
Книги по МРТ КТ на английском языке / MRI for Orthopaedic Surgeons Khanna ed 2010
.pdf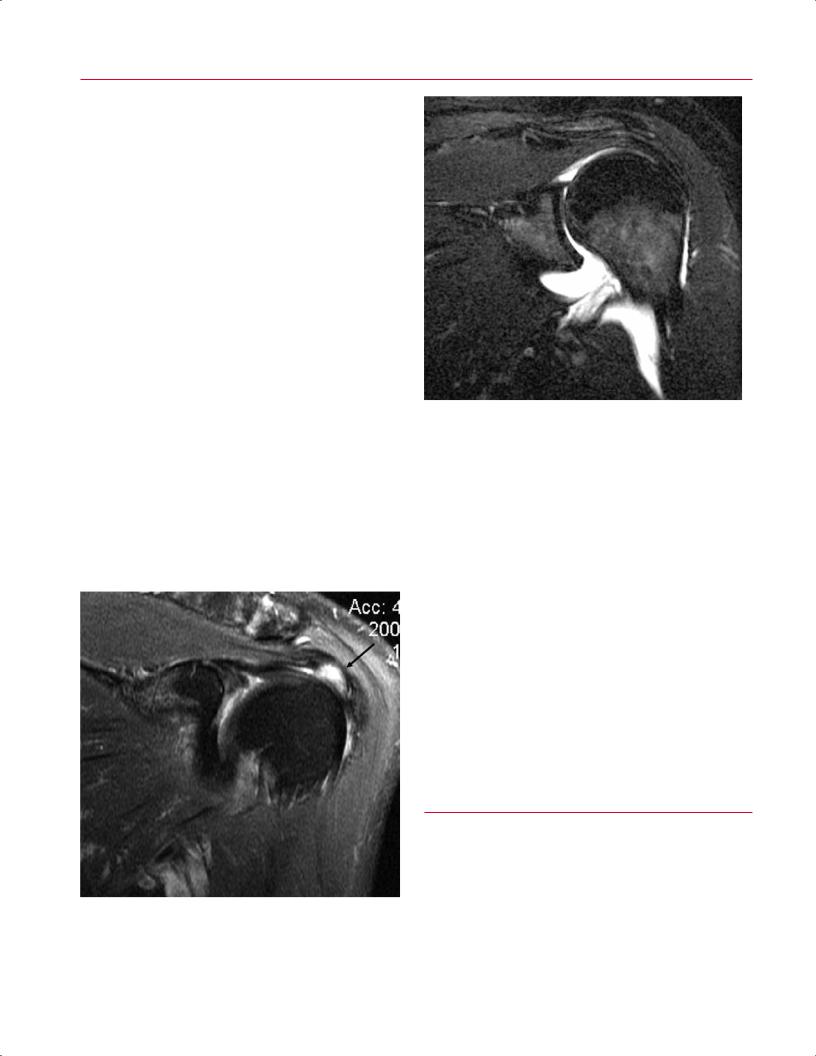
90 I Initial Concepts
A 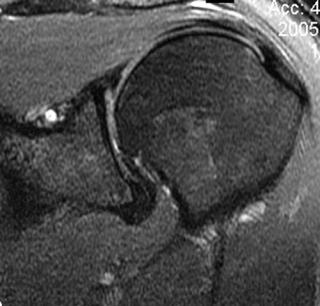 B
B
Fig. 3.17 Coronal oblique STIR images show minimal, if any, fluid within the left shoulder joint of a patient with no pathology (A) and a pathologically increased amount of joint fluid in the left shoulder joint of a patient with a HAGHL lesion (B).
the clinician identify a more specific diagnosis. As discussed above and in region-specific chapters, fat-suppressed T2weighted images can be used to evaluate for nondisplaced fractures and to determine the approximate age or chronicity of fractures, including vertebral compression fractures.
