
Книги по МРТ КТ на английском языке / MRI for Orthopaedic Surgeons Khanna ed 2010
.pdf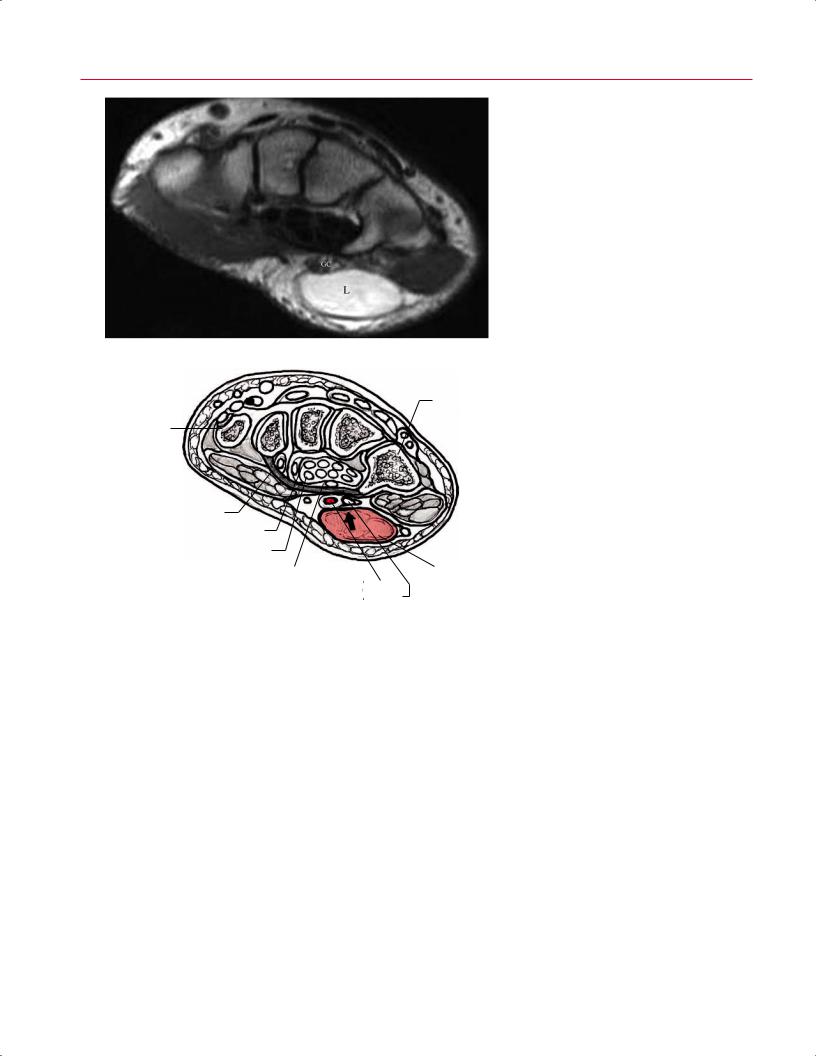
140 II Upper Extremity
Fig. 6.18 Ulnar tunnel syndrome. An axial T1weighted image (A) and artist’s sketch (B) showing a large well-circumscribed lipoma (L) compressing Guyon’s canal (GC).
A
Hamate
First metacarpal
Flexor retinaculum
Flexor digitorum profundus tendons
Flexor digitorum superficialis tendons
|
Median n. |
Lipoma |
|
|
Structures in |
Ulnar a. |
|
B |
|||
Guyon’s canal |
Ulnar n. |
the tendon sheath, lipoma, Dupuytren disease, hamartoma, peripheral nerve sheath tumor, and glomus tumor (Fig. 6.19). Although malignant soft-tissue masses are rare in the hand and wrist, MRI may show irregular features or tissue necrosis that suggest a malignant process and require additional evaluation before excision.47 Many malignant lesions, however, have a nonaggressive appearance on MR images. The value of MRI in the assessment of bone malignancies is to identify and characterize the extent of soft-tissue involvement.
