
Книги по МРТ КТ на английском языке / MRI for Orthopaedic Surgeons Khanna ed 2010
.pdf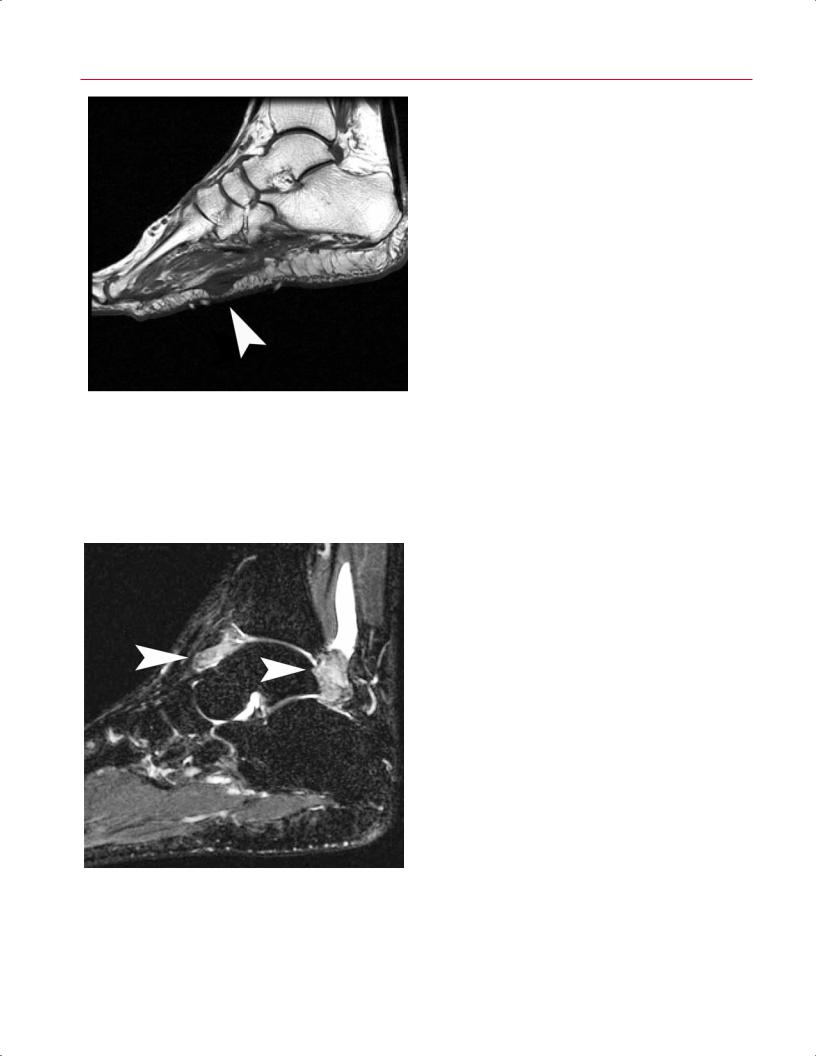
220 III Lower Extremity
A 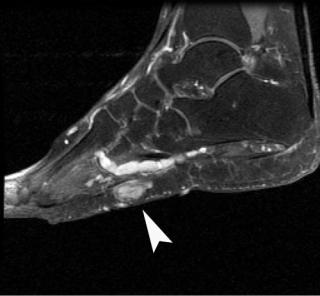 B
B
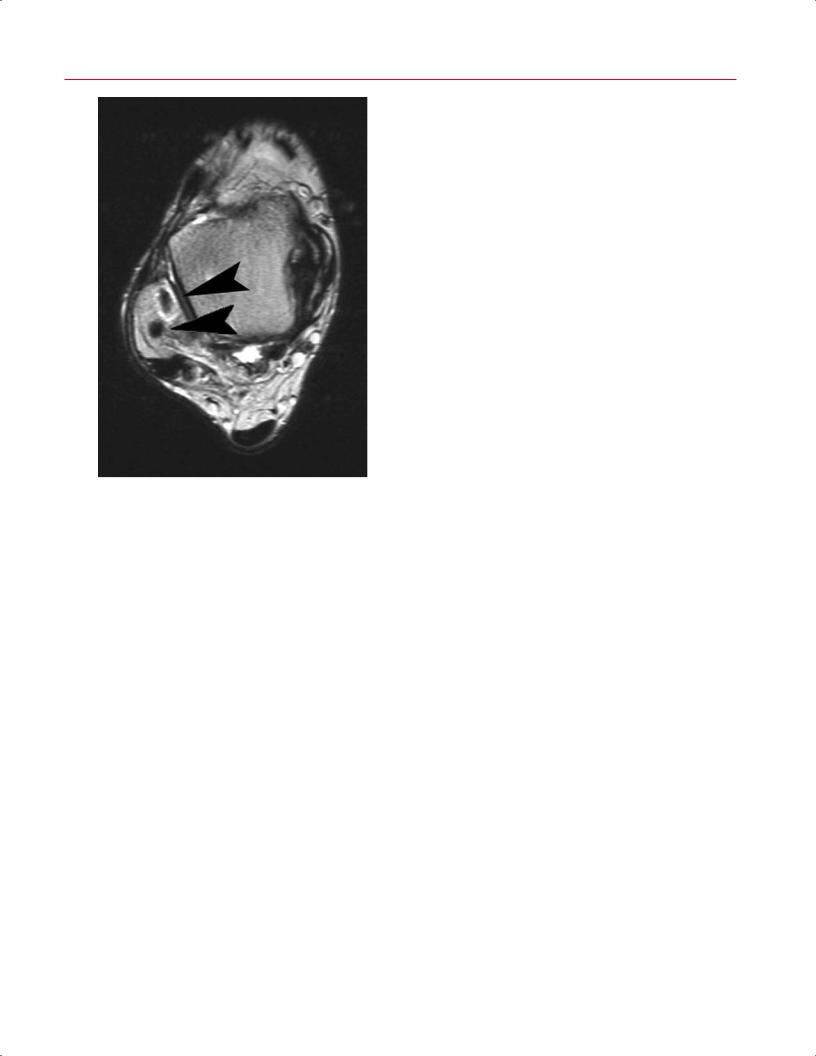
Fig. 9.31 Plantar fibromatosis is best seen on coronal and sagittal MR images of the foot. (A) The lesion typically has low to intermediate signal intensity (arrowhead) on T1-weighted images and is directly contiguous to the plantar fascia. (B) On T2-weighted images, there is
low to intermediate signal and soft-tissue edema and/or signal alternation in the deep musculature. On this fat-suppressed T2-weighted image, the signal within the mass (arrowhead) seems relatively high because of fat suppression.
tendon sheath predominantly a ects the peroneal and flexor tendon sheaths. The MRI appearance is similar to that of intraarticular PVNS, but the lesion is typically less di use and more defined.53
The more common benign bone tumors involving the foot and ankle are the following:
•Simple bone cyst
•Aneurysmal bone cyst
•Intraosseous lipoma
•Giant cell tumor
•Enchondroma
•Osteoid osteoma
Malignant bone tumors of the foot and ankle are rare, but metastasis, Ewing sarcoma, chondrosarcoma, and osteosarcoma are occasionally seen in this region.
Fig. 9.32 A sagittal fat-suppressed T2-weighted image of the ankle in a patient with PVNS shows heterogeneous signal intensity within a region of synovial proliferation in the anterior (left arrowhead) and posterior (right arrowhead) tibiotalar joint. There is also a large posterosuperior extension of the synovial space.
