1 segment. It may present after varicella-zoster virus infection or bacterial meningitis.
•Medium-vessel vasculitis occurs in panarteritis nodosa, lupus erythematosus, Behçet disease, Crohn disease, and Sneddon syndrome.
•Small-vessel vasculitis occurs in leukocytoclastic vasculitis.
■ Other Imaging Findings
•Angiography reveals one or multiple stenoses of brain vessels and abnormal straightening and kinking of arteries caused by vessel wall induration and multiple microaneurysms.
•Contrast enhancement of the vessel wall has been described.
•Conventional angiography is the gold standard.
•Brain biopsy may be necessary for the diagnosis.
•High-resolution magnetic resonance (MR) imaging of the skull base with contrast enhancement may demonstrate vessel wall thickening.
¸Pearls & ˚ Pitfalls
¸MR angiography (MRA) may demonstrate irregularity of
the intracranial vessels in the three-dimensional reconstructions when there is motion artifact. Careful review of the source images helps to determine if the MRA is of diagnostic quality.
˚Intracranial MRA may suggest complete occlusion of vessels with severe stenosis and decreased flow.
119
Case 60
A
■ Clinical Presentation
A 17-year-old girl who fainted while playing basketball.
Further Work-up
B C D
120 |
RadCases.thieme.com |
|
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
|
|
A |
B |
C |
|
D |
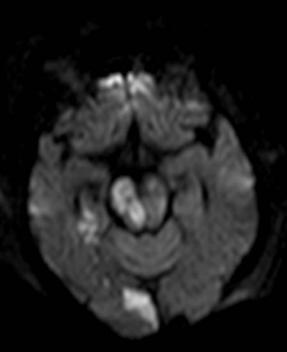
(A) Di usion-weighted image demonstrates acute ischemic changes in the left caudate head and putamen (arrow). (B) Sagittal computed tomography angiography maximum-intensity-projection images of the bifurcations of both carotid arteries demonstrate long-segment narrowing of the left internal carotid artery (ICA) with a serrated contour (arrows). (C) Lateral projection of a digital subtraction angiogram of the left ICA shows a “string of beads” appearance in the cervical segment (arrows). (D) Intracranial views of the same injection show a linear filling defect in the proximal left middle cerebral artery, consistent with a dissection flap (arrow). Irregular filling defects in the distal carotid artery and anterior cerebral artery are also noted, which represent thrombi.
■ Di erential Diagnosis
•Fibromuscular dysplasia (FMD): FMD is an infrequent cause of stroke in young people. It is characterized by a multifocal concentric luminal narrowing alternating with areas of mural dilatation that are wider than the original lumen. It may be associated with arterial dissection.
•Atherosclerotic narrowing: This frequently involves the carotid bifurcation and carotid siphons. Long-segment stenosis is infrequent. It is not usually seen in young patients.
•Mechanically induced vasospasm: This is a mechanically induced contraction of smooth-muscle fibers in the wall of a vessel. It is a common adverse event that may complicate an endovascular procedure by limiting distal blood flow. It has a “standing waves” appearance that mimics FMD. This is a transient phenomenon that usually resolves after withdrawal of the o ending catheter.
■ Essential Facts
•FMD is a nonatherosclerotic, noninflammatory arterial disease that most commonly involves the renal and carotid arteries.
•Cervicocranial FMD is often asymptomatic and can manifest with transient ischemic attack, amaurosis fugax, stroke, or nonspecific symptoms such as headache and tinnitus.
•FMD may be associated with arterial dissection, intracranial aneurysms, and arteriovenous fistulas.
■ Other Imaging Findings
•Angiography reveals multifocal concentric luminal narrowing alternating with areas of mural dilatation that are wider than the original lumen (“string of beads”), focal or tubular stenosis, a septum, or a diverticulum.
•Computed tomography angiography and magnetic resonance angiography (MRA) are e ective for detecting lesions of the middle and distal portions of the carotid and vertebral arteries and may also document or rule out the association of intracranial aneurysms.
¸Pearls & ˚ Pitfalls
¸Unlike atherosclerotic stenoses, stenoses arising from
FMD rarely a ect the ostial or proximal segments of arteries.
¸Spontaneous cervical artery dissections are a common cause of stroke in young and middle-aged adults and are
associated with FMD in ~15% of cases.
˚On time-of-flight MRA, artifacts caused by patient motion and swallowing or related to in-plane flow and susceptibility gradients may mimic the appearance of FMD and tend to decrease both the sensitivity and specificity of this modality for the detection of cervicocephalic FMD.