Ganglion cysts can usually be diagnosed clinically with palpation and visualization. However, occult ganglions can be a cause of chronic dorsal wrist pain. Conventional radiography is usually normal. MRI may help in di erentiating ganglion cysts from synovitis in the chronically painful wrist. In
a recent study, significant di erences were found between the two entities with regard to margins, shape, specific site of involvement, dimensions, internal structure, and contrast enhancement.48 Ganglia have defined margins, a spherical shape, a septated, multilocular appearance, and wall enhancement (Fig. 6.20), whereas synovitis shows di use margins, a crescentic shape, lack of septa, and di use enhancement.48 Distinguishing these two diagnoses in the setting of chronic wrist pain has obvious implications for treatment because patients with findings of chronic synovitis typically undergo a more prolonged course of nonoperative treatment than do patients with ganglia. Approximately 30% of patients with radial-side ganglia may have associated pathology, such as interosseous ligament tears, that are detectable by MRI.49
6 The Wrist and Hand 141
A 
 B
B
|
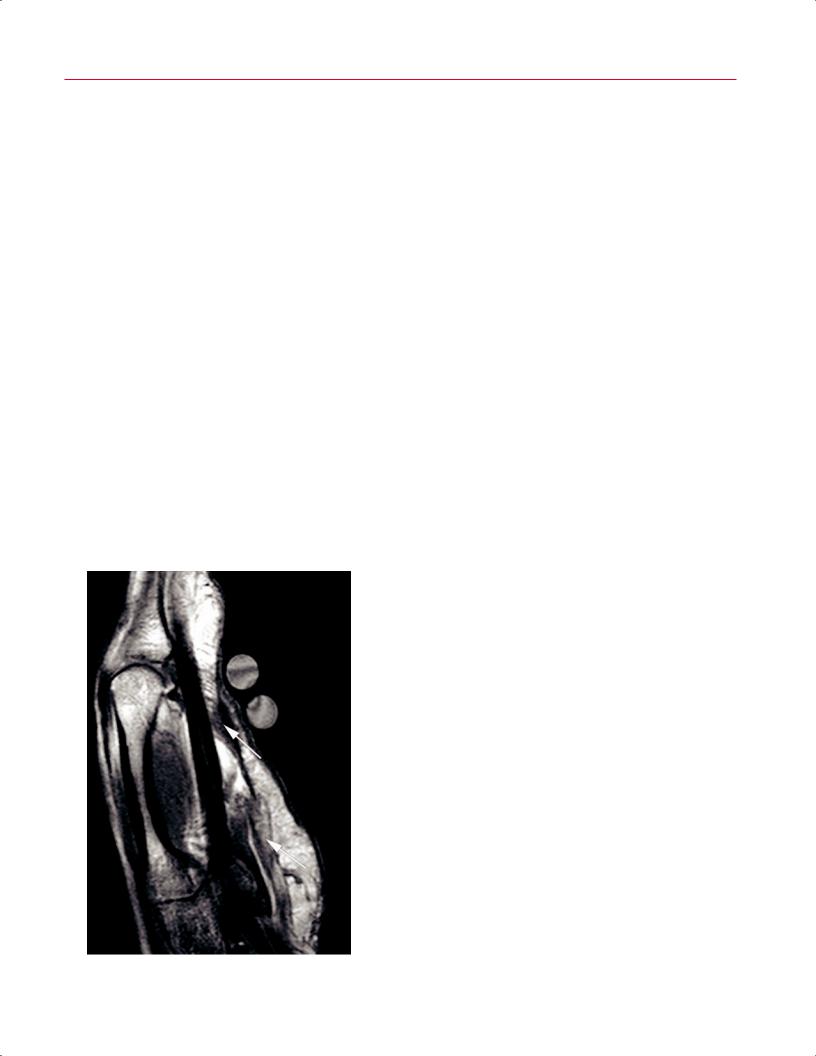
