
- •Preface to the Second Edition
- •Foreword to the First Edition
- •Preface to the First Edition
- •Contents
- •Abbreviations
- •1.1 Magnetic Resonance Sequences
- •1.2 Practical Setup of an MRCP Study
- •1.3 Use of Contrast Media and Drugs
- •2 Intrahepatic Bile Ducts
- •2.1 Normal Anatomy and Variants
- •2.2 Benign Nontraumatic Abnormalities
- •2.4 Malignant Tumors
- •3 Extrahepatic Bile Duct
- •3.1 Normal Anatomy and Variants
- •3.2 Benign Nontraumatic Abnormalities
- •3.4 Malignant Tumors
- •4 Gallbladder and Cystic Duct
- •4.1 Normal Anatomy and Variants
- •4.2 Benign Nontraumatic Abnormalities
- •4.4 Malignant Tumors
- •5 Vaterian Sphincter Complex
- •5.1 Normal Anatomy and Variants
- •5.2 Benign Nontraumatic Abnormalities
- •5.4 Malignant Tumors
- •6 Pancreatic Ducts
- •6.1 Normal Anatomy and Variants
- •6.2 Benign Nontraumatic Abnormalities
- •6.4 Malignant Tumors and Tumors with Malignant Potential
- •Subject Index
236 4.4 Malignant Tumors
4.4 Malignant Tumors
#115 Gallbladder Carcinoma,
General
KEY FACTS: DISEASE
●Histology: variable (from well-differen- tiated to anaplastic)
●Incidence:
–Most common biliary cancer
–Found in 0.4%–0.6% of biliary tract operations
●Peak age: sixth to seventh decade
●Ratio of women to men: 3 : 1
●Location: usually body, fundus
●Predisposing factors/associated disease:
–Porcelain gallbladder (incidence of carcinoma up to 22%; see # 110)
–Gallstones (in 65%–98%; carcinoma occurs in only 1% of patients with stones, however)
–Chronic cholecystitis
–Anomalous pancreaticobiliary duct union (see # 123)
–Focal adenomyomatosis (see # 109)
●Symptoms: either signs of malignancy or signs of cholecystitis
●75% unresectable at the time of diagnosis
●88% mortality rate within 1 year
KEY FACTS: MRI
●Morphologic appearance:
–Mass replacing the gallbladder (40%–70%)
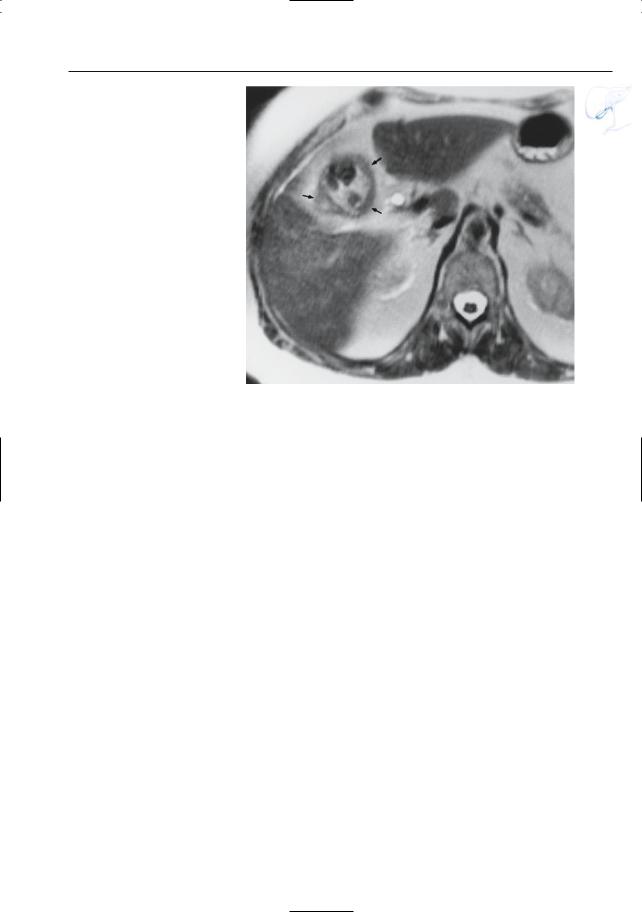
–Focal/diffuse asymmetric irregular wall thickening (15%–30%; Fig. 115)
–Polypoid intraluminal mass (15%–25%)
●Signal intensity:
–Like most other neoplasms: T1, hypointense; T2, moderately hyperintense
–Usually heterogeneous
●Contrast-enhanced images: typically illdefined enhancement in the early phase
●Gallstones commonly present
●Differential diagnosis:
–Xanthogranulomatous cholecystitis (see # 105; Chun et al. 1997)
