
Книги по МРТ КТ на английском языке / MRI for Orthopaedic Surgeons Khanna ed 2010
.pdf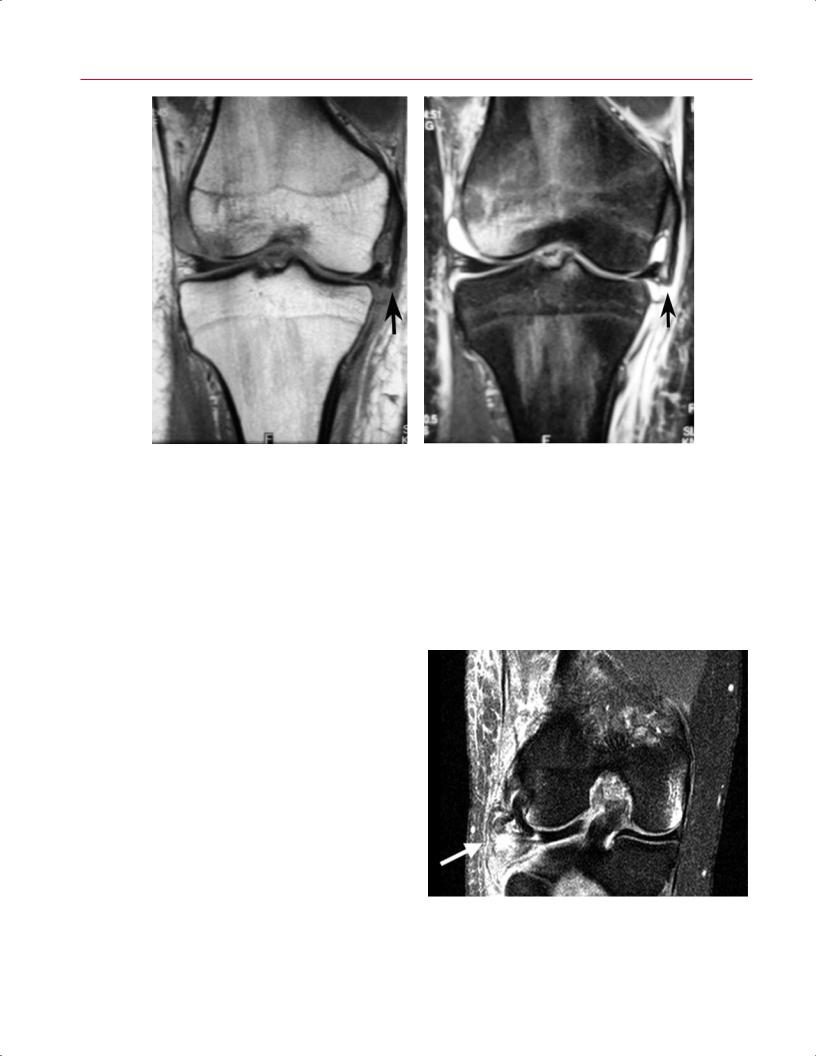
180 III Lower Extremity
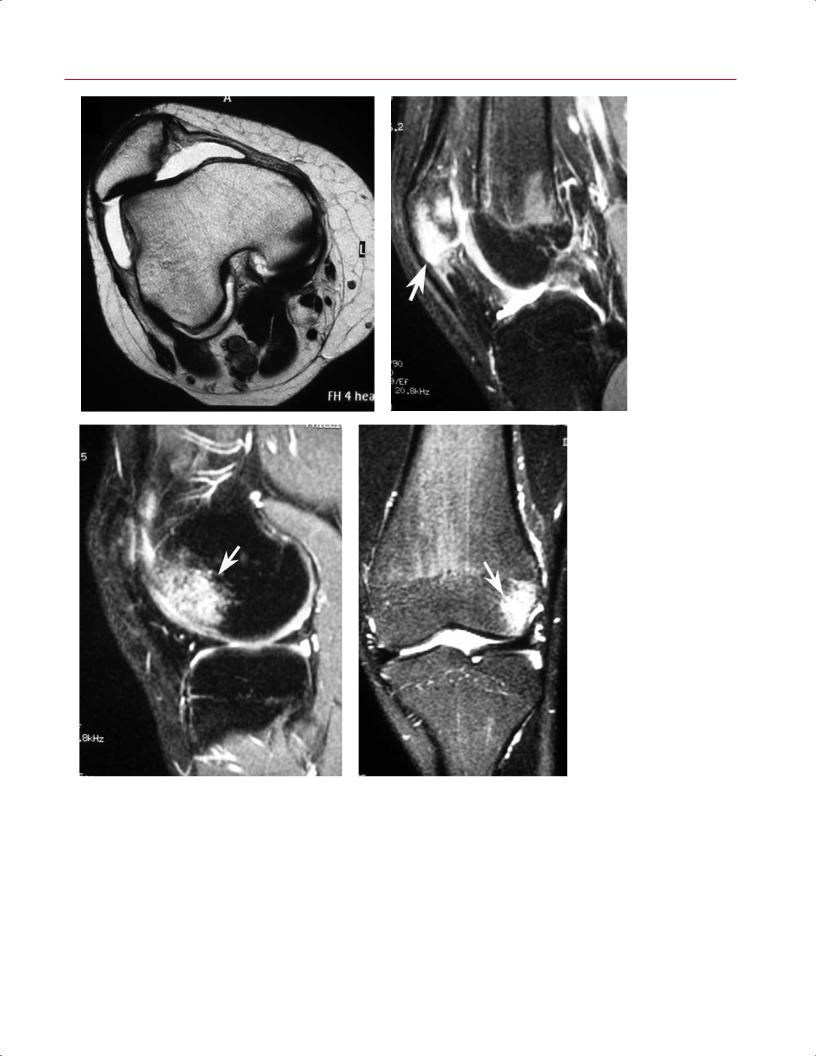
A B
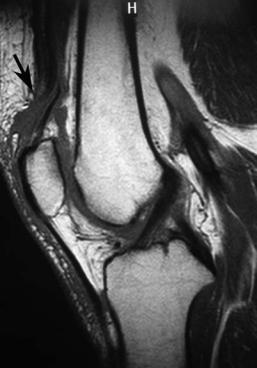
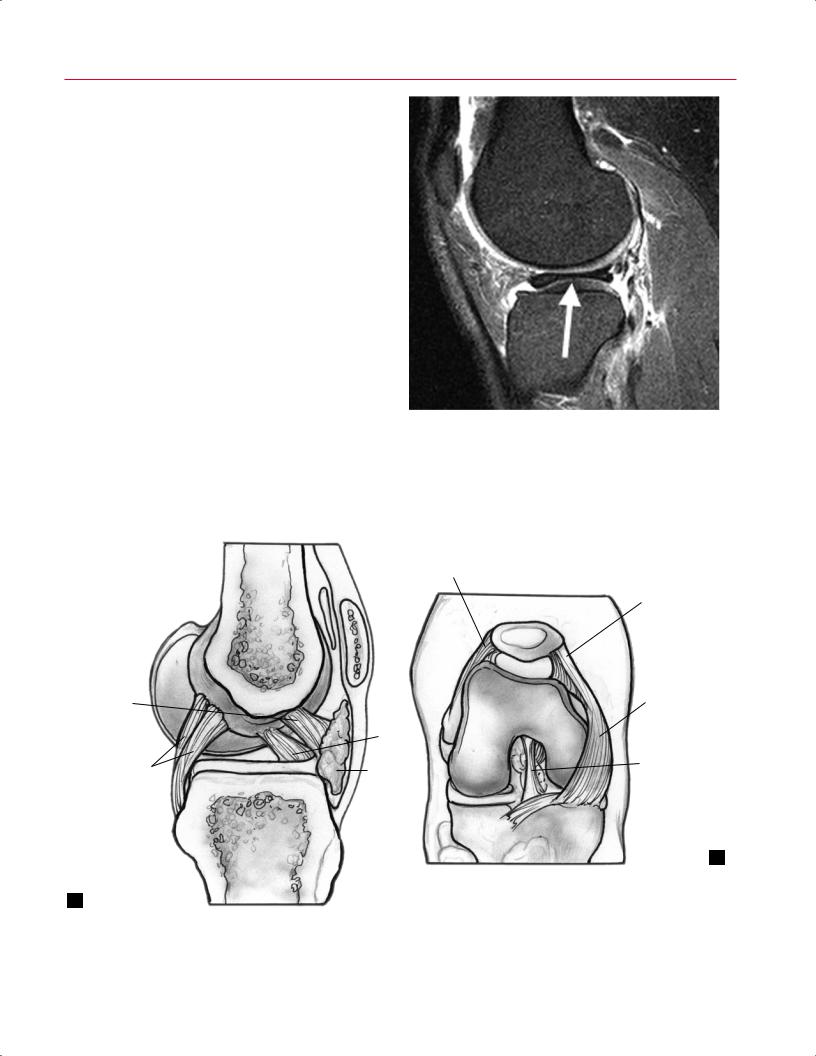
Fig. 8.25 Marked MCL injury in the right knee. Coronal T1-weighted (A) and fat-suppressed T2-weighted (B) images show a high-grade MCL injury (arrow on each). Note the marked lateral femoral condyle bone contusion.
MCL injuries comprise part of the “terrible triad”; the other two components are ACL tears and medial meniscus tears. However, it has been found that lateral meniscus tears, rather than medial meniscus tears, are more common with acute ACL tears.36
posterolateral corner injuries. Coronal oblique images o er the best imaging for evaluating and diagnosing the posterolateral structures (Fig. 8.26). Specific attention should be given to including imaging through the entire fibular head. A high-energy varus injury to the knee can place tension on, and even rupture, the peroneal nerve after the postero-
Posterolateral Corner
The posterolateral corner of the knee is complex from an anatomic and, therefore, imaging standpoint. The variability of the posterolateral structures makes the images of this area of the knee even more di cult to interpret. The posterolateral corner structures resist varus and external rotation forces. The structures that comprise the posterolateral corner are the following:
•LCL
•Arcuate ligament
•Popliteal tendon
•Lateral head of the gastrocnemius
•Posterolateral capsule
•Biceps tendon
•Meniscofibular ligament
•Popliteofibular ligament
•Fabellofibular ligament (when the fabella is present)
Although the biceps tendon and LCL usually are identifiable, identifying the popliteofibular ligament is more di cult.37 This di culty could contribute to the incidence of missed
Fig. 8.26 This coronal fat-suppressed T2-weighted image of the right knee shows tears of the fibular collateral ligament (arrow) and biceps femoris tendon at the fibular head. Note the corresponding impaction injury of the medial femoral condyle.