121
Case 61
A 
 B
B
■ Clinical Presentation
A 70-year-old woman presenting with syncope after a fall.
Further Work-up
C 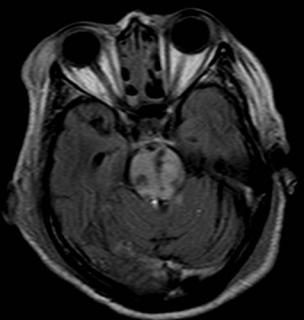
 D
D
122 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
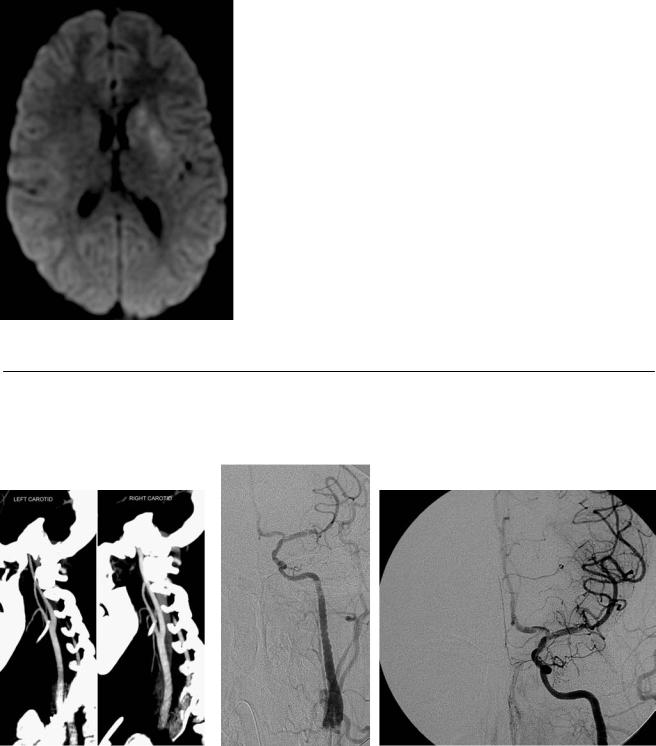
A 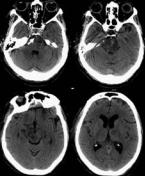 B
B 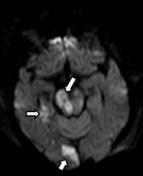 C
C 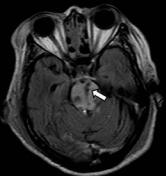
 D
D
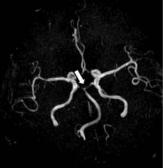
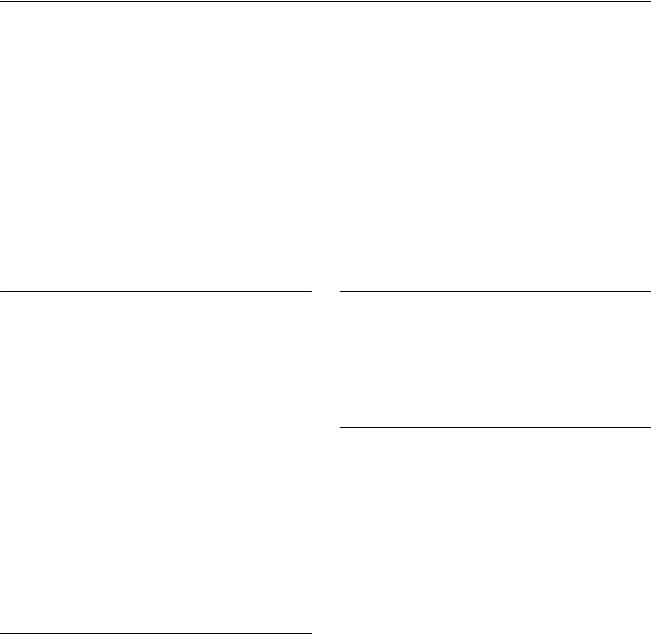
(A) Computed tomography (CT) of the brain shows areas of low attenuation in the pons, right cerebral peduncle, and left thalamus. Note the increased attenuation of the basilar artery (arrow). (B) Di usion-weighted image shows restricted di usion in the right side of the pons, right medial temporal lobe, and right occipital lobe (arrows). All the areas of hypoattenuation on the CT scan demonstrate restriction (not all of them shown). (C) Fluid-attenuated inversion recovery image through the pons shows increased signal and punctate areas of hemorrhage (arrow). (D) Magnetic resonance angiography (MRA) of the brain shows no flow-related signal in the basilar tip or proximal posterior cerebral arteries (arrow). The superior cerebellar arteries are irregular and narrow.