Plantar Fasciitis
Plantar fasciitis is a degenerative condition that occurs at the origin of the medial calcaneal tuberosity.54 Less commonly, it can also occur secondary to an enthesopathy from systemic disease (such as RA, diabetes, or lupus) or after trauma, but typically it does not involve an inflammatory infiltrate, so “fasciitis” is a misnomer. The diagnosis is usually made clinically. Patients typically complain of pain at the plantar medial aspect of the heel that is severe first thing in the morning, after prolonged sitting, and toward the end of the
9 The Foot and Ankle 221
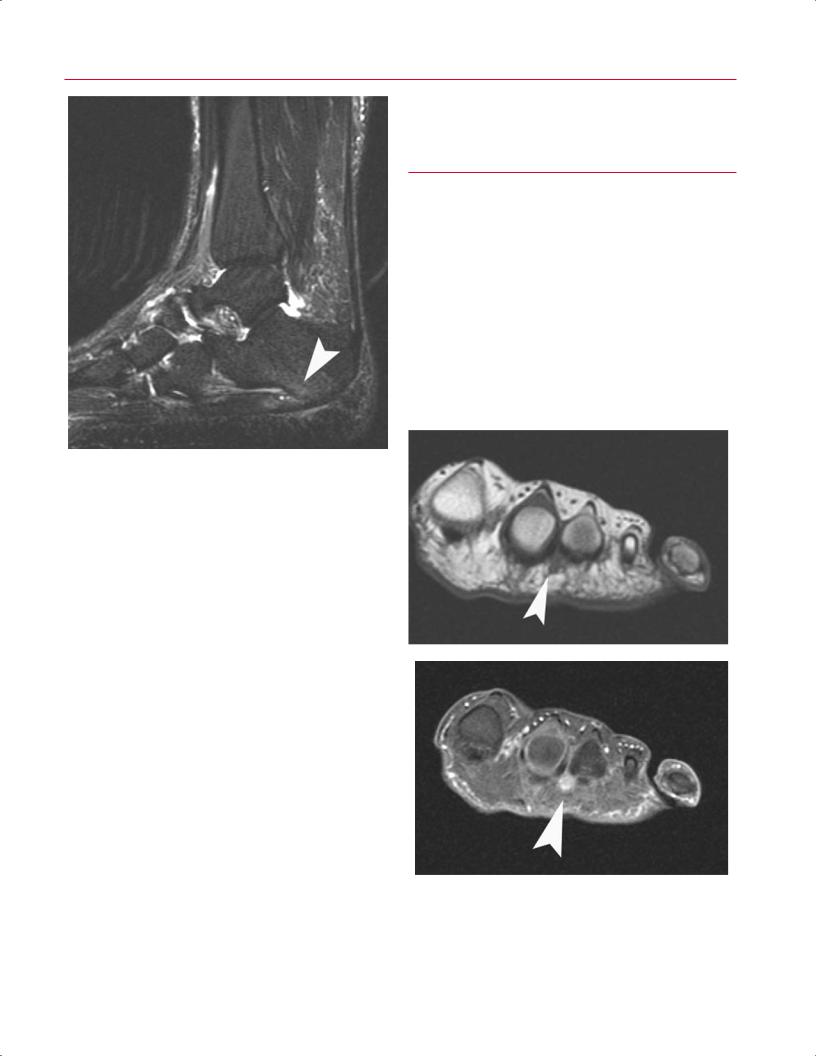
Fig. 9.33 A sagittal fat-suppressed T2-weighted image of a patient with plantar fasciitis, showing thickening of the fascia at its origin, intrasubstance changes, and edema of the calcaneus (arrowhead).
day after activity. The patient has point tenderness at the medial edge of the calcaneal tuberosity. Although not necessary at early presentation, MRI may be useful in di erentiating plantar fasciitis from other conditions such as calcaneal stress fractures. Sagittal images are most helpful in assessing the plantar fascia. MRI shows thickening of the fascia at its origin, intrasubstance changes, and sometimes edema of the calcaneus (Fig. 9.33).
metatarsal ligament.58 The neuroma is isointense compared with muscle on T1-weighted images and hypointense to fat on non–fat-suppressed T2-weighted images.58
■ Postoperative Findings