8 The Knee 181
A 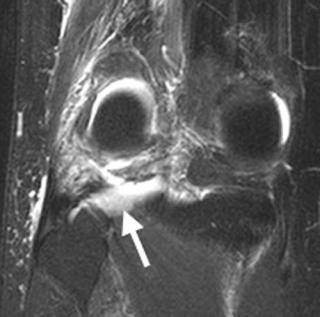 B
B
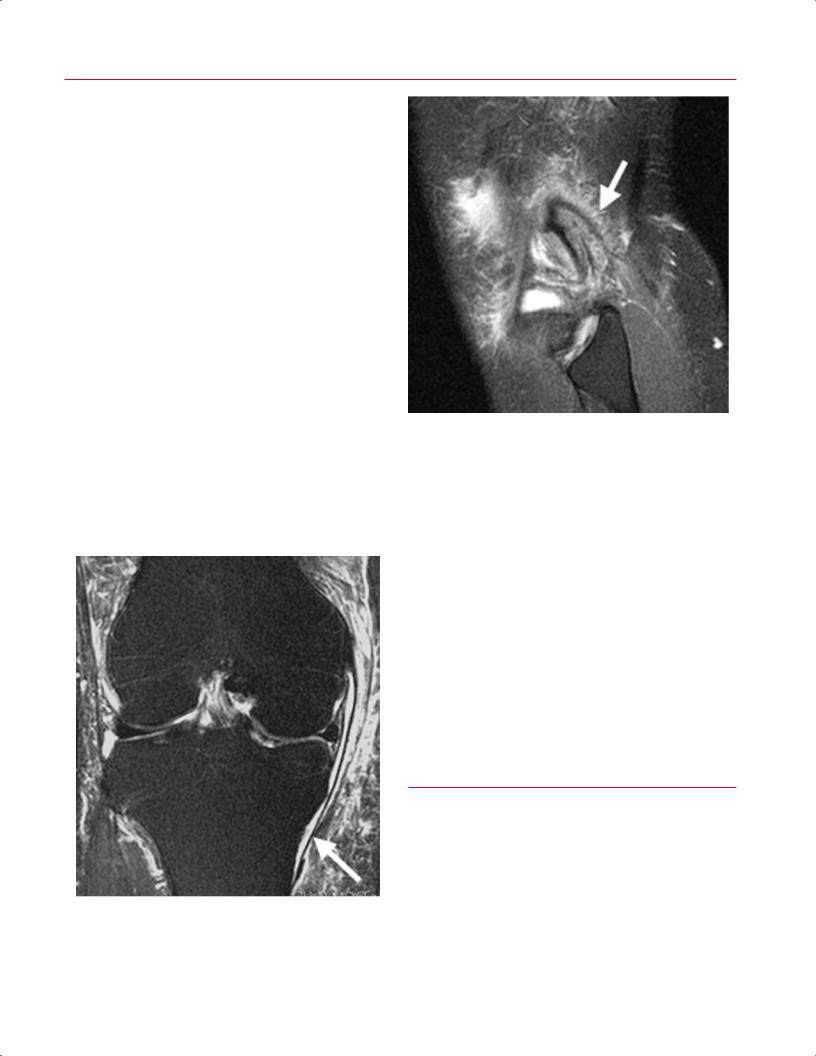
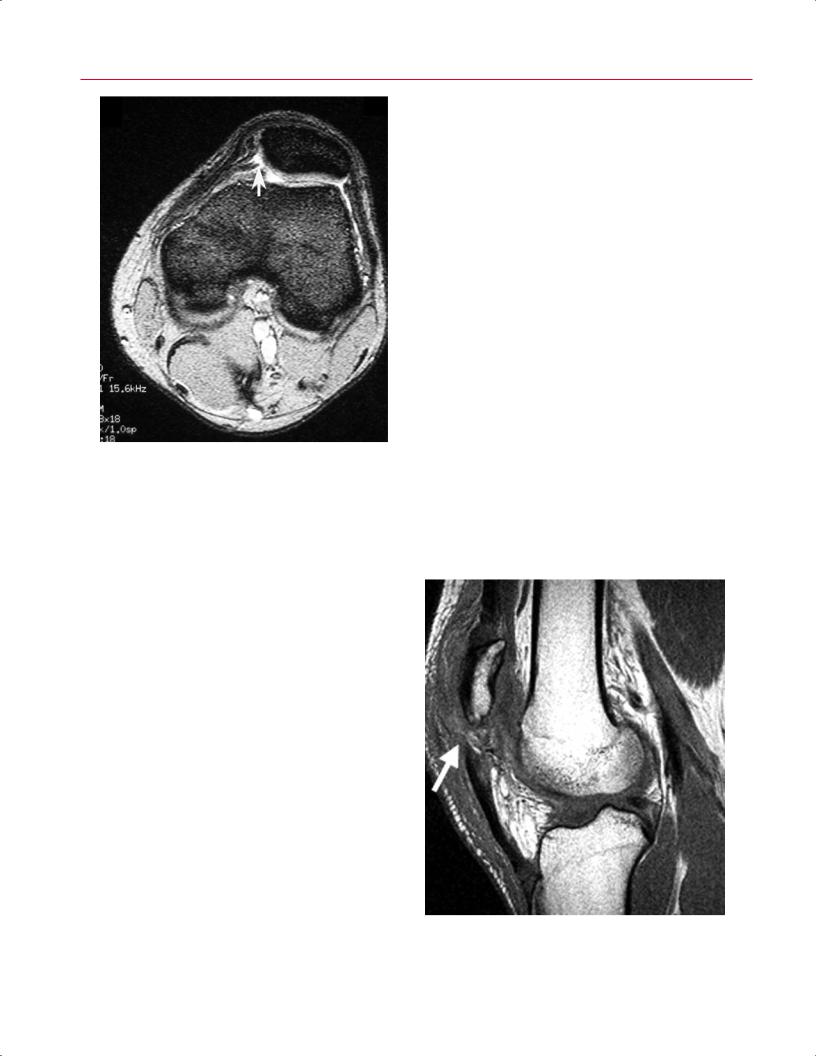
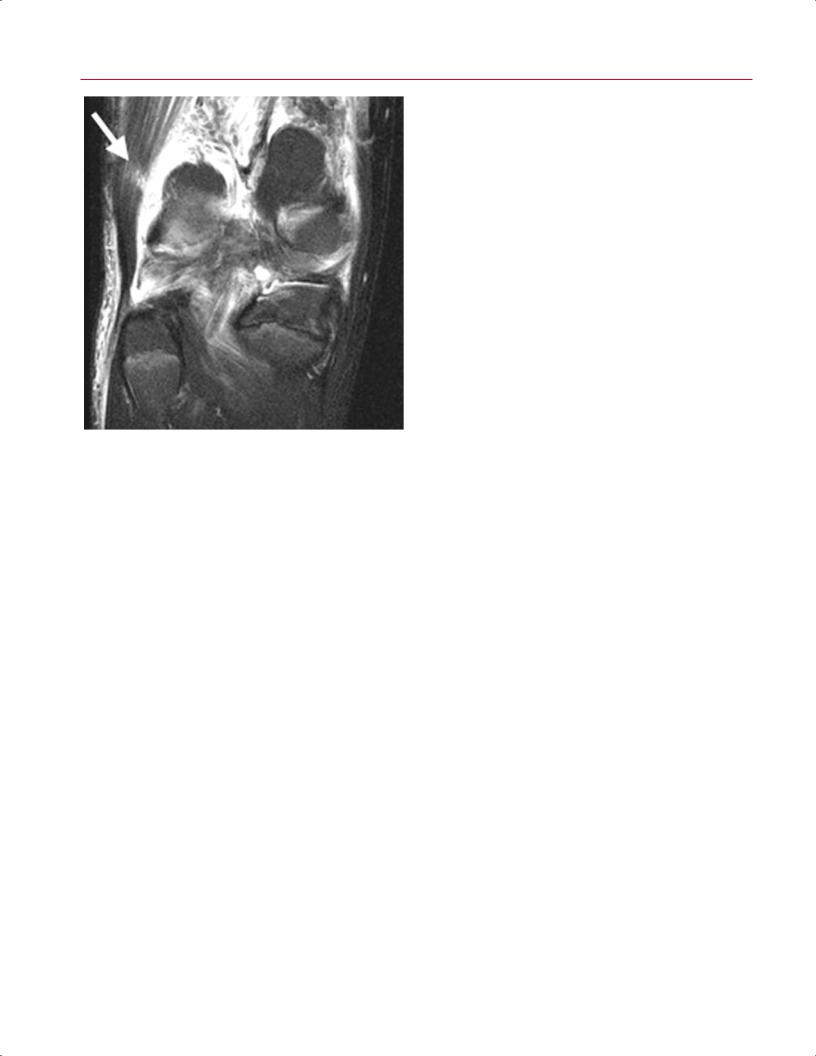
Fig. 8.27 Posterolateral corner injury in the right knee. Coronal fat-suppressed T2-weighted (A) and sagittal fat-suppressed proton-density
(B) images of a patient with an acute ACL injury show marked soft-tissue edema (arrow on each) involving the posterolateral corner of the knee.
lateral knee structures are torn. Careful attention should also be given to noting discontinuity or edema of the peroneal nerve.