■ Di erential Diagnosis
•Basilar artery thrombosis with acute posterior circulation stroke: Acute ischemic changes involve variable extensions of the brainstem, cerebellum, thalami, and temporal and occipital lobes. Edema in the posterior fossa may result in obliteration of the 4th ventricle and acute hydrocephalus.
•Osmotic demyelination, also known as central pontine myelinolysis (CPM): Osmotic demyelination is a localized, frequently symmetric, noninflammatory demyelination within the central pons. In 10% of patients, demyelination is present in extrapontine regions, including the midbrain, thalami, basal nuclei, and cerebellum. CPM occurs inconsistently as a complication of severe and prolonged hyponatremia, particularly when it is corrected too rapidly. T2-weighted magnetic resonance imaging (MRI) shows hyperintense areas where demyelination has occurred.
•Thrombosis of the deep cerebral veins: This causes symmetric infarcts that a ect the thalami bilaterally, possibly extending into the basal ganglia and adjacent white matter bilaterally. The venous structures, such as the thalamostriate vein, internal carotid vein, vein of Rosenthal, vein of Galen, straight sinus, and torcular, are hyperattenuated on CT. Hydrocephalus may occur as a consequence of edema and swelling of both thalami.
•The superior cerebellar artery supplies the superior cerebellum, including the superior cerebellar peduncle, as well as the upper dorsolateral pons and midbrain.
•Basilar artery branches (perforators) supply the paramedian and anterolateral brainstem.
•The proximal posterior cerebral artery, referred to as the precommunicating or P1 segment, supplies regions of the midbrain, mammillary body, and optic tract.
•Mechanism of basilar artery occlusion:
•Most cases of distal (top of the basilar artery) or proximal (vertebrobasilar junction) occlusion are caused by embolism from either a cardiac or an arterial source.
•Midbasilar artery occlusion is typically the result of atherothrombosis.
•Arterial dissections are very rare and usually involve the vertebral artery, with occasional extension to the basilar artery.
■ Other Imaging Findings
•The sensitivity of CT to detect posterior circulation stroke is poor.
•MRI and MRA are highly sensitive to detect acute ischemia and arterial occlusion.
•MRA may overestimate the degree of stenosis because of reduced flow.
■ Essential Facts
•Variable symptoms result from ischemia of the cerebellum, brainstem, occipital lobes, and thalami.
•Vascular territories:
•The posterior inferior cerebellar artery (PICA) and the anterior inferior cerebellar artery supply the inferior cerebellum and lateral aspects of the medulla and pons, respectively.
¸Pearls & ˚ Pitfalls
¸Top-of-the-basilar syndrome: severe impairment of con-
sciousness, usually bilateral oculomotor palsies, visual fields defects, cerebellar symptoms, and hemiplegia or tetraplegia
¸ Results from thalamic, occipital, and cerebellar infarctions
˚A hypoplastic vertebral artery may terminate in the PICA without connecting to the basilar artery. This finding can be mistaken for occlusion.
123
Case 62
A 
 B
B
■ Clinical Presentation
A 47-year-old woman with transient weakness.
Further Work-up
C
124 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
A  B
B 
 C
C
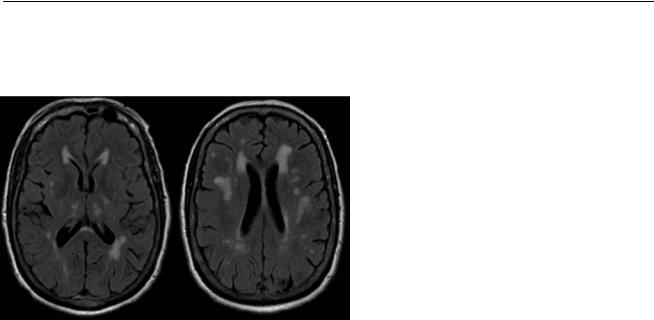
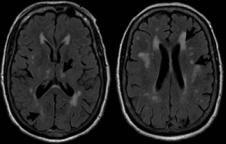
(A) Computed tomography (CT) of the brain shows numerous small areas of low attenuation in the deep white matter bilaterally and in the left thalamus (arrows). (B) Di usion-weighted image shows restriction in the left thalamus (arrow). The centrum semiovale is unremarkable. (C) Fluid-attenuated inversion recovery (FLAIR) images demonstrate numerous areas of high signal (arrows), including the lesion with restricted di usion in the left thalamus.