–Adenomyomatosis
(see # 108; Gerard et al. 1990)
–Acute/chronic cholecystitis (see #96, 104)
–Metastases
(50% malignant melanoma)
–Leukemia, lymphoma
–Benign polyps
–Direct invasion of gallbladder by other tumors (e.g., hepatic, duodenal)
●Signs of extramural spread: see # 116–118
References
Chun KA, Ha HK,Yu ES et al. (1997) Xanthogranulomatous cholecystitis: CT features with emphasis on differentiation from gallbladder carcinoma. Radiology 203 : 93–97
Demachi H, Matsui O, Hoshiba K et al. (1997) Dynamic MRI using a surface coil in chronic cholecystitis and gallbladder carcinoma: radiologic and histopathologic correlation. J Comp Assist Tomogr 21 : 643–651
Franquet T, Montes M, Ruiz de Azua Y, Jimenez FJ, Cozcolluella R (1991) Primary gallbladder carcinoma: imaging findings in 50 patients with pathologic correlation. Gastrointest Radiol 16 : 143–148
Gerard PS, Berman D, Zafaranloo S (1990) CT and ultrasound of gallbladder adenomyomatosis mimicking carcinoma. J Comp Assist Tomogr 14 : 490–491
Schwartz LH, Black J, Fong Y et al. (2002) Gallbladder carcinoma: findings at MR imaging with MR cholangiopancreatography. J Comput Assist Tomogr 26 : 405–410
4 Gallbladder and Cystic Duct 237
Fig. 115. T2-weighted MR image showing asymmetric wall thickening (arrows) associated with multiple stones: carcinoma
238 4.4 Malignant Tumors
#116 Spread of Gallbladder
Carcinoma (1):
Direct Invasion
of Liver Parenchyma and/or Biliary Tree
Related topic: #89 (extrahepatic bile duct, involvement by gallbladder carcinoma)
KEY FACTS: DISEASE
●Local spread to the liver and/or biliary tree occurs in up to 80% of cases (Kumar and Aggarwal 1994)
●Mechanism: venous drainage of the gallbladder ends in adjacent liver substance
●Other routes of spread:
–Duodenum (12%) or colon (9%)
–Lymphatic (see # 117)
–Peritoneal (see # 118)
–Hematogenous (see # 118)
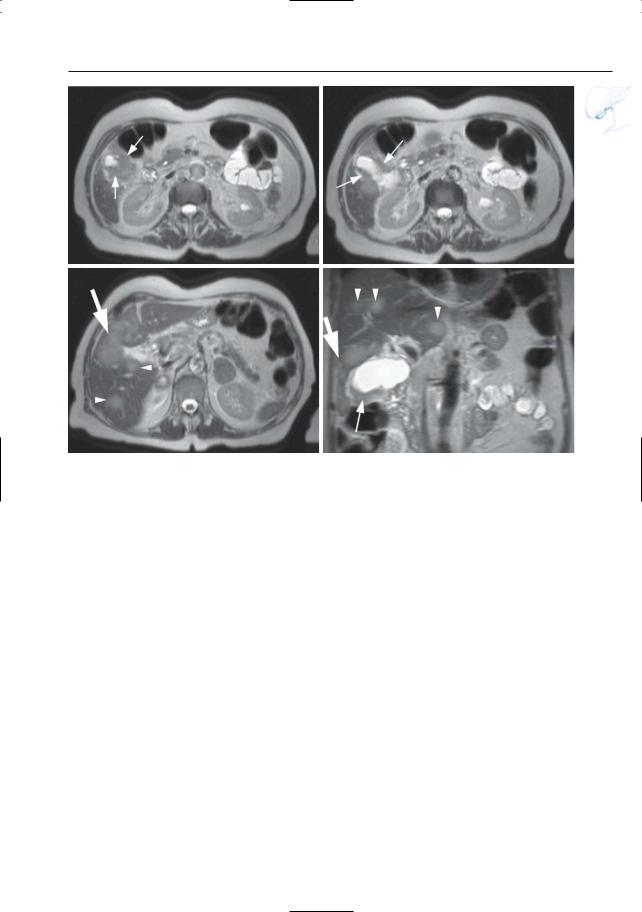
KEY FACTS: MRI (FIG. 116)
●MR features of liver invasion:
–Abnormal aspect of the gallbladder bed with absence of clear separation between the gallbladder and liver
–Soft tissue mass in hepatic parenchyma cranial to the gallbladder and/or in the liver hilum
–Narrowing of the common hepatic duct (see # 89) or intrahepatic ducts