Fig. 6.19 Benign soft-tissue tumors of the hand. (A) Giant cell tumor of ten- |
|
don sheath. A sagittal T1-weighted image of the hand and digit depicting a |
|
solid mass (arrow) of mixed signal intensity originating from the underlying |
|
flexor tendon (FT). (B) Lipoma. A sagittal T1-weighted image showing a well- |
|
circumscribed lipoma (L) in the distal palm. Note how the signal characteristics |
|
of the lipoma match those of surrounding subcutaneous fat. (C) Dupuytren |
|
contracture. A sagittal T1-weighted image showing thickened palmar fascial |
|
bands (bottom arrow) and a fibrotic nodule just proximal to the MCP joint (top |
C |
arrow) in a patient with Dupuytren disease. The circular structures are fiduci- |
ary markers that delineate the site of the patient’s symptoms. |

142 II Upper Extremity
A 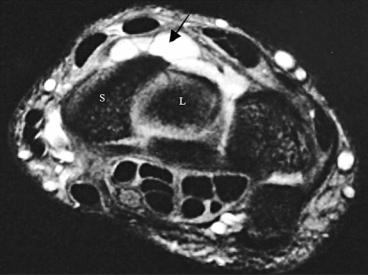
 B
B
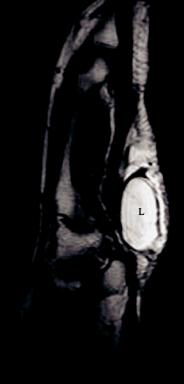
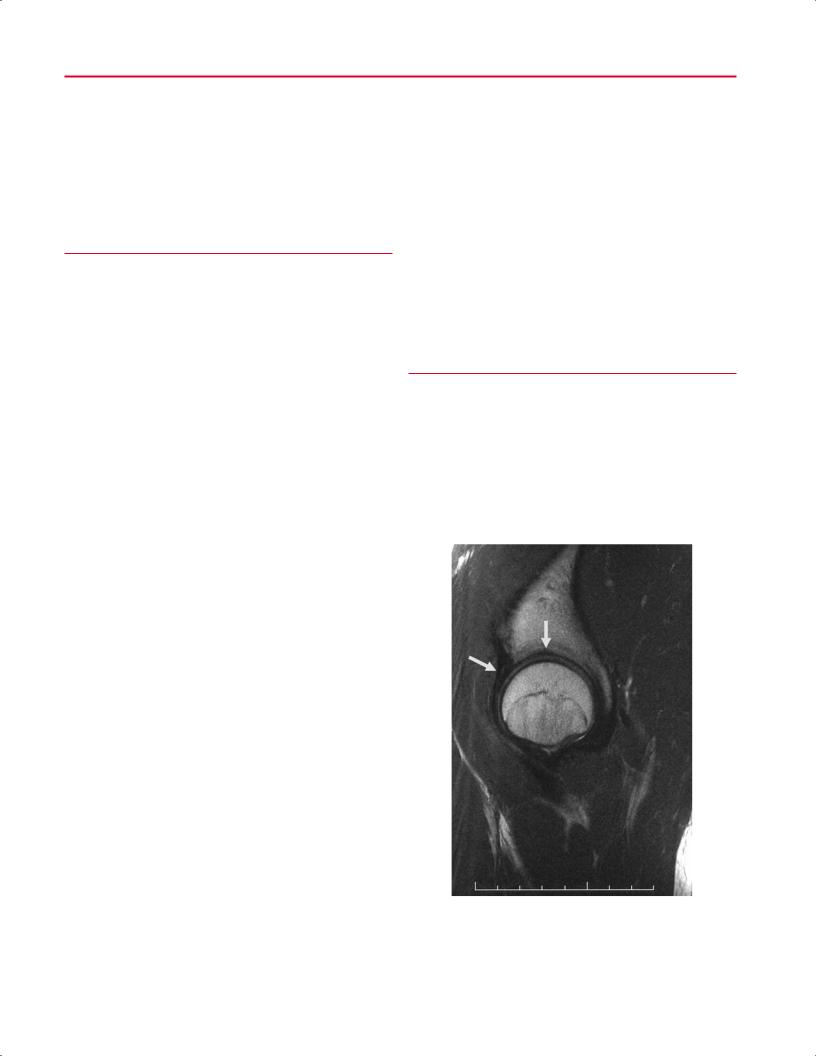
Fig. 6.20 Ganglion cyst. (A) An axial STIR image of the wrist showing a multiloculated ganglion cyst (arrow) adjacent to the dorsal margin of the scapholunate articulation. S, scaphoid; L, lunate. (B) A sagittal STIR image depicting a dorsal ganglion cyst.