Although radiography remains the predominant postoperative imaging modality for the ankle and foot, the excellent soft-tissue contrast of MRI is particularly useful for assessment after ligament and tendon surgery.
Tendon Repair
The treatment of tendon injuries consists primarily of immobilization and surgical reconnection of the apposed tendon ends. During the first month after tendon repair, granulation tissue bridges the anastomosis (week 1), followed by increased vascularization of the paratenon zone (week 2),
A
Morton Neuroma
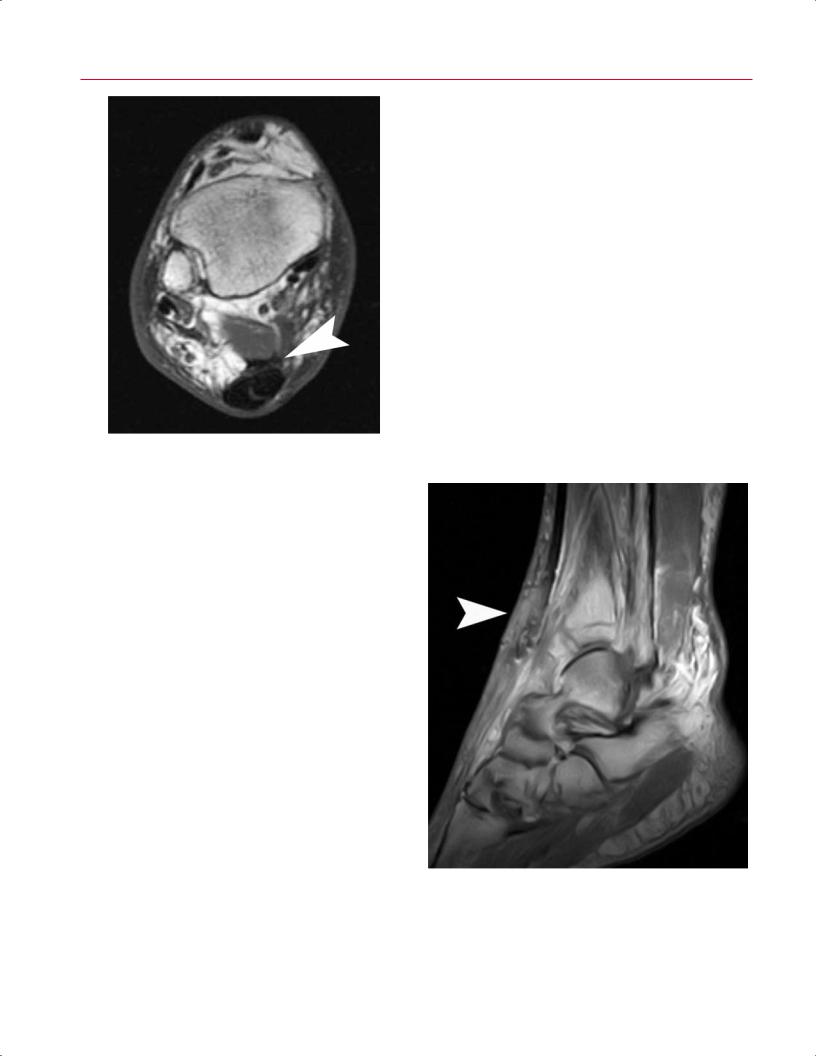
Morton neuroma refers to entrapment or impingement of an interdigital nerve between two adjacent metatarsals near the MTP joint.55 The nerve emerges from beneath the intermetatarsal ligament to bifurcate and course distally to the two adjacent toes at that web space. It most commonly a ects the third interspace; the second interspace is the second most often a ected area.56 The patient typically complains of stabbing, burning, or radiating pain and often numbness in the corresponding toes.57 Histologically, the nerve shows thickening, perineural fibrosis, and axonal demyelination.57 MRI can be a useful diagnostic adjunct to clinical examination because conventional radiographs do not image the soft tissues e ectively. Axial images are best for evaluating the interspaces (Fig. 9.34). On cross-sectional imaging, the nerve appears enlarged and spindle-shaped plantar to the inter-
B
Fig. 9.34 Morton neuroma. (A) A coronal T1-weighted image of the left foot shows a small nodular mass (arrowhead) plantar to the intermetatarsal ligament connecting the second and third metatarsals.