●Differential diagnosis: e.g., cholangiocarcinoma, metastases, lymphoma, hepatocellular carcinoma
●Note: Coronal images should be obtained to evaluate intrahepatic spread
References
Kumar A, Aggarwal S (1994) Carcinoma of the gallbladder: CT findings in 50 cases.Abdom Imaging 19 : 304–308
Schwartz LH, Black J, Fong Y et al. (2002) Gallbladder carcinoma: findings at MR imaging with MR cholangiopancreatography. J Comput Assist Tomogr 26 : 405–410
Yamaguchi K,Enjoji M (1988) Carcinoma of the gallbladder. A clinicopathology of 103 patients and a newly proposed staging. Cancer 62 : 1425–1432

4 Gallbladder and Cystic Duct 239
b
a
d
c |
e |
Fig. 116 a–c. a Coronal T2-weighted image showing a large mass in the right liver lobe (arrows), discrete thickening of the gallbladder wall (arrowhead), and absence of a fatty interface between the gallbladder and liver: gallbladder carcinoma with direct hepatic invasion. b Sagittal cross-sectional image obtained in a different patient showing similar abnormalities as in a (arrows). c Same patient as in b. Projective image showing amputation of bile
ducts in the right liver lobe (arrow). d–e Different patient. Coronal T2-weighted HASTE image (TE 60) (d) showing a slightly hyperintense mass in the gallbladder fossa (large arrow), with extension into the adjacent liver parenchyma (small arrow). e Axial post-gadolinium T1-weighted VIBE images obtained in the venous phase showing ring enhancement of the intrahepatic mass (large arrow) together with focal thickening of the gallbladder wall (small arrow)

240 4.4 Malignant Tumors
|
|
|
|
KEY FACTS: MRI |
|
|
|
|
|
|
#117 Spread of Gallbladder |
|
|
|
|
||
|
|
|
|
|
|
|
|
|
|
|
Carcinoma (2): |
|
● Specific location of lymph node: see |
|
|||
|
|
Lymph Node Metastases |
|
|
||||
|
|
|
|
above |
|
|
! |
|
|
|
|
|
|
|
|||
|
|
|
|
|
|
|||
|
|
KEY FACTS: DISEASE |
● Criteria for malignancy (Ohtani et al. |
|||||
|
|
|
||||||
|
|
|
|
1993; Fig. 117): |
|
|
|
|
|
|
● Second most common route of spread, |
– Size greater than 10 mm (positive pre- |
|
||||
|
|
|
dictive value, 93%) |
|
|
|
||
|
|
after direct invasion of the liver/biliary |
|
|
|
|
||
|
|
– |
Lobulated appearance (positive pre- |
|
||||
|
|
tree |
|
|||||
|
|
|
dictive value, 93%) |
|
|
|
||
|
|
● Incidence: average 17%; 63% in stage III |
|
|
|
|
||
|
|