Postgadolinium T1-Weighted Images
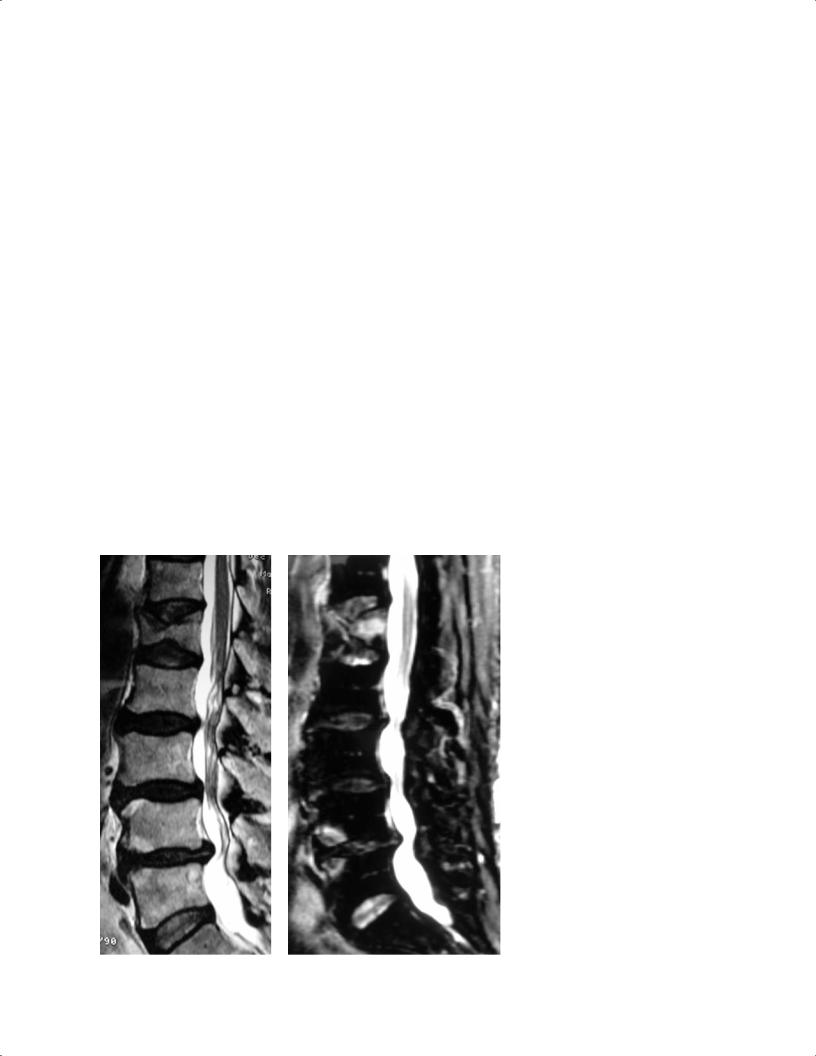
Postgadolinium T1-weighted images are often acquired to evaluate for the presence or absence of infection and tumor and to assess the postoperative joint or spine. For example, in the spine, postgadolinium T1-weighted images can help di erentiate recurrent disc herniation from epidural fibrosis and scar. The recommended method for evaluating these images is to place the postgadolinium T1-weighted images side by side with the pregadolinium T1-weighted images. The region of interest is then compared in the same planes and on matching images. Higher signal intensity in the region or structure of interest on the postgadolinium T1-weighted images is termed postgadolinium or contrast enhancement. An evaluation can then be made with regard to the degree and pattern of enhancement. For example, peripheral rim enhancement with a central region of nonenhancement in a relatively well-circumscribed lesion is considered, in the appropriate clinical setting, to be a finding suggestive of an abscess (Fig. 3.21).
■Step 5: Correlation of Imaging Findings with Patient History and Examination Findings to Determine the Most Likely Diagnosis
Fig. 3.18 A coronal oblique T2-weighted image of the left shoulder shows increased signal within the supraspinatus tendon (arrow), compatible with a high-grade partial-thickness tear.
Clinicians and radiologists have distinct advantages and disadvantages in terms of evaluating an MRI study. The radiologist has the advantage of often being trained with a process
3 A Systematic Approach to the Review of Musculoskeletal MRI Studies |
91 |
A 
 B
B
Fig. 3.19 Sagittal T1-weighted (A) and T2-weighted (B) images show a lesion at the T12 level with high signal intensity on both images and with the typical striations compatible with a vertebral body
hemangioma. An incidentally noted vertebral compression fracture is seen at the L1 level.