(B) A coronal fat-suppressed T2-weighted image of the same patient shows relative hyperintensity of the lesion (arrowhead).
222 III Lower Extremity
Fig. 9.35 An axial T1-weighted image of the right ankle showing an intact anastomosis (arrowhead) between the FHL and the Achilles tendon after tendon transfer surgery for Achilles repair.
collagen fibril formation (week 3), and, ultimately, the resolution of edema (week 4).59 In cases where tendon rupture is left untreated for extended periods of time, the muscle becomes retracted and grafting may be required.60 In such cases, available grafting strategies include free tendon grafts, tendon lengthening, and tendon transfers.
In the early postoperative period, the repaired tendon appears to be thickened.59 In the late postoperative period, the principal findings can include generalized thickening and moderate heterogeneity of signal.61 In the presence of a tendon transfer, the postoperative MR appearance includes nonanatomic connections between the relevant tendons (Fig. 9.35). Recurrent and new tears can be diagnosed as new areas of focal high signal on proton-density and T2-weighted images. T1-weighted images can also be reviewed for anatomic detail (Fig. 9.36). Comparison with previous studies is often useful for distinguishing postoperative intrasubstance changes and degeneration from re-tears. Postoperative infections such as abscess formation and osteomyelitis are best imaged using sequences before and after contrast enhancement.