– |
Heterogeneous enhancement |
(posi- |
|
|||
|
|
carcinoma (i.e., carcinoma invading |
|
|||||
|
|
|
tive predictive value, 86%) |
|
|
|
||
|
|
adjacent organs such as the duodenum, |
|
|
|
|
||
|
|
● Projective images may show narrowing |
|
|||||
|
|
liver, and colon) |
|
|||||
|
|
● Anatomy: lymphatics of the gallbladder |
of the common bile duct (compression |
|
||||
|
|
by paracholedochal nodes) |
|
|
|
|||
|
|
descend around the bile duct, merge |
|
|
|
|||
|
|
● Note: Accurate preoperative assessment |
|
|||||
|
|
with lymph nodes posterior to the pan- |
|
|||||
|
|
creas, portal vein, and common hepatic |
of the extent of metastases may be useful |
|
||||
|
|
for planning radical surgery (Shirai et al. |
|
|||||
|
|
artery, and finally drain into the intera- |
|
|||||
|
|
1992; Tsukada et al. 1997) |
|
|
|
|||
|
|
ortocaval nodes (Shirai et al. 1992) |
|
|
|
|||
|
|
● Differential diagnosis: other tumors |
|
|||||
|
|
● The prevalence of metastases to the dif- |
|
|||||
|
|
ferent types of regional lymph nodes |
(e.g., pancreatic carcinoma) with lymph |
|
||||
|
|
node metastases |
|
|
|
|||
|
|
corresponds to this pathway (Ohtani et |
|
|
|
|||
|
|
al. 1993) |
|
|
|
|
|
|
|
|
● Hepatic hilar nodes usually not involved |
|
|
|
|
|
|
|
|
References |
|
|
|
|||
|
|
● According to Tsukada et al. (1997), gall- |
|
|
|
|||
|
|
|
|
|
|
|
||
|
|
bladder cancer with lymph node metas- |
Kumar A, Aggarwal S (1994) Carcinoma of the gall- |
|
||||
|
|
tases limited to the cystic and perichole- |
bladder: CT findings in 50 cases.Abdom Imaging |
|
||||
|
|
dochal lymph nodes can be cured in |
19 : 304–308 |
|
|
|
||
|
|
more than 50% of cases |
Ohtani T, Shirai Y, Tsukada K, Hatakeyama K, Muto |
|
||||
|
|
T (1993) Carcinoma of the gallbladder: CT evalu- |
|
|||||
|
|
|
|
|
||||
|
|
|
|
ation of lymphatic spread. Radiology 189 : 875– |
|
|||
|
|
|
|
880 |
|
|
|
|
|
|
|
|
Schwartz LH, Black J, Fong Y et al. (2002) Gallblad- |
|
|||
|
|
|
|
der carcinoma: findings at MR imaging with MR |
|
|||
|
|
|
|
cholangiopancreatography. J Comput |
Assist |
|
||
|
|
|
|
Tomogr 26 : 405–410 |
|
|
|
|
|
|
|
|
Shirai Y, Yoshida K, Tsukada K, Ohtani T, Muto T |
|
|||
|
|
|
|
(1992) Identification of the regional lymphatic |
|
|||
|
|
|
|