References
1.Saupe N, Prüssmann KP, Luechinger R, Bösiger P, Marincek B, Weishaupt D. MR imaging of the wrist: comparison between 1.5- and 3-T MR imaging—preliminary experience. Radiology 2005;234:256– 264
2.Steinbach LS, Palmer WE, Schweitzer ME. Special focus session. MR arthrography. Radiographics 2002;22:1223–1246
3.Adey L, Souer JS, Lozano-Calderon S, Palmer W, Lee SG, Ring D. Computed tomography of suspected scaphoid fractures. J Hand Surg Am 2007;32:61–66
4.Fowler C, Sullivan B, Williams LA, McCarthy G, Savage R, Palmer A. A comparison of bone scintigraphy and MRI in the early diagnosis of the occult scaphoid waist fracture. Skeletal Radiol 1998;27:683– 687
5.Memarsadeghi M, Breitenseher MJ, Schaefer-Prokop C, et al. Occult scaphoid fractures: comparison of multidetector CT and MR imag- ing—initial experience. Radiology 2006;240:169–176
6.Senall JA, Failla JM, Bou ard JA, van Holsbeeck M. Ultrasound for the early diagnosis of clinically suspected scaphoid fracture. J Hand Surg Am 2004;29:400–405
7.Brydie A, Raby N. Early MRI in the management of clinical scaphoid fracture. Br J Radiol 2003;76:296–300
8.Hunter JC, Escobedo EM, Wilson AJ, Hanel DP, Zink-Brody GC, Mann FA. MR imaging of clinically suspected scaphoid fractures. AJR Am J Roentgenol 1997;168:1287–1293
9.Low G, Raby N. Can follow-up radiography for acute scaphoid fracture still be considered a valid investigation? Clin Radiol 2005;60:1106– 1110
10.Brooks S, Cicuttini FM, Lim S, Taylor D, Stuckey SL, Wluka AE. Cost e ectiveness of adding magnetic resonance imaging to the usual management of suspected scaphoid fractures. Br J Sports Med 2005;39:75–79
11.Saxena P, McDonald R, Gull S, Hyder N. Diagnostic scanning for suspected scaphoid fractures: an economic evaluation based on costminimisation models. Injury 2003;34:503–511
12.Lohman M, Kivisaari A, Vehmas T, et al. MR imaging in suspected acute trauma of wrist bones. Acta Radiol 1999;40:615–618
13.Spence LD, Savenor A, Nwachuku I, Tilsley J, Eustace S. MRI of fractures of the distal radius: comparison with conventional radiographs. Skeletal Radiol 1998;27:244–249
14.Futami T, Foster BK, Morris LL, LeQuesne GW. Magnetic resonance imaging of growth plate injuries: the e cacy and indications for surgical procedures. Arch Orthop Trauma Surg 2000;120:390–396

6 The Wrist and Hand 143
15.Palmer AK, Werner FW. The triangular fibrocartilage complex of the wrist—anatomy and function. J Hand Surg Am 1981;6:153–162
16.Palmer AK. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am 1989;14:594–606
17.Cooney WP. Evaluation of chronic wrist pain by arthrography, arthroscopy, and arthrotomy. J Hand Surg Am 1993;18:815–822
18.Reinus WR, Hardy DC, Totty WG, Gilula LA. Arthrographic evaluation of the carpal triangular fibrocartilage complex. J Hand Surg Am 1987;12:495–503