The arcuate complex is composed of the LCL, arcuate liga-
Fig. 8.28 This coronal fat-suppressed T2-weighted image of a patient with an MCL sprain in the right knee shows the deep and superficial (arrow) components of the MCL complex, separated by fluid and edema.
ment, and popliteus tendon. It provides posterolateral stability of the knee to varus and rotatory stress. The arcuate ligament is an inconsistent structure and is occasionally absent in individuals with large fabellae. Injury to this complex area of the knee is seen as increased signal intensity on T2-weighted images because of the underlying edema (Fig. 8.27).
Posteromedial Corner
The posteromedial corner is composed of the deep and superficial MCLs, the posterior oblique ligament, and the oblique popliteal ligament. Damage to the posteromedial corner can cause valgus instability of the knee and increased anteromedial subluxation. The posterior oblique ligament is attached to the posterior horn of the medial meniscus. Some authors have advocated surgical repair of damage to this complex.38 Coronal images (Fig. 8.28) o er the best views of
Table 8.5 Collateral Ligament Tears
|
Grade of Tear |
Description |
MRI Appearance |
|
|
Mild |
Ligament has some |
Periligamentous |
|
|
|
torn or stretched |
edema; ligament |
|
|
|
fibers |
grossly intact, |
|
|
|
|
hematoma possible |
|
|
Moderate |
Incomplete tear with |
Partial tear with edema, |
|
|
|
no laxity |
hematoma possible |
|
|
Severe |
Loss of ligament |
Complete tear, fibers |
|
|
|
integrity, |
not in continuity, |
|
|
|
pathologic laxity |
considerable edema |
|
|
|
|
and hematoma |
|
|
|
|
|
|
182 III Lower Extremity
A B
|
Fig. 8.29 Knee dislocation. (A) A sagittal fat-suppressed T2-weighted |
|
image of the right knee shows tears of the ACL (arrowhead) and PCL |
|
(arrow). (B) A sagittal fat-suppressed T2-weighted image shows a |
|
proximal PCL tear (arrow). (C) A coronal fat-suppressed T2-weighted |
C |
image of the right knee shows severe MCL injury (arrow) and a lateral |
femoral condylar bone bruise. |
these structures. The femoral and tibial attachments of the |
of limb and even life. Vascular injury occurs in as many as |
|
structures should be evaluated carefully for increased signal |
50% of knee dislocations, whereas peroneal or tibial nerve |
|
on T2-weighted images, which indicates edema and injury. |
injuries occur in up to 30%.39,40 Although angiography is the |
|
|
standard for diagnosing vascular injuries associated with |
|
Knee Dislocation |
knee dislocations, MR angiography is less invasive and can |
|
play a valuable role (see Chapter 16). Care must be taken to |
||
|
||
Knee dislocation is a serious injury that may lead to com- |
evaluate for peroneal nerve or tibial nerve edema or discon- |
|
partment syndrome and rhabdomyolysis, with resultant loss |
tinuity. A careful neurovascular examination is essential. As |
8 The Knee 183
A B
|
Fig. 8.30 Lateral patellar |
|
dislocation. (A) An axial T2- |
|
weighted image of the right |
|
knee shows lateral patellar |
|
subluxation and chondral |
|
injury involving the medial |
|
facet of the patella. (B) A |
|
sagittal fat-suppressed T2- |
|
weighted image shows a frac- |
|
ture and bone bruise of the |
|
patella (arrow). (C) A sagittal |
|
fat-suppressed T2-weighted |
|
image shows an impac- |
|
tion-related bone bruise of |
|
the anterolateral aspect of |
|
the lateral femoral condyle |
|
(arrow). (D) A coronal fat- |
|
suppressed T2-weighted im- |
|
age of the left knee shows a |
|
lateral femoral condylar bone |
C |
D bruise (arrow). |
with many other diagnoses, the clinician has a substantial |
Extensor Mechanism |
|
advantage over the radiologist, given that the clinician can |
Traumatic injuries to the extensor mechanism include pa- |
|
correlate the clinical findings with the imaging findings to |
||
tellar dislocation, quadriceps tendon rupture, and patellar |
||
determine the most likely diagnosis with a high degree of |
||
tendon rupture.41 |
||
certainty. Knee dislocations are associated with fractures, |
||
|
||
cartilage injury, and tears of the ACL, PCL, LCL, MCL, and pos- |
Patellar Dislocation |
|
terolateral and posteromedial corners (Fig. 8.29); imaging |
||
|
||
studies should be scrutinized carefully for the presence or |
Patellar dislocations occur through noncontact mechanisms |
|
absence of these findings. |
such as rotation on a planted foot (e.g., as during batting in |
184 III Lower Extremity
Fig. 8.31 This axial fat-suppressed T2-weighted image of the left knee shows a tear (arrow) of the medial patellar retinaculum at its patellar attachment.