Lateral Ankle Ligament Reconstruction
Surgical reconstruction of the lateral ligament complex is indicated for patients with chronic lateral instability as a sequela of ankle sprain.62 In such cases, knowledge of the relevant surgical procedure is essential because the post-
operative appearance is characterized by nonanatomic anastomoses and osseous tunnels.63 In the modified Evans procedure, the peroneus brevis tendon is transected, passed through a fibular tunnel, and anastomosed at the transaction site.63 In the Lee procedure, the peroneus brevis is transected proximally, and the distal portion is looped through a fibular tunnel and anastomosed to its distal portion. The proximal peroneus brevis is then anastomosed to the peroneus longus.63 In the Watson-Jones procedure, the peroneus brevis tendon is transected proximally, looped through two fibular tunnels and a tarsal tunnel, and sutured to itself distally.63 As in the Lee procedure, the proximal portion is anastomosed to the peroneus longus. In the Christman-Sook procedure, the peroneus brevis is split, and the free half is passed beneath the talar periosteum, fibula tunnel, and calcaneal periosteum where it is anastomosed to the tethered portion of the peroneus brevis and adjacent peroneus longus in the region of the distal fibula (Fig. 9.37).63
Other Foot and Ankle Surgical Procedures
Other common surgical procedures of the foot and ankle include plantar fasciotomy, tarsal tunnel surgery, arthrod-
Fig. 9.36 A sagittal T1-weighted image showing several foci of susceptibility artifact within the anterior tibialis tendon, suggestive of previous repair. In addition, there is discontinuity within the anterior tibialis tendon (arrowhead), representing recurrent tear with some retraction.
9 The Foot and Ankle 223
A  B
B
Fig. 9.37 Postoperative imaging in lateral ankle ligament reconstruction in a patient after a Chrisman-Snook procedure. (A) An axial T1-weighted image of the right ankle showing the split peroneus brevis tendon traversing two osseous tunnels through the fibula (ar-
esis, and hallux valgus repair.59 After fasciotomy, the plantar fascia is thickened with indistinct margins, with a lack of the fascial edema that characterizes plantar fasciitis.64 After tarsal tunnel surgery, MR shows scarring of the subcutaneous fat and fascia medial to the tarsal tunnel visible as abnormal areas of low T1 signal.54 Postoperative imaging after arthrodesis typically involves using radiography
rowheads). (B) A sagittal T1-weighted image showing the split peroneus brevis tendon traversing through additional tunnels traversing the talus (black arrowhead) and calcaneus (white arrowhead).
or CT to assess the extent of osseous fusion, although MRI can be useful for assessing soft-tissue complications such as infection, secondary degenerative changes, and tendinous and ligamentous stability. Lastly, MR is a useful adjunct in postoperative assessment of hallux valgus repair to evaluate for complications such as infection, osteonecrosis, and nonunion.59
References
1.Tocci SL, Madom IA, Bradley MP, Langer PR, DiGiovanni CW. The diagnostic value of MRI in foot and ankle surgery. Foot Ankle Int 2007;28:166–168
2.Rosenberg ZS, Beltran J, Bencardino JT. From the RSNA Refresher Courses. MR imaging of the ankle and foot. Radiographics 2000;20(Suppl 1):S153–S179
3.Bauer JS, Banerjee S, Henning TD, Krug R, Majumdar S, Link TM. Fast high-spatial-resolution MRI of the ankle with parallel imaging using GRAPPA at 3 T. AJR Am J Roentgenol 2007;189:240–245
4.Barr C, Bauer JS, Malfair D, et al. MR imaging of the ankle at 3 Tesla and 1.5 Tesla: protocol optimization and application to cartilage, ligament and tendon pathology in cadaver specimens. Eur Radiol 2007;17:1518–1528
5.Cerezal L, Abascal F, García-Valtuille R, Canga A. Ankle MR arthrography: how, why, when. Radiol Clin North Am 2005;43:693–707
6.Morrison WB. Magnetic resonance imaging of sports injuries of the ankle. Top Magn Reson Imaging 2003;14:179–197
7.Pinar H, Akseki D, Kovanlikaya I, Araç S, Bozkurt M. Bone bruises detected by magnetic resonance imaging following lateral ankle sprains. Knee Surg Sports Traumatol Arthrosc 1997;5:113– 117
8.Schneck CD, Mesgarzadeh M, Bonakdarpour A. MR imaging of the most commonly injured ankle ligaments. Part II. Ligament injuries. Radiology 1992;184:507–512
9.Fong DTP, Hong Y, Chan LK, Yung PSH, Chan KM. A systematic review on ankle injury and ankle sprain in sports. Sports Med 2007;37:73– 94