19.Potter HG, Asnis-Ernberg L, Weiland AJ, Hotchkiss RN, Peterson MGE, McCormack RR Jr. The utility of high-resolution magnetic resonance imaging in the evaluation of the triangular fibrocartilage complex of the wrist. J Bone Joint Surg Am 1997;79:1675–1684
20.Haims AH, Schweitzer ME, Morrison WB, et al. Limitations of MR imaging in the diagnosis of peripheral tears of the triangular fibrocartilage of the wrist. AJR Am J Roentgenol 2002;178:419–422
21.Zanetti M, Bräm J, Hodler J. Triangular fibrocartilage and intercarpal ligaments of the wrist: does MR arthrography improve standard MRI? J Magn Reson Imaging 1997;7:590–594
22.Blazar PE, Chan PSH, Kneeland JB, Leatherwood D, Bozentka DJ, Kowalchick R. The e ect of observer experience on magnetic resonance imaging interpretation and localization of triangular fibrocartilage complex lesions. J Hand Surg Am 2001;26:742–748
23.Daunt N. Magnetic resonance imaging of the wrist: anatomy and pathology of interosseous ligaments and the triangular fibrocartilage complex. Curr Probl Diagn Radiol 2002;31:158–176
24.Zlatkin MB, Chao PC, Osterman AL, Schnall MD, Dalinka MK, Kressel HY. Chronic wrist pain: evaluation with high-resolution MR imaging. Radiology 1989;173:723–729
25.Scheck RJ, Kubitzek C, Hierner R, et al. The scapholunate interosseous ligament in MR arthrography of the wrist: correlation with non-en- hanced MRI and wrist arthroscopy. Skeletal Radiol 1997;26:263– 271
26.Miller RJ. Information that orthopedists still need to know and what is missing from the MR images of the wrist. Semin Musculoskelet Radiol 2001;5:211–216
27.Shin AY, Battaglia MJ, Bishop AT. Lunotriquetral instability: diagnosis and treatment. J Am Acad Orthop Surg 2000;8:170–179
28.Ahn JM, Sartoris DJ, Kang HS, et al. Gamekeeper thumb: comparison of MR arthrography with conventional arthrography and MR imaging in cadavers. Radiology 1998;206:737–744
29.Harper MT, Chandnani VP, Spaeth J, Santangelo JR, Providence BC, Bagg MA. Gamekeeper thumb: diagnosis of ulnar collateral ligament injury using magnetic resonance imaging, magnetic resonance arthrography and stress radiography. J Magn Reson Imaging 1996;6:322–328
30.Verdan CE. Half a century of flexor-tendon surgery. Current status and changing philosophies. J Bone Joint Surg Am 1972;54:472–491
31.Hauger O, Chung CB, Lektrakul N, et al. Pulley system in the fingers: normal anatomy and simulated lesions in cadavers at MR imaging, CT, and US with and without contrast material distention of the tendon sheath. Radiology 2000;217:201–212
32.Cerezal L, del Piñal F, Abascal F, García-Valtuille R, Pereda T, Canga A. Imaging findings in ulnar-sided wrist impaction syndromes. Radiographics 2002;22:105–121
33.Berquist TH. Infection. In: Berquist TH, ed. MRI of the Hand and Wrist. Philadelphia: Lippincott Williams & Wilkins; 2003:142–152
34.Erickson SJ, Cox IH, Hyde JS, Carrera GF, Strandt JA, Estkowski LD.
