
- •CONTENTS
- •EXPERTS
- •CONTRIBUTORS
- •ABBREVIATIONS
- •1 The management of chronic subdural haematoma
- •2 Glioblastoma multiforme
- •3 Spondylolisthesis
- •4 Intramedullary spinal cord tumour
- •5 Surgery for temporal lobe epilepsy
- •6 Management of lumbosacral lipoma in childhood
- •7 Idiopathic intracranial hypertension
- •8 Colloid cyst of the third ventricle
- •9 Bilateral vestibular schwannomas: the challenge of neurofibromatosis type 2
- •10 Multimodality monitoring in severe traumatic brain injury
- •11 Intracranial abscess
- •12 Deep brain stimulation for debilitating Parkinson’s disease
- •14 Trigeminal neuralgia
- •15 Cerebral metastasis
- •16 The surgical management of the rheumatoid spine
- •17 Cervical spondylotic myelopathy
- •18 Brainstem cavernous malformation
- •19 Peripheral nerve injury
- •20 Spontaneous intracerebral haemorrhage
- •21 Low-grade glioma
- •22 Intracranial arteriovenous malformation
- •INDEX
CASE
7Idiopathic intracranial hypertension
David Sayer
 Expert commentary Raghu Vindindlacheruvu
Expert commentary Raghu Vindindlacheruvu
Case history
A 20-year-old lady presented to her local Accident and Emergency (A&E) department with a history of gradual onset headache over a period of 6 months, associated with visual disturbance. The headache was global, dull, and worse when she was lying flat. It increased when she laughed and coughed. The patient described blurring of her vision with onset at the same time as her headache. Her body mass index (BMI) was 32. There was no family history of headaches, she had previously had one child, and there were no risks factors for thrombosis.
Her previous medical history was otherwise unremarkable and she took no regular medication. Neurological examination was unremarkable, but fundoscopy revealed bilateral papilloedema.
A non-contrasted CT head scan was normal. At a lumbar puncture, the opening pressure was 50cmH2O and 50mL of CSF was drained to bring the pressure down to 18cmH2O. The protein content of the CSF was 0.25g/L and the glucose was 3.6mmol/L (both normal). She initially complained of a post-lumbar puncture headache, but this settled after a few hours. Over the next few weeks her headache and visual disturbance improved. She was advised to lose weight, although this was never achieved.
 Learning point Cerebrospinal fluid constituents and pressure (Table 7.1)
Learning point Cerebrospinal fluid constituents and pressure (Table 7.1)
Table 7.1 CSF constituents and pressure
CSF constituent |
Normal range |
|
|
CSF pressure |
5–15mmHg (7–20cmH2O) |
Protein |
0.15–0.45g/L |
Glucose |
3.3–4.4mmol/L |
White cell count (WCC) |
0–5 × 106/L |
Red cell count (RCC) |
0–10 × 106/L |
|
|
 Expert comment Initial work-up and management of idiopathic intracranial hypertension (IIH)
Expert comment Initial work-up and management of idiopathic intracranial hypertension (IIH)
The natural history of IIH is variable. It may be self-limiting, intermittent, or become progressively worse. Approximately one-third of patients are in each of these categories [1]. The worst complication is visual loss and
can be severe in up to 25% of patients [2].
The neurological diagnosis was IIH. Over the next 12 months her condition was managed medically with repeated lumbar punctures and acetazolamide, starting at 250mg daily and escalating by 250mg weekly to a maximum dose of 1000mg/ day. Unfortunately, while acetazolamide gave her some symptomatic relief she had to discontinue it as she found the side effects of gastrointestinal upset and fatigue
70 |
Challenging concepts in neurosurgery |
|
intolerable. To compound this, after every lumbar puncture, she suffered for a num- |
|
ber of weeks with low pressure headaches. These were followed by a quiescent |
|
period, then a gradual return of her pressure symptoms. |
 Learning point Diagnostic criteria for idiopathic intracranial hypertension
Learning point Diagnostic criteria for idiopathic intracranial hypertension
Modified Dandy Criteria for the Diagnosis of Idiopathic Intracranial Hypertension [3]
● Signs and symptoms of increased intracranial pressure (ICP).
● No localizing focal neurological signs except unilateral or bilateral sixth nerve paresis. ● CSF opening pressure >25cmH2O, without cytological or chemical abnormalities.
● Normal neuroimaging adequate to exclude cerebral venous thrombosis.