|
Fig. 3.20 Vertebral compression fracture. |
|
(A) A sagittal T2-weighted image of the lum- |
|
bar spine showing an L1 vertebral body com- |
|
pression fracture of an indeterminate age, |
|
given that edema is not definitely seen. (B) A |
|
sagittal STIR image of the same patient shows |
|
edema within the L1 vertebral body, which is |
|
compatible with an acute or subacute verte- |
A, B |
bral compression fracture. |
92 I Initial Concepts
A 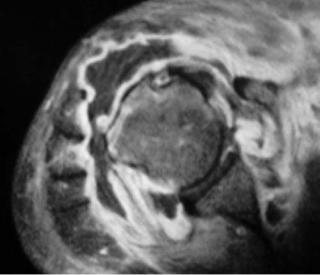 B
B
Fig. 3.21 Pregadolinium (A) and postgadolinium (B) T1-weighted images of the right shoulder showing a fluid collection around the glenohumeral joint with peripheral rim enhancement on the postga-
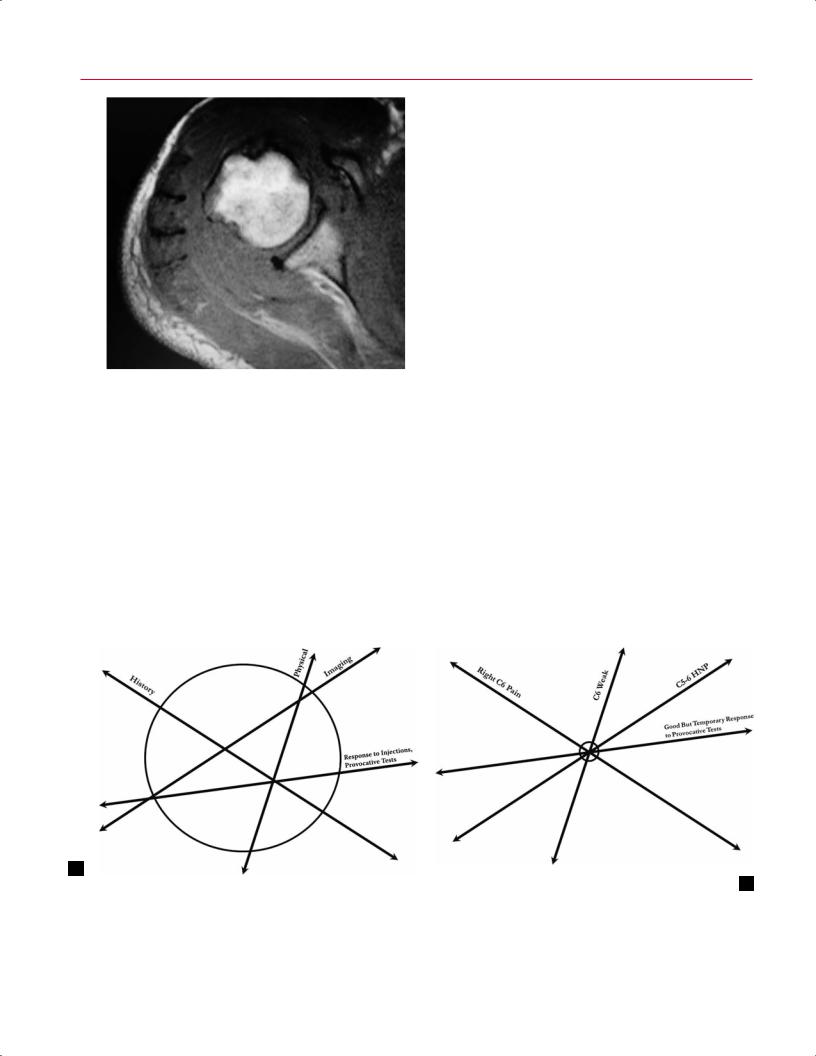
similar to the one described above and often has, and takes, the time to evaluate the images in a systematic fashion. However, the clinician has the advantage of knowing the patient’s history and physical examination findings, laboratory results, and other parameters. It is essential that clinicians use this advantage to help maximize the accuracy and reliability of their MRI interpretations. An accurate diagnosis, or di erential diagnosis, occurs at the “intersection” of a patient’s history, physical examination results, radiographic findings, and laboratory study results (Fig. 3.22). With an
dolinium image (B) in a patient with infectious symptoms and findings. The imaging characteristics are compatible with an abscess and associated septic joint.
understanding of the clinical scenario, clinicians can arrive at an accurate diagnosis, especially when they are armed with the appropriate techniques for evaluating the MRI studies. One way to leverage the advantages of both clinicians and radiologists is to use a collaborative team approach to the evaluation of patients with complex pathology.