E ect of tendon orientation on MR imaging signal intensity: a manifestation of the “magic angle” phenomenon. Radiology 1991;181:389–392
35.Peh WCG, Chan JHM. The magic angle phenomenon in tendons: effect of varying the MR echo time. Br J Radiol 1998;71:31–36
36.Totterman SMS, Seo GS. MRI findings of scapholunate instabilities in coronal images: a short communication. Semin Musculoskelet Radiol 2001;5:251–255
37.Lichtman DM, Mack GR, MacDonald RI, Gunther SF, Wilson JN. Kienböck’s disease: the role of silicone replacement arthroplasty. J Bone Joint Surg Am 1977;59:899–908
38.Kalainov DM, Cohen MS, Hendrix RW, Sweet S, Culp RW, Osterman AL. Preiser’s disease: identification of two patterns. J Hand Surg Am 2003;28:767–778
39.Cerezal L, Abascal F, Canga A, García-Valtuille R, Bustamante M, del Piñal F. Usefulness of gadolinium-enhanced MR imaging in the evaluation of the vascularity of scaphoid nonunions. AJR Am J Roentgenol 2000;174:141–149
40.Quinn MA, Emery P. Potential for altering rheumatoid arthritis outcome. Rheum Dis Clin North Am 2005;31:763–772
41.Rominger MB, Bernreuter WK, Kenney PJ, Morgan SL, Blackburn WD, Alarcon GS. MR imaging of the hands in early rheumatoid arthritis: preliminary results. Radiographics 1993;13:37–46
42.Sugimoto H, Takeda A, Masuyama J, Furuse M. Early-stage rheumatoid arthritis: diagnostic accuracy of MR imaging. Radiology 1996;198:185–192
43.Sugimoto H, Takeda A, Hyodoh K. Early-stage rheumatoid arthritis: prospective study of the e ectiveness of MR imaging for diagnosis. Radiology 2000;216:569–575
44.Taouli B, Guermazi A, Sack KE, Genant HK. Imaging of the hand and wrist in RA. Ann Rheum Dis 2002;61:867–869
45.Brahme SK, Hodler J, Braun RM, Sebrechts C, Jackson W, Resnick D. Dynamic MR imaging of carpal tunnel syndrome. Skeletal Radiol 1997;26:482–487
46.Frassica FJ, Khanna JA, McCarthy EF. The role of MR imaging in soft tissue tumor evaluation: perspective of the orthopedic oncologist and musculoskeletal pathologist. Magn Reson Imaging Clin North Am 2000;8:915–927
47.Teh J, Whiteley G. MRI of soft tissue masses of the hand and wrist. Br J Radiol 2007;80:47–63
48.Anderson SE, Steinbach LS, Stau er E, Voegelin E. MRI for di erentiating ganglion and synovitis in the chronic painful wrist. AJR Am J Roentgenol 2006;186:812–818
49.el-Noueam KI, Schweitzer ME, Blasbalg R, et al. Is a subset of wrist ganglia the sequela of internal derangements of the wrist joint? MR imaging findings. Radiology 1999;212:537–540

III Lower Extremity
7 The Hip
Michael K. Shindle, Bryan T. Kelly, Luis E. Moya, and Douglas N. Mintz
■Specialized Pulse Sequences and Imaging Protocols
As with MRI of any anatomic region, accurate MRI assessment of the hip requires attention to technical detail. Traditionally, MRI of the hip performed for suspicion of osteonecrosis or an occult fracture used a large body coil within the magnet bore, which provided very poor in-plane resolution and little to no detail of the articular cartilage or labrum. More recently, surface coils have been used to evaluate the hip, providing much higher spatial resolution. However, initial body coil sequences of the entire pelvis are still helpful for screening for other etiologies of pain, such as the following:
•Muscle strains
•Pelvic masses
•Hernias
•Spine and sacroiliac joint pathology
•Occult fractures
At the authors’ institution, coronal inversion recovery and axial proton-density sequences are obtained using a body coil, followed by the use of a surface coil with cartilagesensitive, intermediate TE, FSE pulse sequences in the coronal, sagittal, and axial planes, with high in-plane and segment resolution. The authors’ institution also prefers to use an intermediate TE sequence rather than T1-weighted and T2weighted images for several reasons. First, T1 is not good for evaluating cartilage because there is no contrast between fluid and cartilage. Second, it is also not good for evaluating subtle muscle abnormalities, so another sequence in each plane would be required for a thorough evaluation, and yet a third for cartilage. The intermediate TE sequence eliminates that redundancy by allowing enough signal for excellent resolution and enough contrast to evaluate all the structures (bone, ligament, tendon, muscle, and articular cartilage) and the quality of synovitis, if present. One can obtain this sequence in each plane and then add one fat-suppressed sequence to evaluate for subtle findings and assess acuity.