 Learning point Acetazolamide
Learning point Acetazolamide
Acetazolamide is a carbonic anhydrase inhibitor that is believed to work by decreasing the rate of CSF production. CSF is formed as an ultrafiltrate of plasma and active secretion of CSF in the choroid plexus. This process is energy dependent and requires the enzyme carbonic anhydrase. This enzyme converts carbon dioxide and water into carbonic acid. Acetazolamide inhibits this
enzyme and thus the reaction. This reaction takes place in the epithelial cells of the choroid plexus [4]. As a sulphonamide derivative potential side effects of acetazolamide are blood disorders, such as leukopenia, leading to infections and rashes. Other side effects and nausea/vomiting, headache, fatigue, and GI disturbances including taste disturbance [5].
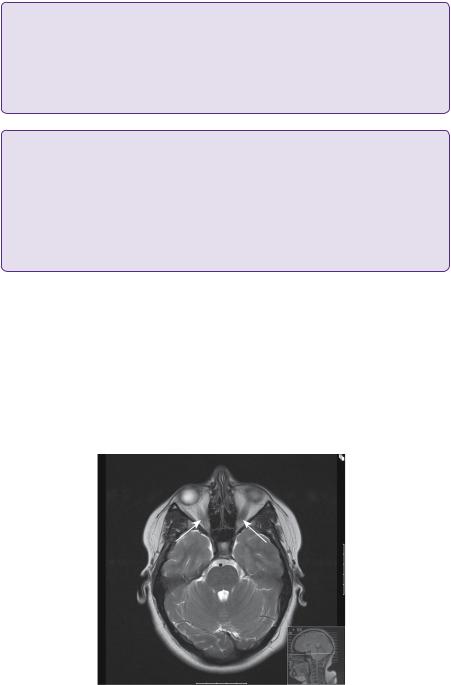
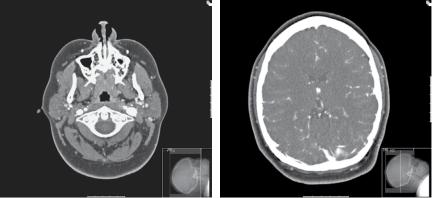
At this point, she was referred for a neurosurgical opinion. An MRI scan demonstrated engorgement and dilatation of the optic nerve sheath complexes bilaterally (Figure 7.1). A small incidental lesion in the left parietal lobe was found to be an unrelated cavernoma. A CT venogram preand post-lumbar puncture demonstrated static narrowing of the tranverse sinuses (Figure 7.2). At this point, the opening pressure was 40cmH2O and after drainage of 32mL of CSF, and the closing pressure was 12cmH2O.
In view of the significant post-lumbar puncture headaches, it was recommended that lumbar peritoneal or ventricular peritoneal shunting should be avoided if possible in the first instance. Instead, she was assessed for venous sinus stenting and
Figure 7.1. T2-weighted axial MRI imaging demonstrating bilateral optic nerve engorgement (arrows).
Case 7 Idiopathic intracranial hypertension |
71 |
(a) |
(b) |
Figure 7.2. CTA (delayed filling of venous structures) demonstrating asymmetry of the internal jugular veins (a), and narrowed transverse venous sinuses (b).
offered venous pressure measurements of the transverse sinus, but she declined this treatment, preferring the option of shunting. At this time, she was undergoing approximately one lumbar puncture every 3 months to control her symptoms.
She underwent insertion of a valveless lumbar peritoneal shunt. In the immediate post-operative period she experienced low pressure headaches, which resolved over the ensuing week. She then had a number of weeks of complete symptom resolution, but high pressure symptoms subsequently recurred. A further lumbar puncture revealed an opening pressure of 32cmH2O. Ophthalmological assessment showed an acuity of 6/5 in the right eye and 6/9 on the left, with papilloedema and mild enlargement of the blind spot in both eyes, unchanged from before.
After careful counselling, she was offered VP shunting on the basis that she had benefitted from repeated lumbar punctures and the lumbar peritoneal shunt had initially resolved symptoms. At this point she became pregnant and her treatment was deferred. After delivery, the patient’s symptoms had improved to a tolerable level and she decided that she did not wish to proceed with the shunt.
Discussion
Idiopathic intracranial hypertension has also been called benign intracranial hypertension (despite not running a benign course) and pseudotumour cerebri. The clinical and imaging features of the syndrome are of raised ICP, without dilated ventricles or intracranial mass lesions, but with evidence of papilloedema [6]. In 90% of cases this affects obese women with an incidence of 3.5/100 000 in the 20–44 years age group [7].