For example, if a patient presents with knee pain after trauma and is point-tender at the proximal anterior tibia and if the MR image shows an area of increased T2-weighted signal within the tibial plateau, the diagnosis of a bone bruise
A
Fig. 3.22 The concept of intersecting lines for diagnosis and surgical decision-making. (A) In a patient for whom the history, physical examination, imaging findings, and response to provocative tests do not “intersect” within a small circle, it is di cult to identify a diag-
B
nosis or to narrow a di erential diagnosis. (B) Conversely, for a patient with a smaller region of intersection, such as one with a right C6 radiculopathy, one may expect to see a C5-C6 disc protrusion on MRI.

3 A Systematic Approach to the Review of Musculoskeletal MRI Studies |
93 |
or a nondisplaced tibial plateau fracture can be suggested. However, if a patient with the same imaging findings presents with no history of trauma, is elderly, has a history of insidious onset of knee pain (particularly at night), and has a history of a primary malignancy, another diagnosis (e.g., metastatic disease) might be higher on the di erential diagnosis. To determine the correct diagnosis, the clinician would likely obtain a CT scan to evaluate further the osseous anatomy in both patients. The second patient might also benefit from a primary malignancy survey and a three-phase bone scan.
In summary, the above-described five-step technique will help guide the clinician in systematically evaluating MRI studies of various regions of the musculoskeletal system. This
author strongly believes that such a systematic technique should be used for the evaluation of all MRI studies and that the tendency to become less meticulous and systematic over time should be avoided. One additional concept taught to the residents in the author’s institution is always to attempt to read the MRI study using the above-described technique and then to evaluate the “o cial” radiologist’s reading to determine the degree of correlation between the two readings. Occasionally, findings are noted by the clinicians that were not reported by the radiologist, and vice versa. Over time, this method of checking one’s own evaluation against that of another trained specialist will serve as method of quality control and assurance and will likely result in a continuously improving ability to evaluate MRI studies accurately.
Reference
1. Groopman J. How Doctors Think. Boston: Houghton Mi in; 2007.

II Upper Extremity
4 The Shoulder
Adam J. Farber, A. Jay Khanna, Laura M. Fayad, Timothy S. Johnson, and Edward G. McFarland
■Specialized Pulse Sequences and Imaging Protocols
MRI of the shoulder has improved with the development of high-field systems and enhanced surface coil technology.1 The patient is imaged in the supine position and the arm is held at the side, rather than across the chest, to minimize transmission of respiratory motion to the shoulder. To optimally visualize the supraspinatus tendon and its insertion and to prevent confusing overlap with the infraspinatus tendon on coronal oblique images, the arm is placed in slight external rotation. Axial, coronal oblique, and sagittal oblique images are obtained routinely.
Most centers use a standard screening examination, consisting of an array of specified imaging planes and pulse sequences.1 In addition to standard intermediate-weighted (proton-density) images, fat-suppressed proton-density, fatsuppressed T2-weighted, and STIR sequences are sensitive to the presence of fluid. The latter sequences allow the detection of soft-tissue pathology by accentuating the increased signal of edema relative to the surrounding structures. In some centers, non–fat-suppressed T2-weighted imaging is preferred for the evaluation of the rotator cu tendons because it aids in the distinction of tendinosis and partial tears. In general, these sequences are acquired with an FSE technique that produces the desired contrast in a fraction of the time needed for conventional SE sequences. In addition, gradient-echo sequences may be used to evaluate the articular cartilage (see Chapter 14) and to delineate the presence of intraarticular bodies or accentuate calcification seen with calcium hydroxyapatite deposition. However, gradient-echo sequences should be avoided after shoulder surgery (especially in the presence of metal hardware) because of the increased artifact inherent to the gradient-echo technique (see Chapter 1).
