
- •Table of Contents
- •Copyright
- •Dedication
- •Introduction to the eighth edition
- •Online contents
- •List of Illustrations
- •List of Tables
- •1. Pulmonary anatomy and physiology: The basics
- •Anatomy
- •Physiology
- •Abnormalities in gas exchange
- •Suggested readings
- •2. Presentation of the patient with pulmonary disease
- •Dyspnea
- •Cough
- •Hemoptysis
- •Chest pain
- •Suggested readings
- •3. Evaluation of the patient with pulmonary disease
- •Evaluation on a macroscopic level
- •Evaluation on a microscopic level
- •Assessment on a functional level
- •Suggested readings
- •4. Anatomic and physiologic aspects of airways
- •Structure
- •Function
- •Suggested readings
- •5. Asthma
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic approach
- •Treatment
- •Suggested readings
- •6. Chronic obstructive pulmonary disease
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic approach and assessment
- •Treatment
- •Suggested readings
- •7. Miscellaneous airway diseases
- •Bronchiectasis
- •Cystic fibrosis
- •Upper airway disease
- •Suggested readings
- •8. Anatomic and physiologic aspects of the pulmonary parenchyma
- •Anatomy
- •Physiology
- •Suggested readings
- •9. Overview of diffuse parenchymal lung diseases
- •Pathology
- •Pathogenesis
- •Pathophysiology
- •Clinical features
- •Diagnostic approach
- •Suggested readings
- •10. Diffuse parenchymal lung diseases associated with known etiologic agents
- •Diseases caused by inhaled inorganic dusts
- •Hypersensitivity pneumonitis
- •Drug-induced parenchymal lung disease
- •Radiation-induced lung disease
- •Suggested readings
- •11. Diffuse parenchymal lung diseases of unknown etiology
- •Idiopathic pulmonary fibrosis
- •Other idiopathic interstitial pneumonias
- •Pulmonary parenchymal involvement complicating systemic rheumatic disease
- •Sarcoidosis
- •Miscellaneous disorders involving the pulmonary parenchyma
- •Suggested readings
- •12. Anatomic and physiologic aspects of the pulmonary vasculature
- •Anatomy
- •Physiology
- •Suggested readings
- •13. Pulmonary embolism
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic evaluation
- •Treatment
- •Suggested readings
- •14. Pulmonary hypertension
- •Pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic features
- •Specific disorders associated with pulmonary hypertension
- •Suggested readings
- •15. Pleural disease
- •Anatomy
- •Physiology
- •Pleural effusion
- •Pneumothorax
- •Malignant mesothelioma
- •Suggested readings
- •16. Mediastinal disease
- •Anatomic features
- •Mediastinal masses
- •Pneumomediastinum
- •Suggested readings
- •17. Anatomic and physiologic aspects of neural, muscular, and chest wall interactions with the lungs
- •Respiratory control
- •Respiratory muscles
- •Suggested readings
- •18. Disorders of ventilatory control
- •Primary neurologic disease
- •Cheyne-stokes breathing
- •Control abnormalities secondary to lung disease
- •Sleep apnea syndrome
- •Suggested readings
- •19. Disorders of the respiratory pump
- •Neuromuscular disease affecting the muscles of respiration
- •Diaphragmatic disease
- •Disorders affecting the chest wall
- •Suggested readings
- •20. Lung cancer: Etiologic and pathologic aspects
- •Etiology and pathogenesis
- •Pathology
- •Suggested readings
- •21. Lung cancer: Clinical aspects
- •Clinical features
- •Diagnostic approach
- •Principles of therapy
- •Bronchial carcinoid tumors
- •Solitary pulmonary nodule
- •Suggested readings
- •22. Lung defense mechanisms
- •Physical or anatomic factors
- •Antimicrobial peptides
- •Phagocytic and inflammatory cells
- •Adaptive immune responses
- •Failure of respiratory defense mechanisms
- •Augmentation of respiratory defense mechanisms
- •Suggested readings
- •23. Pneumonia
- •Etiology and pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features and initial diagnosis
- •Therapeutic approach: General principles and antibiotic susceptibility
- •Initial management strategies based on clinical setting of pneumonia
- •Suggested readings
- •24. Bacterial and viral organisms causing pneumonia
- •Bacteria
- •Viruses
- •Intrathoracic complications of pneumonia
- •Respiratory infections associated with bioterrorism
- •Suggested readings
- •25. Tuberculosis and nontuberculous mycobacteria
- •Etiology and pathogenesis
- •Definitions
- •Pathology
- •Pathophysiology
- •Clinical manifestations
- •Diagnostic approach
- •Principles of therapy
- •Nontuberculous mycobacteria
- •Suggested readings
- •26. Miscellaneous infections caused by fungi, including Pneumocystis
- •Fungal infections
- •Pneumocystis infection
- •Suggested readings
- •27. Pulmonary complications in the immunocompromised host
- •Acquired immunodeficiency syndrome
- •Pulmonary complications in non–HIV immunocompromised patients
- •Suggested readings
- •28. Classification and pathophysiologic aspects of respiratory failure
- •Definition of respiratory failure
- •Classification of acute respiratory failure
- •Presentation of gas exchange failure
- •Pathogenesis of gas exchange abnormalities