baseball) and through contact mechanisms (e.g., laterally directed force to the medial side of the patella). Patients can be first-time dislocators, which implies acute trauma, or recurrent dislocators, implying chronicity and instability. The MRI findings in the recurrent dislocator without a history of trauma may not be as definitive. The patella has usually already reduced by the time the MRI study has been obtained, but it is frequently subluxated laterally. Images of acute patellar dislocations commonly show bone bruises of the lateral trochlea and the medial patella (Fig. 8.30). When the patella displaces over the lateral femoral condyle, varying sizes of osteochondral fragments may be fractured from the patella or trochlea, or both. On MRI, these loose bodies may be found in the joint, and fluid–fluid levels may be seen. MRI typically reveals a rupture of the medial patellar retinaculum, including the medial patellofemoral ligament (Fig. 8.31). Noting the location of the medial patellofemoral ligament is important because it can guide decisions about repair or reconstruction and may help identify the optimal location for the incision. Edema may also be seen in the region of the vastus medialis oblique. The only clue for chronic dislocators may be an attenuation or laxity of the medial retinaculum and medial patellofemoral ligament. Large e usions are commonly seen on MRI of these injuries. MRI also can help the clinician determine the degree of predisposition to patella dislocation. For instance, a hypoplastic lateral trochlea seen on axial images suggests instability secondary to insu cient osseous constraint. Identification of these predisposing factors assists with surgical planning and determination of prognosis.
A 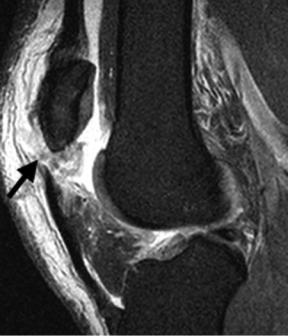 B
B
Fig. 8.32 Patellar tendon rupture. Sagittal fat-suppressed proton-density (A) and sagittal T1-weighted (B) images show a compete tear (arrow on each) of the proximal patellar tendon.

8 The Knee 185
A 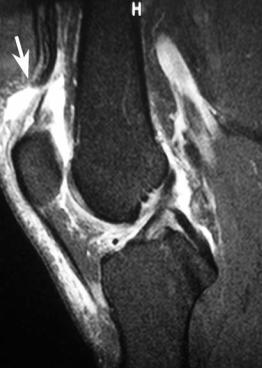
 B
B
Fig. 8.33 Quadriceps tendon rupture. Sagittal fat-suppressed T2-weighted (A) and sagittal T1-weighted (B) images show a rupture of the quadriceps tendon (arrow on each).
Quadriceps and Patellar Tendon Ruptures
The quadriceps tendon has a laminated appearance on MRI because it is formed as a conjoined structure from four muscles. Understanding this concept allows the orthopaedic surgeon to avoid misreading the normal appearance of the quadriceps tendon as an intrasubstance injury or strain of the quadriceps tendon. Partial quadriceps tendon tears often are associated with increased T2-weighted signal, especially on fat-suppressed images, just anterior to the quadriceps tendon.
Patellar tendon ruptures (Fig. 8.32) usually occur in young patients (<50 years old), whereas quadriceps tendon ruptures (Fig. 8.33) occur in older patients, in patients with comorbidities such as diabetes mellitus and obesity, and in patients on steroids. Sagittal images are ideal for visualizing both types of ruptures. Tendon discontinuity with patella alta is seen on T1-weighted sagittal images with patellar tendon rupture. Discontinuity of the tendon and patella baja can be seen in patients with quadriceps tendon rupture.42 Both types of rupture show edema on T2-weighted images. It is helpful to di erentiate an avulsion from an intratendinous failure because bone-to-bone healing allows for a better prognosis. Although the diagnosis of quadriceps and patellar tendon rupture can frequently be made by history and physical examination (including palpation of a suprapatellar or
infrapatellar defect), MRI may still provide valuable information regarding the presence or absence of other intraarticular injuries, such as cruciate ligament or meniscal tears, that may be treated at the time of ligament repair or reconstruction.
Muscle Strain
Muscle strains about the knee are common.43 The biceps femoris (Fig. 8.34) is by far the most commonly strained muscle at the knee, followed by the semimembranosus and semitendinosus muscles.44 A muscle strain is identified on MRI as a region of increased T2-weighted signal within the substance of the muscle without frank discontinuity of the muscle fibers. One third of all strains involve multiple muscles.43 The length of abnormal signal in the strained muscle is predictive of the athlete’s ability to return to play.45 Care must be taken to di erentiate an avulsion from a strain, given that avulsions often require surgical intervention.
Loose Bodies
Loose bodies are an indication for arthroscopic surgery. There are two typical sources for loose bodies:
•Osteophytes and degenerative cartilage debris in the osteoarthritic knee
186 III Lower Extremity
Fig. 8.34 This coronal fat-suppressed T2-weighted image of the right knee shows intramuscular edema (arrow), compatible with strain, involving the biceps femoris muscle.