■ Di erential Diagnosis
•Acute and chronic lacunar infarcts: These present as multiple small areas of T2 signal abnormality; if magnetic resonance imaging (MRI) is acquired in the acute phase, there is restricted di usion. The distribution is not typical for demyelinating lesions.
•Multiple sclerosis (MS): MS is an inflammatory, demyelinating disease of the central nervous system. On MRI, typical MS appears as oval areas of T2 hyperintensity in the periventricular regions, with their longest axis oriented perpendicular to the ventricular surface. White matter lesions involving the corpus callosum, infratentorial compartment, and spinal cord make the diagnosis of MS more likely. Enhancement and restricted di usion are seen in active lesions.
•Migraine-related ischemic lesions: There is an increased frequency of small white matter lesions in patients with a history of migraine headaches. These are believed to represent subclinical infarcts.
■ Essential Facts
•Lacunes are small subcortical infarcts (< 15 mm in diameter) in the territory of the deep penetrating arteries.
•Lacunar infarcts may be asymptomatic, or patients may present with specific lacunar syndromes: pure motor stroke/hemiparesis, ataxic hemiparesis, dysarthria/clumsy hand, pure sensory stroke, or mixed sensorimotor stroke
•They occur most frequently in the basal ganglia and internal capsule, thalamus, corona radiata, and pons.
•Associated conditions include hypertension, smoking, diabetes, and microemboli from the heart or carotid arteries.
■ Other Imaging Findings
•CT findings may be normal, or a small area of low attenuation may be seen. The age of lacunar infarcts is di cult to establish with CT.
•MRI demonstrates restricted di usion. A few hours later, a T2 signal increase is also present.
¸Pearls & ˚ Pitfalls
¸Other forms of arteriopathy that can a ect small vessels
include amyloid angiopathy, hemodynamic disorders, and cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL).
¸ Abnormalities in the perfusion studies may predict progression of a lacunar stroke.
˚Virchow-Robin spaces are extensions of the subarachnoid space surrounding the blood vessels and should not be mistaken for lacunar infarcts. They follow the signal of cerebrospinal fluid on all sequences. Increased FLAIR signal or restricted di usion should not be present.
125
Case 63
A
■ Clinical Presentation
A 78-year-old man with a history of prior cerebral hemorrhage presenting with headache and right leg weakness.
Further Work-up
B C D
126 RadCases.thieme.com |
RadCases Neuro Imaging |
|
|
■ Imaging Findings |
|
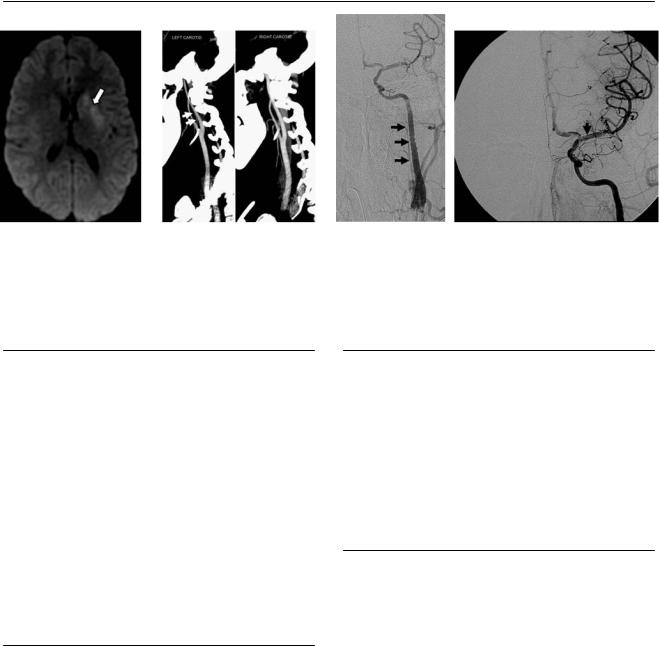
A  B
B 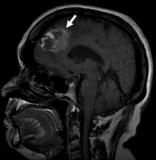 C
C 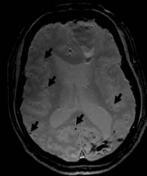
 D
D
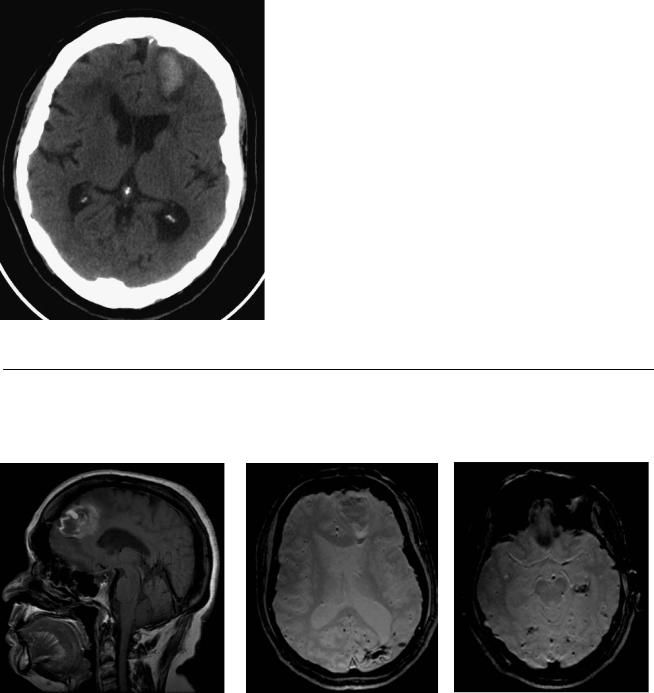
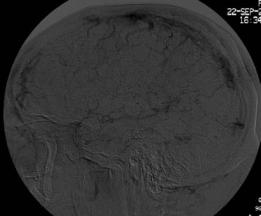