Many authors advocate using MR arthrography of the hip for the evaluation of labral pathology and articular cartilage (see Chapter 14),1–3 but this modality increases the cost and imaging time, and makes MRI an invasive procedure.4 Mintz et al.5 evaluated 92 patients before hip arthroscopy via an optimized protocol similar to that outlined above
and concluded that noncontrast imaging can identify labral and chondral pathology. However, many institutions in the United States and abroad continue to use MR arthrography to improve the visualization of intraarticular hip pathology, especially labral pathology.6
■Traumatic Conditions and the Athletic Hip
Acetabular Labral Tears
The fibrocartilaginous labrum (type I collagen) appears as a triangular, low signal intensity structure attached to the rim of the acetabulum7 (Fig. 7.1). Labral pathology can be a cause of substantial hip pain (Table 7.1) and is associated
Fig. 7.1 A sagittal FSE image of the hip showing a normal anterior labrum (left arrow) as a triangular focus of low signal and normal articular cartilage of the acetabulum (top arrow). (© 2009 Hospital for Special Surgery, New York, NY.)
147

148 |
III Lower Extremity |
|
|
|
Table 7.1 Di erential Diagnosis of Hip Pain |
with the development of osteoarthritis.8 The labrum sur- |
|
|
Primary labral pathology |
Nonmusculoskeletal causes |
rounds the rim of the acetabulum nearly circumferentially |
|
Femoroacetabular |
Genitourinary |
and is contiguous with the transverse acetabular ligament |
|
across the acetabular notch. The labrum is thickest superi- |
||
|
impingement |
|
|
|
Laxity |
Spine |
orly and posteriorly and widest anteriorly and superiorly. |
|
The joint capsule attaches to the acetabular rim adjacent to |
||
|
Trauma |
Psoas muscle abscess |
|
|
the labrum; however, at the superior aspect of the joint, the |
||
|
Dysplasia |
Hernia |
|
|
capsule inserts a few millimeters above the labrum, which |
||
|
Degenerative |
Endometriosis |
creates a sublabral recess or sulcus.9 Neuroreceptors that |
|
|
Ovarian cyst |
provide proprioception have been identified, and there is a |
|
|
Peripheral vascular disease |
limited blood supply to the periphery of the labrum.10,11 |
|
Primary chondral |
Unknown etiology |
Labral tears are diagnosed by the presence of increased |
|
signal intensity (often equivalent to that of synovial fluid) on |
||
|
Lateral impact |
Transient osteoporosis of |
|
|
fat-suppressed images through the substance of the labrum, |
||
|
|
the hip |
|
|
|
with or without displacement (Fig. 7.2). Partial or complete |
|
|
Subluxation/dislocation |
Bone marrow edema |
|
|
detachment is characterized by fluid-matching signal under- |
||
|
|
syndrome |
|
|
|
mining the attachment between the labrum and acetabulum. |
|
|
Osteonecrosis |
|
|
|
|
The presence of paralabral cysts should prompt careful in- |
|
|
Loose bodies |
|
|
|
|
spection of the labrum to discern the often subtle splits that |
|
|
Degeneration |
|
serve as the origin for these cysts (Fig. 7.3). Lecouvet et al.12 |
|
Primary capsule |
Synovial proliferative |
performed MRI of the hip in 200 asymptomatic individuals |
|
|
disorders |
and showed that intralabral areas of high signal intensity |
|
Laxity |
PVNS |
communicating with the free surface increased with age. |
|
Adhesive capsulitis |
Synovial chondromatosis |
To optimize outcomes, the underlying etiology of the in- |
|
Synovitis/inflammation |
Chondrocalcinosis |
jury must be identified. In addition to degenerative labral |
|
tears associated with arthritis, there are at least five causes |
||
|
Extraarticular |