•Osteochondral fragments from acute trauma, such as when the patella dislocates
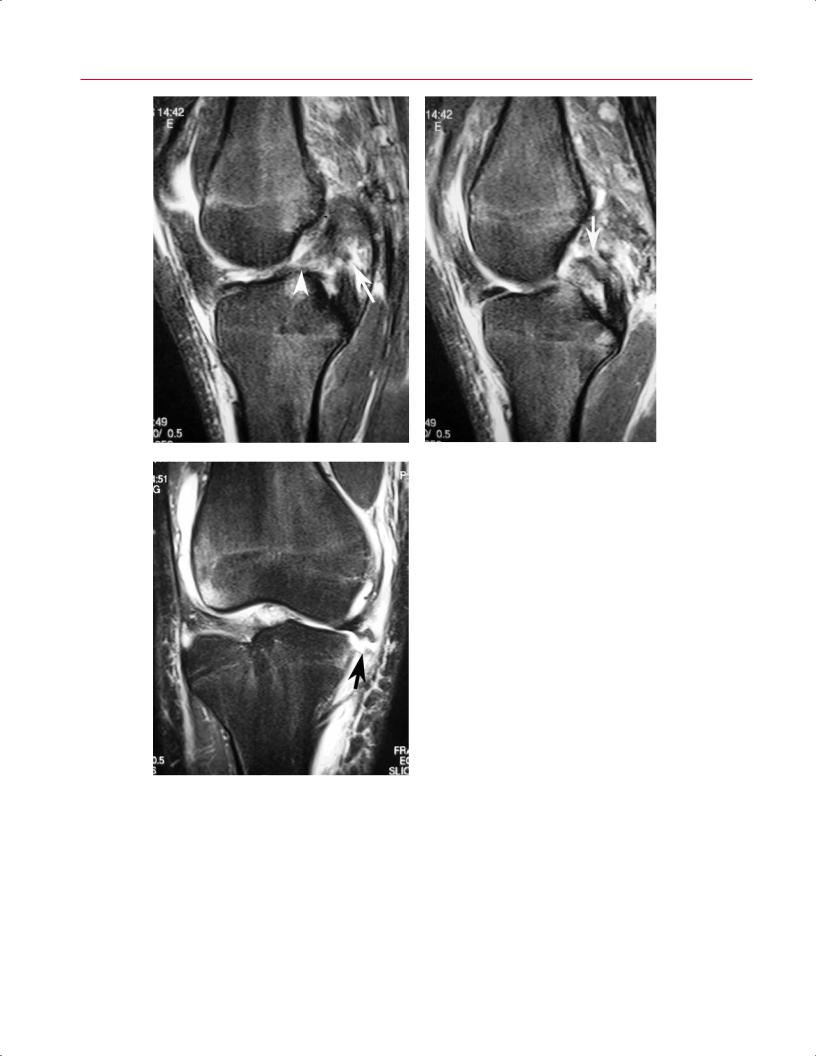
The source of the loose body sometimes is recognizable; when it is, it o ers valuable information. MRI is useful for locating chondral or osseous fragments in the knee, especially purely chondral and unmineralized lesions, which are not visible on conventional radiographs. Estimating the size of osteochondral fragments is important because the size dictates what treatment options are available. Loose bodies are found most frequently in the suprapatellar pouch, the medial and lateral gutters, and the posterior compartments46 (Fig. 8.35). A good clue that allows for diagnosis of a loose body is identification of the osteochondral donor site. Multiple loose bodies seen on MRI without evidence of donor sites may suggest synovial osteochondromatosis, a benign proliferative disorder of the synovium.
MRI and MR arthrography can be used to evaluate loose bodies, which typically have low signal on T1-weighted and T2-weighted pulse sequences. Gradient-echo images are also frequently used, especially to help di erentiate the diagnosis from PVNS. As with other diagnoses, it is important to correlate the MRI findings with those seen on conventional radiographs.
A 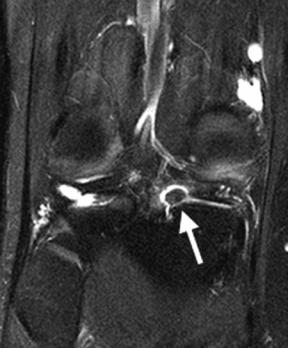
 B
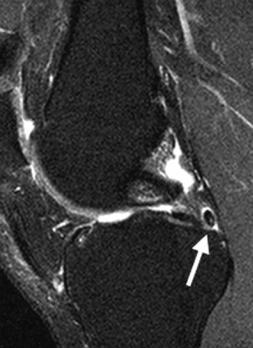
B
Fig. 8.35 Loose bodies. Coronal fat-suppressed T2-weighted (A) and sagittal fat-suppressed proton-density (B) images of the right knee show a loose body (arrow on each) located within the recess lateral to the posterior horn of the medial meniscus.