10.Clanton TO, Schon LC. Athletic injuries to the soft tissues of the foot and ankle. In: Mann RA, Coughlin MJ, eds. Surgery of the Foot and Ankle. St. Louis: Mosby-Year Book; 1993:1095–1224

224 III Lower Extremity
11.Nielson JH, Gardner MJ, Peterson MGE, et al. Radiographic measurements do not predict syndesmotic injury in ankle fractures: an MRI study. Clin Orthop Relat Res 2005;436:216–221
12.Oae K, Takao M, Naito K, et al. Injury of the tibiofibular syndesmosis: value of MR imaging for diagnosis. Radiology 2003;227:155–161
13.Boytim MJ, Fischer DA, Neumann L. Syndesmotic ankle sprains. Am J Sports Med 1991;19:294–298
14.Edwards GS Jr, DeLee JC. Ankle diastasis without fracture. Foot Ankle 1984;4:305–312
15.Flick AB, Gould N. Osteochondritis dissecans of the talus (transchondral fractures of the talus): review of the literature and new surgical approach for medial dome lesions. Foot Ankle 1985;5:165–185
16.Berndt AL, Harty M. Transchondral fractures (osteochondritis dissecans) of the talus. J Bone Joint Surg Am 1959;41:988–1020
17.Canale ST, Belding RH. Osteochondral lesions of the talus. J Bone Joint Surg Am 1980;62:97–102
18.Raikin SM, Elias I, Zoga AC, Morrison WB, Besser MP, Schweitzer ME. Osteochondral lesions of the talus: localization and morphologic data from 424 patients using a novel anatomical grid scheme. Foot Ankle Int 2007;28:154–161
19.Scranton PE Jr, McDermott JE. Treatment of type V osteochondral lesions of the talus with ipsilateral knee osteochondral autografts. Foot Ankle Int 2001;22:380–384
20.Mintz DN, Tashjian GS, Connell DA, Deland JT, O’Malley M, Potter HG. Osteochondral lesions of the talus: a new magnetic resonance grading system with arthroscopic correlation. Arthroscopy 2003;19:353– 359
21.Stroud CC, Marks RM. Imaging of osteochondral lesions of the talus. Foot Ankle Clin 2000;5:119–133
22.De Smet AA, Fisher DR, Burnstein MI, Graf BK, Lange RH. Value of MR imaging in staging osteochondral lesions of the talus (osteochondritis dissecans): results in 14 patients. AJR Am J Roentgenol 1990;154:555–558
23.Dipaola JD, Nelson DW, Colville MR. Characterizing osteochondral lesions by magnetic resonance imaging. Arthroscopy 1991;7:101– 104
24.Lahm A, Erggelet C, Steinwachs M, Reichelt A. Arthroscopic management of osteochondral lesions of the talus: results of drilling and usefulness of magnetic resonance imaging before and after treatment. Arthroscopy 2000;16:299–304
25.Higashiyama I, Kumai T, Takakura Y, Tamail S. Follow-up study of MRI for osteochondral lesion of the talus. Foot Ankle Int 2000;21:127– 133
26.Pester S, Smith PC. Stress fractures in the lower extremities of soldiers in basic training. Orthop Rev 1992;21:297–303
27.Matheson GO, Clement DB, McKenzie DC, Taunton JE, Lloyd-Smith DR, Macintyre JG. Scintigraphic uptake of 99mTc at non-painful sites in athletes with stress fractures. The concept of bone strain. Sports Med 1987;4:65–75
28.Weinfeld SB, Haddad SL, Myerson MS. Metatarsal stress fractures. Clin Sports Med 1997;16:319–338
29.Khoury NJ, El-Khoury GY, Saltzman CL, Brandser EA. MR imaging of posterior tibial tendon dysfunction. AJR Am J Roentgenol 1996;167:675–682
30.Rosenberg ZS, Cheung Y, Jahss MH, Noto AM, Norman A, Leeds NE. Rupture of posterior tibial tendon: CT and MR imaging with surgical correlation. Radiology 1988;169:229–235
31.Schweitzer ME, Karasick D. MR imaging of disorders of the posterior tibialis tendon. AJR Am J Roentgenol 2000;175:627–635
32.Khoury NJ, El-Khoury GY, Saltzman CL, Kathol MH. Peroneus longus and brevis tendon tears: MR imaging evaluation. Radiology 1996;200:833–841
33.Khoury NJ, El-Khoury GY, Saltzman CL, Brandser EA. Rupture of the anterior tibial tendon: diagnosis by MR imaging. AJR Am J Roentgenol 1996;167:351–354
34.Erickson SJ, Cox IH, Hyde JS, Carrera GF, Strandt JA, Estkowski LD. E ect of tendon orientation on MR imaging signal intensity: a manifestation of the “magic angle” phenomenon. Radiology 1991; 181:389–392
35.Puddu G, Ippolito E, Postacchini F. A classification of Achilles tendon disease. Am J Sports Med 1976;4:145–150
36.Kvist M. Achilles tendon injuries in athletes. Sports Med 1994;18:173– 201
37.Rosenberg ZS. Chronic rupture of the posterior tibial tendon. Magn Reson Imaging Clin N Am 1994;2:79–87
38.Sobel M, Geppert MJ, Olson EJ, Bohne WH, Arnoczky SP. The dynamics of peroneus brevis tendon splits: a proposed mechanism, technique of diagnosis, and classification of injury. Foot Ankle 1992;13:413–422