Infectious/tumor/metabolic |
|
|
of labral tears13: |
||
|
Snapping hip |
Septic arthritis |
|
|
• Femoroacetabular impingement |
||
|
(internal/external) |
|
|
|
Trochanteric bursitis |
Osteomyelitis |
• Traumatic labral injury (dislocation/subluxation) |
|
Ischial bursitis |
|
• Atraumatic capsular laxity (hypermobility) |
|
|
|
|
|
Psoas bursitis |
Neoplasms |
|
|
Osteitis pubis |
Benign bone and soft tissue |
|
|
Sports hernia |
Malignant bone and soft |
|
|
|
tissue |
|
|
Piriformis syndrome |
Paget disease |
|
|
Sacroiliac joint |
Primary |
|
|
|
hyperparathyroidism |
|
|
Tendinitis |
Metastatic bone disease |
|
|
Hip flexor |
|
|
|
Adductor |
|
|
|
Abductor |
|
|
|
Gluteus medius tear |
|
|
|
Inflammatory |
Systemic |
|
|
RA |
Polyarticular |
|
|
Reiter syndrome |
Reflex sympathetic |
|
|
|
dystrophy |
|
|
Psoriatic arthritis |
Complex regional pain |
|
|
|
syndrome |
|
|
Bursitis |
Hormonal |
|
|
|
|
|
Source: From Shindle MK, Ranawat AS, Kelly BT. Diagnosis and management of traumatic and atraumatic hip instability in the athletic patient. Clin Sports Med 2006;25:309–326. Reprinted by permission.
Fig. 7.2 A sagittal FSE image of the hip showing a nondisplaced anterior labral tear (arrow). (© 2009 Hospital for Special Surgery, New York, NY.)

7 The Hip 149
Fig. 7.3 A sagittal FSE image of the hip showing paralabral cysts associated with an anterior labral tear (arrow) and full-thickness cartilage loss of the anterior acetabulum. (© 2009 Hospital for Special Surgery, New York, NY)
•Psoas impingement
•Dysplastic labral tears
Several classification systems have been used for labral tears, two of which are described here. In a cadaveric study, Seldes et al.14 determined histologically that there were two distinct types of tears (Fig. 7.4):
•Detachment of the labrum from the hyaline cartilage at the transitional zone (type 1)
•Cleavage of variable depth within the substance of the labrum (type 2)
In another study, Lage et al.15 developed an arthroscopic classification based on morphology:
•Radial flap tear
•Radial fibrillated tear
•Longitudinal peripheral tear
•Unstable tear
A recent article by Ilizaliturri et al.16 described a zone method with which to classify intraarticular pathology at hip arthroscopy (Fig. 7.5). Among a group of expert hip arthroscopists, the zone method was found to be more reproducible than the clock-face method.16
Two potential pitfalls may occur when interpreting noncontrast MRI and MR arthrography studies, potentially leading to an inaccurate diagnosis of a labral tear. First, there is a normal variant of the posteroinferior sublabral groove, which is a relatively common occurrence and typically seen on axial images.9 The clinician should recognize that this location is distinct from that of most labral tears. The second variant is a superior sublabral recess at the anterosuperior margin of the acetabulum, which has been described in the presence of mild acetabular dysplasia.17
The prevalence of labral tears in the anterosuperior labrum reportedly is high, and several authors have speculated that this tear may be secondary to decreased vascularity in this zone.13,14 In an evaluation of 12 hips from six cadavers, Kelly et al.13 used a modified Spalteholz technique to map the
Fig. 7.4 Seldes type 1 and type 2 labral tears: detachment of the labrum from the hyaline cartilage at the transitional zone and cleavage of variable depth within the substance of the labrum, respectively. (From Seldes RM, Tan V, Hunt J, Katz M, Winiarsky R, Fitzgerald RH Jr.
Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res 2001;382:232–240. Reprinted by permission.)