- •Clinical and therapeutic aspects of hypercapnic/hypoxemic respiratory failure
- •Suggested readings
- •29. Acute respiratory distress syndrome
- •Physiology of fluid movement in alveolar interstitium
- •Etiology
- •Pathogenesis
- •Pathology
- •Pathophysiology
- •Clinical features
- •Diagnostic approach
- •Treatment
- •Suggested readings
- •30. Management of respiratory failure
- •Goals and principles underlying supportive therapy
- •Mechanical ventilation
- •Selected aspects of therapy for chronic respiratory failure
- •Suggested readings
- •Index

7: Miscellaneous airway diseases
OUTLINE
Bronchiectasis, 107
Etiology and Pathogenesis, 107
Pathology, 109
Pathophysiology, 109
Clinical Features, 109
Diagnostic Approach, 110
Treatment, 111
Cystic Fibrosis, 112
Etiology and Pathogenesis, 112
Pathology, 113
Pathophysiology, 113
Clinical Features, 114
Diagnostic Approach, 114
Treatment, 115
Upper Airway Disease, 115
Etiology, 116
Pathophysiology, 116
Clinical Features, 116
Diagnostic Approach, 117
Treatment, 117
This chapter considers several disorders that affect airways, chosen because of their clinical or physiologic importance. The first of these disorders, bronchiectasis, is defined by chronic structural changes of airways that are often a consequence of prior respiratory tract infection and/or a variety of
underlying predisposing conditions. The second disorder, cystic fibrosis, is a genetic disease that usually
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/

first manifests in childhood and is notable for the serious clinical consequences that ensue. Finally, abnormalities of the upper airway (which for our purposes here includes the airway at or above the level of the trachea) are discussed briefly to acquaint the reader with the physiologic principles that allow detection of these disorders.
Bronchiectasis
Bronchiectasis is an irreversible dilation of airways caused by inflammatory destruction of airway walls. Because the most common etiologic factor is infection, which triggers the destructive inflammatory process, the involved area with bronchiectasis depends on the location and extent of the underlying infection. In some cases, bronchiectasis is localized to a specific region of the lung. In other cases, the process involves more than one area or even is diffuse, involving a large portion of both lungs.
Etiology and pathogenesis
Infection and impairment of drainage (frequently due to obstruction) are the two underlying problems that contribute to development of dilated or bronchiectatic airways. The responsible infection(s) may be viral or bacterial. Up until the mid-20th century in developed nations, measles and pertussis (whooping cough) pneumonia were common respiratory infections resulting in bronchiectasis. Currently, a variety of other viral and bacterial infections often are associated; important examples are tuberculosis and Mycobacterium avium complex. At times, inflammation resulting from hypersensitivity to fungal organisms is the underlying cause, as with allergic bronchopulmonary aspergillosis. This condition, found almost exclusively in patients with clinically apparent asthma or cystic fibrosis, is characterized by colonization of airways with Aspergillus organisms and by thick mucus plugs and bronchiectasis in relatively proximal airways.
Prior infection, obstruction, or both are the most common problems leading to bronchiectasis.
When an airway is obstructed, a superimposed infection is likely to develop behind the obstruction, causing injury to the airway wall and leading to bronchiectasis. Slow-growing tumors, thick mucus, or foreign bodies commonly cause bronchial obstruction that results in bronchiectasis. As will be described later in this chapter, poor airway clearance of thick mucus as well as impaired antimicrobial defenses are factors that make bronchiectasis an important consequence of cystic fibrosis.
A factor that plays a role in some patients is a defect in the ability of the airway to clear itself of, or protect itself against, bacterial pathogens (see Chapter 22). Such a defect predisposes a person to recurrent infections and eventually to airway dilation and bronchiectasis. The abnormality may involve inadequate humoral immunity and insufficient antibody production (hypogammaglobulinemia) or defective leukocyte function. Another potential cause is primary ciliary dyskinesia, in which ciliary dysfunction impairs the ability of the ciliary blanket that lines the airway to clear bacteria and protect the airway against infection. The ciliary dysfunction is not limited to the lower airways; it also affects the nasal mucosa and, in males, may affect sperm motility and hence fertility. Pathologically, the dynein arms that are a characteristic feature of the ultrastructure of cilia are frequently absent in this disorder. One specific syndrome associated with bronchiectasis and ciliary dysfunction is Kartagener syndrome, which includes a triad of sinusitis, bronchiectasis, and situs inversus (usually discovered because of the presence of dextrocardia) (Fig. 7.1).