The commonest symptom is headache. This tends to be a non-specific global headache that is aggravated by actions that increase the cerebral venous pressure, e.g. coughing, sneezing, and straining on defaecation. It can be accompanied by features associated with migraine, such as photosensitivity, nausea, and vomiting [1]. Visual disturbance is also common and can manifest as blurring or transient visual obscurations. These may be postural. Other symptoms include diplopia, visual field deficits, and pulsatile tinnitus. Focal neurology is rare and should prompt a search for another cause. Papilloedema is the diagnostic hallmark of this condition and, indeed, it is sometimes an incidental finding in an otherwise asymptomatic patient.
72
 Learning point Opthalmological findings in idiopathic intracranial hypertension
Learning point Opthalmological findings in idiopathic intracranial hypertension
●Bilateral papilloedema.
●Decreasing visual acuity.
●Enlargement of blind spot.
●VI cranial nerve palsy.
 Learning point MRI findings in idiopathic intracranial hypertension [3]
Learning point MRI findings in idiopathic intracranial hypertension [3]
●Flattening of the posterior globe of the eye.
●Dilatation and tortuosity of optic nerve sheaths.
●Empty sella turcica.
●Stenosis of one or other of transverse venous sinuses.
 Expert comment Transverse sinus stenosis implications
Expert comment Transverse sinus stenosis implications
Transverse sinus stenosis can lead to intracranial venous hypertension. This, in turn,
decreases the rate of absorption of CSF, causing a rise in CSF pressure and the symptoms associated with IIH. A potential therapeutic target to alleviate this condition
is to ‘correct’ the transverse sinus stenosis.
 Learning point Complications of lumbar peritoneal shunts [11]
Learning point Complications of lumbar peritoneal shunts [11]
●Shunt failure.
●CSF leak.
●Over drainage.
●Meningitis.
●Nerve root damage.
●Damage to intraperitoneal structures.
Challenging concepts in neurosurgery
A diagnostic lumbar puncture should be performed and, by definition, the opening pressure should be above 25cmH2O [7]. The CSF analysis should also be normal.
In the first instance, a non-contrasted CT head scan is performed to exclude hydrocephalus and ensure safety of lumbar puncture. A contrasted MRI scan is normally also performed to exclude mass lesions or meningeal infiltration, which may be responsible for raised pressure. Additional imaging may include MRI of the spine to exclude abnormalities such as Chiari malformation, imaging of the venous sinuses, either by CT venography, MR venography, or angiography, to exclude venous sinus thrombosis or to demonstrate narrowing of the sinuses that may present a therapeutic target [1].
IIH is primarily a diagnosis of exclusion. A careful history and examination must be performed to rule out any other potential causes for the headaches. Imaging as described above excludes any mass lesions and ensures that ventricles are of normal size. Lumbar puncture confirms raised pressure and CSF analysis further excludes any other secondary causes. Treatment is typically medical in the initial setting. Visual deterioration will lead to more aggressive and earlier treatment. Once treatment has been started, it is reasonable to review the patient regularly and gradually decrease the dosage of acetazolamide, as the condition stabilizes and improves. Management, however, is often difficult and protracted.
The patient should be advised to lose weight and strategies put in place to help the patient achieve this, including bariatric surgery where necessary [8]. Pregnancy may worsen symptoms and patients must be aware of the implications of this, particularly with regard to vision [1].
 Expert comment The efficacy of conservative measures
Expert comment The efficacy of conservative measures
With regard to the control of headache, analgesia is frequently prescribed, but is not usually helpful and may lead to ‘analgesic abuse’ headaches. Acetazolamide can be added as described above, although side effects may be an issue. Other medication, which may be useful includes topiramate [9], which has a weak carbonic anhydrase inhibitor action, steroids, and octreotide, an inhibitor of insulin like growth factor [10]. The mainstay of conservative management, however, is therapeutic lumbar puncture.
It must be stressed that, while conservative/medical approaches are effective in many patients, if vision is deteriorating, then other options must be explored urgently, primarily CSF diversion. If repeated lumbar punctures are giving satisfactory relief, but are undesirable, shunting should be considered. Either lumboperitoneal (LP) or ventriculo-peritoneal (VP) shunts may be used, depending on surgeon/ patient preference.
 Clinical tip Lumboperitoneal shunts—valve or valveless?
Clinical tip Lumboperitoneal shunts—valve or valveless?