system of the gallbladder by vital staining. Br J |
|
|||
|
|
|
|
Surg 79 : 659–662 |
|
|
|
|
|
|
|
|
Tsukada K, Kurosaki I, Uchida K et al. (1997) Lymph |
|
|||
|
|
|
|
node spread from carcinoma of the gallbladder. |
|
|||
|
|
|
|
Cancer 80 : 661–667 |
|
|
|
|
4 Gallbladder and Cystic Duct 241
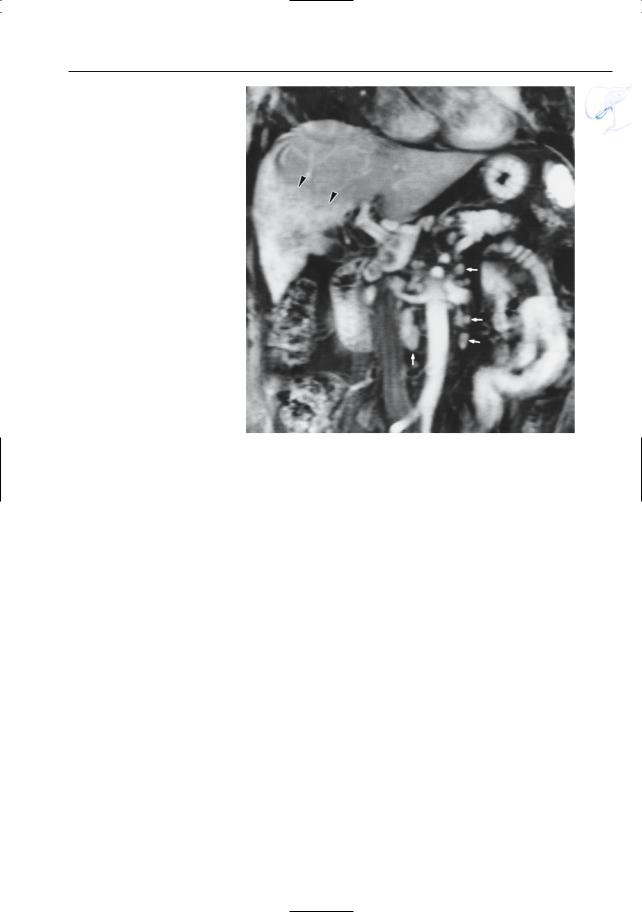
Fig.117. Contrast-enhanced image obtained in the coronal plane showing multiple enlarged retroperitoneal lymph nodes (arrows). Also note the abnormal enhancement of the caudal part of the right liver lobe secondary to invasion by the gallbladder tumor (arrowheads; same patient as in Fig. 116b, c)
242 4.4 Malignant Tumors
#118 Spread of Gallbladder
Carcinoma (3):
Other Metastases
KEY FACTS: DISEASE
●Local spread to adjacent organs such as the stomach, duodenum, and hepatic colonic flexure is relatively common
●Hematogenous spread:
–Intrahepatic dissemination may occur secondary to spread into branches of the portal vein
–Distant metastases are rare
●Peritoneal metastases: found in ± 6% (Buhr et al. 1996)
●Ovarian metastases (rare)
●Note: A problem that has arisen recently is the risk of implantation metastases following laparoscopic cholecystectomy (seeding may occur along the trocar pathways)
KEY FACTS: MRI
●Liver metastases: see #60 (Fig. 118)
●Findings in peritoneal metastatic disease:
–Ascites
–Thickening of parietal peritoneum
–Marked enhancement of peritoneum (Low et al. 1997)
References
Buhr J, Hürten M, Heinrichs CM, Graf M, Padberg WM (1996) Implantation metastases following laparoscopic cholecystectomy in gallbladder carcinoma. Dtsch Med Wochenschr 121 : 57–61
Kriplani AK, Jayant S, Kapur BML (1992) Laparoscopy in primary carcinoma of the gallbladder. Gastrointest Endosc 38 : 326–329
Low RN, Barone RM, Lacey C, Sigeti JS, Alzate GD, Sebrechts CP (1997) Peritoneal tumor: MR imaging with dilute oral barium and intravenous gadolinium-containing contrast agents compared with unenhanced MR imaging and CT. Radiology 204 : 513–520
4 Gallbladder and Cystic Duct 243
a |
b |
c |
d |
Fig. 118 a–d. Axial (a–c) and coronal (d) T2weighted HASTE image (TE 60) showing diffuse thickening of the gallbladder wall (small arrows)
with extension into the adjacent liver parenchyma (large arrow). Several hepatic metastases are seen
(arrowheads)