FIGURE 7.1 Chest imaging studies from a patient with Kartagener syndrome,
showing dextrocardia and bronchiectasis. A, Posteroanterior (PA) chest x-ray. Note
the “L” at the top of the image, identifying the left side of the chest and documenting
that the heart is on the opposite (right) side. B, Coronal slice from the chest CT
scan. In addition to dextrocardia, multiple dilated airways are readily visible.
Source: (Courtesy Dr. Seth Kligerman.)
Whatever the underlying cause, a “vicious cycle” of events has been proposed to explain the evolution and potential for progression of disease. The cycle starts with infection or another injury to the airway wall leading to an inflammatory response, resulting in structural changes to the airway wall and impaired mucus clearance, which then facilitates ongoing or progressive infection, inflammation, and perpetuation of the cycle.
Abnormalities of ciliary structure and function can result in recurrent infections and bronchiectasis.
Pathology
The primary pathologic feature of bronchiectasis is evident on gross inspection of the airways, which are markedly dilated in the involved region (Fig. 7.2). Three specific patterns of dilation have been described: cylindrical (appearing as uniform widening of the involved airways), varicose (having irregularly widened airways resembling varicose veins), and saccular bronchiectasis (characterized by widening of peripheral airways in a balloon-like fashion). These terms are used when describing radiographic patterns but are not relevant clinically. The dilated airways typically are filled with a considerable amount of secretions that may be grossly purulent. Microscopic changes of the bronchial wall can be seen, including epithelial ulceration and squamous metaplasia, as well as infiltration by inflammatory cells (both lymphocytes and neutrophils) in the mucosa and submucosa.
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
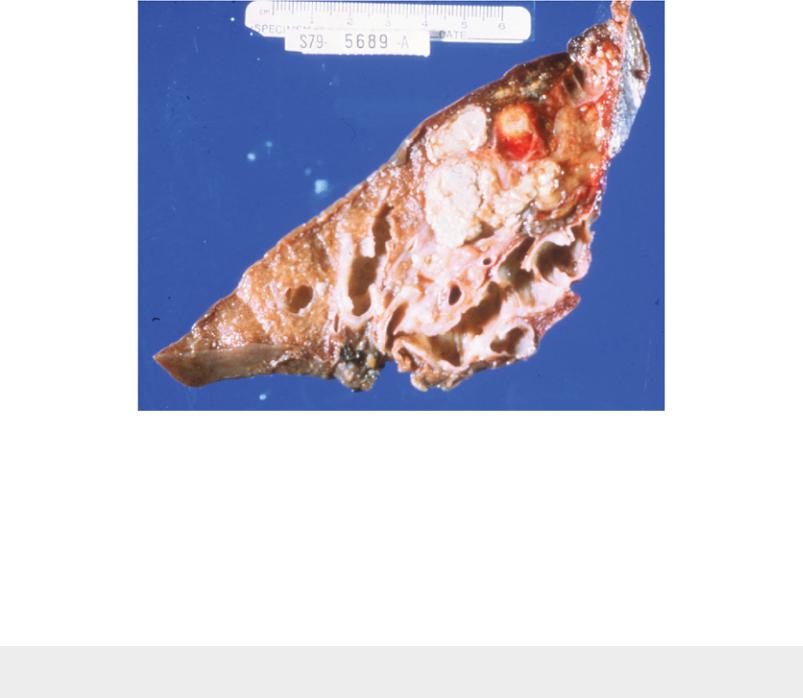
FIGURE 7.2 Surgically removed specimen of lung shows extensive bronchiectasis.
Some grossly dilated airways are filled with large amounts of mucoid and purulent
material.
As a result of the exuberant inflammatory changes in the bronchial wall, the blood supply, provided by the bronchial arteries, is increased. The arteries enlarge and increase in number, and new anastomoses may form between the bronchial and pulmonary artery circulations. Inflammatory erosion or mechanical trauma at the site of these vascular changes is often responsible for the hemoptysis seen frequently in patients with bronchiectasis.
Vessels from the bronchial arterial circulation supplying a bronchiectatic region are often a source of bleeding and hemoptysis.
Coexisting disease in the remainder of the tracheobronchial tree is common. Other areas of bronchiectasis may be present, or generalized changes of chronic bronchitis may be seen (see Chapter 6).
Pathophysiology
After the airways have become irreversibly dilated, their defense mechanisms against infection are disturbed. The normal propulsive action of cilia in the involved area is lost, even if it was intact before development of bronchiectasis. Bacteria colonize the enlarged airways, and secretions pool in the dilated sacs of patients with saccular bronchiectasis. Cough becomes much less effective at clearing secretions because of the abnormally collapsible airways. In many cases, the relationship established between the colonizing bacteria and the host is relatively stable over time, but the course may be punctuated by acute exacerbations of airway infection.