Recently, LP shunts can incorporate valves, allowing for pressure or flow control of CSF transit. There is no doubt that adopting an erect posture will increase CSF pressure in the lumbar cistern and increase flow into the peritoneal cavity: this may underlie the development of the low pressure headache and occasionally iatrogenic Chiari malformation (chronic hindbrain herniation). However,
the development of LP valves and, in particular, the science behind flowand pressure-adjustments is in its infancy, and further research is required.

Case 7 Idiopathic intracranial hypertension |
73 |
 Learning point Intracranial venous sinus stenting [12]
Learning point Intracranial venous sinus stenting [12]
Transverse sinus stenosis may be focal or diffuse. The exact nature of the stenosis is ascertained by MR venography, particularly the auto-triggered elliptic centric-ordered (ATECO sequence) technique, giving excellent anatomical detail. If amenable to stenting, this is performed under general anaesthesia. Stenting requires heparin cover and pre-treatment with clopidogrel,
with aspirin and clopidogrel therapy for a number of months following procedure to prevent thrombosis. Increasing the flow in the transverse sinus reduces venous hypertension and thus relieves symptoms.
A final word from the expert
The complex nature of this disease often necessitates a multi-disciplinary approach and referral to an ophthalmic surgeon should be considered as fenestration of the optic nerve sheath [13] allows direct drainage of CSF away from the optic nerve providing protection against visual deterioration with a significant chance of visual improvement.
If there is narrowing of the transverse sinus, stenting is another option [14]. This is a new treatment, but shows promise. Another potential treatment option is bilateral subtemporal craniectomies [15].
To summarize, IIH is a poorly understood condition. Patients who develop it often have a prolonged course with a risk of severe loss. The variety of management options available demonstrates that there is no single therapy that works for all patients and treatment needs to be directed by the patient’s response.
References
1.Winn H. Youman’s neurological surgery, 6th edn. Amsterdam: Elsevier.
2.Krajewski KJ, Gurwood AS. Idiopathic intracranial hypertension: pseudotumor cerebri. Optometry 2002; 73(9): 546–52.
3.Biousse V, Bruce B, Newman N. Update on the pathophysiology and management of idiopathic intracranial hypertension. Journal of Neurology, Neurosurgery & Psychiatry 2012; 83: 488–94.
4.Brown PD, Davies SL, Speake T, et al. Molecular mechanisms of cerebrospinal fluid production. Neuroscience 2004; 129(4): 957–70.
5.Joint Formulary Committee. British national formulary, 62nd edn. London: Pharmaceutical Press.
6.Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri. Population studies in Iowa and Louisiana. Archives of Neurology 1988; 45: 875–7.
7.Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology 2002; 59: 1492e5.
8.Ko MW, Chang SC, Ridha MA, et al. Weight gain and recurrence in idiopathic intracranial hypertension: a case-control study. Neurology 2011; 76: 1564e7.
9.Celebisoy N, Gokcay F, Sirin H, et al. Treatment of idiopathic intracranial hypertension: topiramate vs acetazolamide, an open-label study. Acta Neurologica Scandinavica 2007; 116: 322e7.
74 |
Challenging concepts in neurosurgery |
|
|
10. |
Deftereos SN, Panagopoulos G, Georgonikou D, et al. Treatment of idiopathic intracranial |
|
|
hypertension: is there a place for octreotide? Cephalalgia 2011; 31: 1679e80. |
|
11. |
Yadav YR, Prihar V, Agarwal M, et al. Lumbar periotenal shunting in idiopathic intracra- |
|
|
nial hypertension. Turkish Neurosurgery 2012, 22(1): 21–6. |
|
12. |
Ahmed RM, Wilkinson M, Parker GD, et al. Transverse sinus stenting for idiopathic |
|
|
intracranial hypertension: a review of 52 patients and of model predications. AJNR |
|
|
American Journal of Neuroradiology 2011; 32(8): 1408–14. |
|
13. |
Thambisetty M, Lavin PJ, Newman NJ, et al. Fulminant idiopathic intracranial hyperten- |
|
|
sion. Neurology 2007; 68: 229e32. |
|
14. |
Ahmed R, Friedman DI, Halmagyi GM. Stenting of the transverse sinuses in idiopathic |
|
|
intracranial hypertension. Journal of Neuroophthalmology 2011; 31: 374e80. |
|
15. |
Werndle MC, Newling-Ward E, Rich P, et al. Patient controlled intracranial pressure for |
|
|
treating idiopathic intracranial hypertension. Proceedings of the 2012 Spring Meeting of the |
|
|
Society of British Neurological Surgeons. British Journal of Neurosurgery 2012; 26(2): 132–74. |