|
|
8 The Knee 187 |
||
Meniscal ossicles, which may be mistaken for loose bod- |
on conventional radiographs, especially early in the progres- |
|
||
ies, are typically located at the posterior horns of the menisci |
sion and before the sclerosis seen in the healing phase oc- |
|||
and, on MRI, appear as corticated structures with marrow |
curs. MRI findings of an acute stress fracture include a low |
|||
signal characteristics on all sequences. Meniscal ossicles are |
signal intensity line on T1-weighted images and a high signal |
|||
rare and frequently asymptomatic. Their etiology and clini- |
intensity linear region on T2-weighted images because of the |
|||
cal significance are unclear. |
presence of surrounding edema (Fig. 8.36). Although stress |
|||
|
|
fractures of the femoral neck have more severe clinical con- |
||
Ho a Disease |
sequences, stress fractures of the proximal tibia and distal |
|||
femur must be identified early and treated appropriately. |
||||
Ho a disease (fat pad disease) has been described in young |
||||
|
|
|||
athletes, usually after traumatic events.11 Acutely, edema is |
Extensor Mechanism: Patellar Tendinitis |
|||
found in the patellar fat pad and can cause pain. The fat pad |
|
|
||
may hypertrophy, and repetitive trauma and fibrosis can en- |
Also known as jumper’s knee, patellar tendinitis is a com- |
|||
sue (see Anterior Interval Scarring, below). |
mon entity in patients participating in activities requiring |
|||
|
|
explosive jumping motions, such as basketball, soccer, and |
||
|
|
volleyball. MR images may show variable amounts of focal |
||
■ Degenerative (Nonacute) |
tensity on T2-weighted images (Fig. 8.37).48,49 These partial |
|||
|
|
thickening of the tendon and associated increased signal in- |
||
Pathology |
tears usually are located at the proximal aspect of the tendon |
|||
Stress Fracture |
just distal to the inferior pole of the patella. The diagnosis |
|||
of patellar tendinitis is important because the inflammatory |
||||
|
|
|||
Stress fractures about the knee are often missed because this |
process and associated tendon degeneration may proceed to |
|||
diagnosis may not be considered.47 There may be no changes |
complete rupture. |
|||
A 
 B
B
Fig. 8.36 Stress fracture. Sagittal T1-weighted (A) and fat-suppressed proton-density (B) images show a horizontal fracture (arrow on each) of the medial tibial metaphysis in a patient with a partial medial meniscectomy. Note the surrounding bone marrow edema pattern.

188 III Lower Extremity
• Grade I (complete)
• Grade II (incomplete)
• Grade III (Wrisberg or lateral meniscal variant, i.e., a meniscus that is not secured to the posterior tibia by coronary ligaments)
Monllau et al55 described a fourth, ring-shaped type. Symptoms include a popping sensation in the knee and pain. Treatment includes arthroscopic contouring or stabilization of the discoid meniscus.
The discoid lateral meniscus is recognizable on sagittal and coronal MR images with central bridging of the anterior and posterior horns (Fig. 8.39). Particularly on sagittal images obtained through the central portion of the lateral compartment, the normally separate triangular anterior and posterior meniscal horns are connected by fibrocartilaginous tissue. The discoid meniscus may show increased signal intensity on T1-weighted images because of internal myxoid degeneration, even in children and young adults.
Plicae
Plicae are synovial folds that are embryologic remnants. Usually four plicae are described (Fig. 8.40):
Fig. 8.37 This sagittal fat-suppressed proton-density image shows thickening and abnormal signal intensity (arrow) involving the proximal patellar tendon, indicative of a partial tear (jumper’s knee).
Osteochondroses
Osgood-Schlatter Disease
Osgood-Schlatter disease is an osteochondrosis of the immature apophysis of the patellar insertion found commonly in adolescent males. The patella tendon insertion is tender to the touch. The adolescent can have severe pain with activity, especially with forceful extension of the flexed knee. MRI shows focal fragmentation of the patellar tendon insertion onto the tibia with associated edema (Fig. 8.38). Patients are treated with activity modification, rest, and occasionally casting. Very rarely, surgery is necessary to remove recalcitrant, painful fragments.
Sinding-Larsen-Johansson Disease
This entity, which is similar to but less common than OsgoodSchlatter disease, occurs at the inferior pole of the patella.
Discoid Meniscus
This entity occurs in approximately 5% of the population.50–52 The lateral meniscus is much more commonly involved than is the medial meniscus.53 Discoid menisci were first classified by Wantanabe et al54 as follows:
Fig. 8.38 This sagittal fat-suppressed proton-density image shows Osgood-Schlatter disease: thickening and abnormal signal intensity involving the distal patellar tendon (arrow); bone marrow edema and slight distraction of the tibial tubercle apophysis; and fluid accumulation and edema involving the deep infrapatellar bursa, posterior to the distal patellar tendon.
8 The Knee 189
A  B
B
Fig. 8.39 Discoid lateral meniscus. Coronal fat-suppressed T2-weighted (A) and sagittal fat-suppressed proton-density (B) images of the right knee show central bridging (arrow on each) of the anterior and posterior horns of the lateral meniscus.
Superior lateral plica
Superior medial plica
Infrapatellar |
|
Medial |
|
plica |
|
plica |
|
|
ACL |
|
|
PCL |
Fat |
Infrapatellar |
|
plica |
|||
pad |
|||
|
|
B
A
Fig. 8.40 Artist’s sketch illustrating the location of superior, inferior, and medial plicae of the knee in the sagittal (A) and coronal (B) planes.