Functionally, patients with a localized area of bronchiectasis are not impaired to the same extent as patients with generalized obstructive lung disease. Measurement of pulmonary function may reveal surprisingly few if any abnormalities. When present, functional abnormalities are the result of either

extensive bronchiectasis involving a large area of one or both lungs or coexistent generalized airway disease, primarily chronic bronchitis.
Clinical features
The most prominent symptoms in patients with bronchiectasis are generally cough and copious sputum production. The sputum may be frankly purulent and tenacious, and often the profuse amount of yellow or green sputum production raises the physician’s suspicion of bronchiectasis. However, not all patients with bronchiectasis have significant sputum production. It has been estimated that approximately 10% to 20% of patients are free of copious sputum production; these patients are said to have “dry” bronchiectasis.
Common clinical features of bronchiectasis are as follows:
1.Cough
2.Copious and purulent sputum
3.Hemoptysis
4.Localized rales or rhonchi
5.Clubbing
The other frequent symptom in patients with bronchiectasis is hemoptysis, which may be massive and life-threatening. Hypertrophied bronchial arterial circulation to the involved area is responsible for this symptom in most cases. Because bronchial arteries are branches of the aorta and therefore perfused at systemic blood pressure, bleeding from these vessels can be brisk. Physical examination of the patient with bronchiectasis may reveal few abnormalities, even over the area of involvement. When present, abnormal findings, such as wheezes, crackles, or rhonchi in a localized area, are heard. Clubbing is frequently observed. Although the mechanism is not clear, clubbing is thought to be associated with the chronic suppurative process.
Whether gas exchange is abnormal in these patients often depends on the extent of involvement and the presence or absence of underlying chronic bronchitis. With well-localized disease, both PO2 and PCO2 may be normal. At the other extreme, patients with more severe disease may develop hypoxemia and hypercapnia. Cor pulmonale may subsequently develop.
Diagnostic approach
The diagnosis of bronchiectasis is usually suggested by a history of copious sputum production, frequent respiratory tract infections, hemoptysis, or all three. A chest radiograph often reveals nonspecific abnormalities in the involved area. The radiograph may show an area of increased markings, crowded vessels, or “ring” shadows corresponding to dilated or saccular airways. However, none of the findings on the routine radiograph is considered diagnostic of bronchiectasis.
High-resolution computed tomography (HRCT) provides a definitive diagnosis and is the initial procedure used to define the presence, location, and extent of bronchiectasis (Fig. 7.3). HRCT (with sections 1-2 mm thick) provides excellent detail and is particularly useful for detecting subtle bronchiectasis. In the past, the definitive diagnosis depended on bronchography, a radiographic procedure in which an inhaled opaque contrast material was used to outline part of the tracheobronchial tree (Fig. 7.4). This procedure is uncomfortable, can induce bronchospasm, and is not currently performed.
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/

FIGURE 7.3 High-resolution computed tomography scan of bronchiectasis shows dilated airways in both lower lobes and in the lingula. When seen in cross-section, dilated airways have a ringlike appearance.

FIGURE 7.4 Bronchogram of patient with extensive saccular bronchiectasis,
primarily in right upper lobe.
Examination of the sputum for microorganisms may be helpful, particularly during an acute exacerbation of the disease. Patients with bronchiectasis frequently become colonized and infected with Pseudomonas aeruginosa or nontuberculous mycobacteria (see Chapter 25), and the finding of these otherwise relatively unusual pathogens may be a clue to the presence of underlying bronchiectasis. The effects of bronchiectasis on functional evaluation were discussed in the sections on pathophysiology and clinical features.
Treatment
The three major aspects of treatment of bronchiectasis are control of infection, mobilization and clearance of airway secretions, and suppression of the inflammatory response. Bronchodilators are also frequently used in the patient who has functional evidence of airflow obstruction. Antibiotics to control infection are used and are dependent on the particular organisms cultured from the airways. Patients are typically treated during an exacerbation of their disease (i.e., when the quantity or appearance of the sputum unequivocally changes). In addition, some patients also are treated on a more chronic or intermittent basis with antibiotics in an attempt to suppress or even eradicate colonizing bacteria, with the intent of reducing symptoms and exacerbations. Oral agents that are typically effective against many strains of Streptococcus pneumoniae and Haemophilus influenzae are often used in patients with bronchiectasis in whom Pseudomonas aeruginosa has not yet become problematic. When these patients are infected with Pseudomonas organisms, treatment is generally more difficult. Inhaled tobramycin is sometimes used to suppress the growth of Pseudomonas and other Gram-negative organisms. Parenteral antibiotic therapy with either one or two antibiotics active against Pseudomonas is often administered, particularly during
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