39.Major NM, Helms CA, Fritz RC, Speer KP. The MR imaging appearance of longitudinal split tears of the peroneus brevis tendon. Foot Ankle Int 2000;21:514–519
40.Rosenberg ZS, Beltran J, Cheung YY, Colon E, Herraiz F. MR features of longitudinal tears of the peroneus brevis tendon. AJR Am J Roentgenol 1997;168:141–147
41.Schweitzer ME, Eid ME, Deely D, Wapner K, Hecht P. Using MR imaging to di erentiate peroneal splits from other peroneal disorders. AJR Am J Roentgenol 1997;168:129–133
42.Cheung YY, Rosenberg ZS, Ramsinghani R, Beltran J, Jahss MH. Peroneus quartus muscle: MR imaging features. Radiology 1997;202:745–750
43.Sobel M, Pavlov H, Geppert MJ, Thompson FM, DiCarlo EF, Davis WH. Painful os peroneum syndrome: a spectrum of conditions responsible for plantar lateral foot pain. Foot Ankle Int 1994;15:112–124
44.Mengiardi B, Pfirrmann CWA, Vienne P, et al. Anterior tibial tendon abnormalities: MR imaging findings. Radiology 2005;235:977–984
45.Sammarco GJ, Cooper PS. Flexor hallucis longus tendon injury in dancers and nondancers. Foot Ankle Int 1998;19:356–362
46.Rubin DA, Tishko NW, Britton CA, Conti SF, Towers JD. Anterolateral soft-tissue impingement in the ankle: diagnosis using MR imaging. AJR Am J Roentgenol 1997;169:829–835
47.Adelaar RS, Madrian JR. Avascular necrosis of the talus. Orthop Clin North Am 2004;35:383–395
48.Brody AS, Strong M, Babikian G, Sweet DE, Seidel FG, Kuhn JP. John Ca ey Award paper. Avascular necrosis: early MR imaging and histologic findings in a canine model. AJR Am J Roentgenol 1991;157:341–345
49.Schweitzer ME, Morrison WB. MR imaging of the diabetic foot. Radiol Clin North Am 2004;42:61–71
50.Ledermann HP, Morrison WB, Schweitzer ME. MR image analysis of pedal osteomyelitis: distribution, patterns of spread, and frequency of associated ulceration and septic arthritis. Radiology 2002;223:747–755
51.Fabrin J, Larsen K, Holstein PE. Long-term follow-up in diabetic Charcot feet with spontaneous onset. Diabetes Care 2000;23:796–800
52.Klenerman L. The Charcot joint in diabetes. Diabet Med 1996;13(suppl 1):S52–S54
53.Woertler K. Soft tissue masses in the foot and ankle: characteristics on MR Imaging. Semin Musculoskelet Radiol 2005;9:227–242
54.Recht MP, Donley BG. Magnetic resonance imaging of the foot and ankle. J Am Acad Orthop Surg 2001;9:187–199

9 The Foot and Ankle 225
55.Morton TG. The Classic. A peculiar and painful a ection of the fourth metatarso-phalangeal articulation. Clin Orthop Relat Res 1979;142: 4–9
56.Levitsky KA, Alman BA, Jevsevar DS, Morehead J. Digital nerves of the foot: anatomic variations and implications regarding the pathogenesis of interdigital neuroma. Foot Ankle 1993;14:208–214
57.Kay D, Bennett GL. Morton’s neuroma. Foot Ankle Clin 2003;8: 49–59
58.Zanetti M, Weishaupt D. MR imaging of the forefoot: Morton neuroma and di erential diagnoses. Semin Musculoskelet Radiol 2005;9:175–186
59.Bergin D, Morrison WB. Postoperative imaging of the ankle and foot. Radiol Clin North Am 2006;44:391–406
60.Platt MA. Tendon repair and healing. Clin Podiatr Med Surg 2005;22:553–560
61.Reinig JW, Dorwart RH, Roden WC. MR imaging of a ruptured Achilles tendon. J Comput Assist Tomogr 1985;9:1131–1134
62.Alparslan L, Chiodo CP. Lateral ankle instability: MR imaging of associated injuries and surgical treatment procedures. Semin Musculoskelet Radiol 2008;12:346–358
63.Chien AJ, Jacobson JA, Jamadar DA, Brigido MK, Femino JE, Hayes CW. Imaging appearances of lateral ankle ligament reconstruction. Radiographics 2004;24:999–1008
64.Woel er KE, Figura MA, Sandberg NS, Snyder NS. Five-year followup results of instep plantar fasciotomy for chronic heel pain. J Foot Ankle Surg 2000;39:218–223

IV Spine
10 The Cervical Spine
Lukas P. Zebala, Jacob M. Buchowski, Aditya R. Daftary, Joseph R. O’Brien, John A. Carrino, and A. Jay Khanna
■ Specialized Pulse Sequences and
Protocols
Although imaging protocols of the cervical spine for specific indications can vary among institutions, standard MRI of the cervical spine for degenerative pathologies usually includes the following pulse sequences:
•Sagittal T1-weighted SE
•Sagittal T2-weighted FSE
•Axial gradient-echo
•Axial T2-weighted FSE
A detailed discussion of all the imaging sequences used in the cervical spine is beyond the scope of this chapter; however, salient features of commonly used sequences are discussed below.