(A) Nonenhanced computed tomography (CT) of the brain demonstrates acute hemorrhage in the left frontal lobe (arrow). (B) Sagittal T1-weighted image (WI) of the brain shows a subacute hematoma in the right frontal lobe (arrow). (C) Gradient-echo (GRE) T2*WI shows an acute left frontal hematoma, an old left occipital hemorrhagic lesion, and multiple punctate foci of hemosiderin deposition in the subcortical regions of both cerebral hemispheres (arrows). (D) GRE T2*WI: note the multiple punctate foci of hemosiderin deposition in both cerebral hemispheres (arrows).
■ Di erential Diagnosis
•Intracranial hemorrhage (ICH) secondary to cerebral amyloid angiopathy (CAA): CAA causes multiple and recurrent ICH in a cortical-subcortical distribution that generally spares the deep white matter, basal ganglia, and brainstem. It may involve the cerebellum. Subarachnoid and subdural hemorrhage (may be primary or due to direct extension of the cortical-subcortical hemorrhage) can also occur. Cortical microhemorrhages can be better visualized on GRE T2*-weighted magnetic resonance imaging (MRI).
•Hypertensive ICH: Hypertension is the most common cause of nontraumatic hemorrhage in adults. In contrast to the typical cortical-subcortical location of CAA-related hemorrhage, hypertensive hemorrhages, both large and small, most commonly occur in the deep gray matter, such as the basal ganglia and thalami, or in the brainstem.
•Hemorrhagic metastasis: The intracerebral metastases most prone to hemorrhage include malignant melanoma, choriocarcinoma, renal cell carcinoma, bronchogenic carcinoma, and thyroid malignancy. Of the primary gliomas, glioblastoma multiforme, oligodendroglioma, and ependymoma are the ones that can present with hemorrhage.
■ Essential Facts
•CAA is an important cause of spontaneous cortical-subcor- tical ICH in the normotensive elderly.
•There may be deposition of β-amyloid protein in the media and adventitia of small and medium-size vessels of the cerebral cortex, subcortex, and leptomeninges.
•The clinical presentation includes sudden neurologic deficit (stroke) related to acute ICH and symptoms resembling those of a transient ischemic attack or dementia.
■ Other Imaging Findings
•CT shows acute hemorrhage or encephalomalacia from prior bleeding. Leukoaraiosis is frequently present.
•GRE T2*-weighted MRI is used to evaluate for microhemorrhages.
¸Pearls & ˚ Pitfalls
¸Cerebral microhemorrhages can be seen in patients with
CAA and chronic systemic hypertension most commonly.
¸Other causes of ICH include di use axonal injury, cerebral embolism, cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL), multiple cavernous malformations, vasculitis, hemorrhagic micrometastasis, and radiation vasculopa-
thy.
˚Increased T1 signal intensity in a hematoma should not be mistaken for enhancement.
127
Case 64
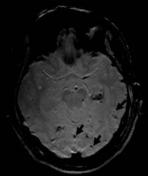
A
■ Clinical Presentation
A 72-year-old man with a history of treated cancer, now presenting with severe headache.
Further Work-up
B 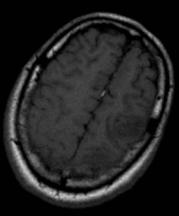 C
C 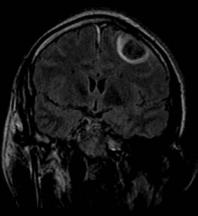
 D
D