T1-weighted images are useful in identifying fracture lines. Because they are sensitive to the presence of gadolinium contrast, they are also used for contrast-enhanced imaging, which is helpful in assessing neoplasms, infections, and the postoperative spine. Typically, fat-suppressed postgadolinium T1-weighted images are used to make lesions more conspicuous. T2-weighted images are sensitive to water (and thus edema) and are useful in identifying areas of potential pathology. However, care must be taken with regard to interpreting bone marrow edema because it may be seen with a variety of conditions, including infection, inflammation, trauma, and degeneration. Although edema may focus attention toward an abnormality, many of these conditions can coexist, so additional analysis is required before finalizing a conclusion. FSE is now routinely used to acquire T2-weighted images at speeds up to 64 times faster than conventional SE T2-weighted images. Sometimes the di erentiation of fat, water, and lesions can be di cult, especially on T2-weighted FSE images, and therefore fat suppression is used to make these areas more conspicuous. This sequence can be obtained by applying a fat-suppression pulse to produce fat-suppressed T2-weighted images or by obtaining a STIR sequence. Visualizing edema is helpful in identifying ligamentous injuries, and such visualization is best achieved with STIR or fat-suppressed T2-weighted images. T2-weighted images are also most sensitive for evaluating the cord parenchyma for lesions and edema, which are seen as abnormally bright signal, although the sagittal orientation
is subject to linear bright artifact within the cord (Gibbs phenomenon). For this reason, axial T2-weighted images serve as a useful tool for detecting cord abnormalities and confirming lesions suspected on sagittal T2-weighted images.
Gradient-echo images are very susceptible to magnetic artifacts; this important characteristic makes them useful for detecting small areas of hemorrhage, such as with cervical spine trauma and vascular malformations. However, these images can also overestimate the degree of canal and foraminal stenosis secondary to artifact from the adjacent bone. Because of the rapidity with which gradient-echo images are acquired, studies can be obtained with higher resolution than that required for other pulse sequences and even as a 3D volume set, which allows for isotropic voxels and reformations in multiple planes. This volume set can then allow one to characterize the cervical foramina in the appropriate oblique plane.
For evaluation of vascular structures in the neck, MR angiography can be obtained without contrast, using 2D or 3D time-of-flight or phase-contrast imaging. These sequences create contrast between flowing and stationary structures. Phase-contrast imaging may also provide flow-velocity information. As a result of the technique, time-of-flight imaging shows fat or subacute thrombus as bright signal and may be useful in detecting small, subtle thrombi. The 3D techniques require more time and are slightly less sensitive to slow flow states. Gadolinium-enhanced MR angiography may also be obtained and is extremely accurate.
■ Traumatic Conditions
Although the cervical spine is injured in only 2% to 3% of blunt trauma accidents,1 the potential for instability and critical neurologic injury makes prompt identification and management of cervical spine injuries important. Patients with suspected cervical spine injury should be evaluated initially with conventional radiographs (AP, lateral, and open-mouth odontoid views). CT imaging o ers greater osseous detail than does conventional radiography and may reveal fractures or details that are not detected with radiography. CT is especially helpful in assessing fractures of the occipital condyles and cervicothoracic junction, where osseous overlap on conventional radiographs makes fracture detection dif-
229