MR arthrography can be performed via direct or indirect methods. Direct MR arthrography is performed by injecting approximately 10 to 15 mL of diluted gadolinium contrast agent into the glenohumeral joint from an anterior or posterior approach and acquiring fat-suppressed T1-weighted and T2-weighted images. Indirect MR arthrography is performed by injecting gadolinium intravenously and imaging the joint after contrast has been taken up by the synovium and then di used into the joint. Direct MR arthrography of
the shoulder has been shown to improve visualization of the labrum, the articular cartilage, and the rotator cu tendons. Indirect MR arthrography has limited use for evaluation of the labrum, but it aids in the detection of rotator cu pathology and in the assessment of arthritis, neoplasm, and infection. However, with the advent of high-field, high-reso- lution imaging and novel noncontrast MR techniques, direct and indirect MR arthrography techniques may be rendered obsolete in the future.2
■ Traumatic Conditions
Traumatic conditions a ecting the shoulder that are commonly evaluated by MRI include the following:
•Glenohumeral instability
•Labral pathology
•Occult fractures
•Rotator cu tears
Many rotator cu tears occur in the setting of long-standing tendinosis (see Degenerative Conditions, below).
Glenohumeral Instability
Because of the shoulder’s extensive range of motion, it is the most commonly dislocated joint in the body.3,4 Instability encompasses a spectrum of disorders of varying direction, degree, and etiology. Shoulder instability is classified based on the direction of dislocation (i.e., anterior [most common], posterior, or multidirectional) and by degree (dislocation, subluxation, and microinstability), force (traumatic versus atraumatic), and patient contribution (voluntary versus involuntary). Instability episodes range from subluxation to complete dislocation and are associated with a spectrum of injury to the shoulder stabilizers.
Patients with recurrent anterior shoulder instability typically have a history of a traumatic (direct or indirect) anterior shoulder dislocation, report recurrent episodes of subluxation or dislocation, and describe symptoms such as pain or apprehension during arm abduction and external rotation. Patients with recurrent posterior instability pose more complex diagnostic challenges and can present
97
98 |
II Upper Extremity |
|
|
|
• An abnormally small or absent anterior labrum, or |
|
|
• A displaced anterior glenoid labrum with the presence |
|
|
of fluid signal intensity between the anterior rim of |
|
|
the osseous glenoid and the displaced labrum. |
|
|
In addition, a low signal intensity fracture line surrounded |
|
|
by edema (intermediate T1-weighted signal intensity and |
|
|
high T2-weighted signal intensity) is seen in the presence of |
|
|
a fracture.8 These findings are best appreciated on the axial |
|
|
images (Figs. 4.1 and 4.2). As with most traumatic condi- |
|
|
tions, the pattern of MRI signal intensity often can be used |
|
|
to estimate the approximate age of a given injury. High signal |
|
|
intensity on T2-weighted or fat-suppressed T2-weighted im- |
|
|
ages (along with low signal intensity on T1-weighted images) |
|
|
suggests the presence of an acute, or at least subacute, injury |
|
|
because it indicates the presence of edema at the site of in- |
|
|
jury. Conversely, the absence of increased signal intensity on |
|
|
T2-weighted or fat-suppressed T2-weighted images suggests |
|
|
the presence of a chronic injury with no substantial edema |
|
|
present. A finding known as the double axillary pouch sign |
|
|
is assessed with coronal oblique images and is very specific |
|
Fig. 4.1 An axial fat-suppressed proton-density image of the left |
for anterior labral tears.9 |
|
A lesion known as the anterior labroligamentous perios- |
|
|
shoulder showing an osseous Bankart lesion (white arrow) and a Hill- |
|
|
Sachs lesion (black arrow). |
teal sleeve avulsion injury is a variation of the Bankart le- |
|
with traumatic posterior instability or with atraumatic sub- |
sion; unlike a Bankart lesion, the anterior labroligamentous |
|
periosteal sleeve avulsion lesion has an intact anterior scap- |
|
|
luxations not associated with trauma. Trauma, direct or in- |
ular periosteum, allowing the labroligamentous structures |
|
direct, also may be the mechanism of injury of a posterior |
to displace medially and to rotate inferiorly on the scapular |
|
shoulder instability or dislocation. Seizures and electrocu- |
neck.10 This lesion is visualized on axial MR images as medial |
|
tion are common causes of posterior shoulder dislocation. |
|
|
Although conventional radiographs often are su cient |
|
|
for diagnosing shoulder dislocation, MRI is valuable in eval- |
|
|
uating patients with presumed instability but no history of |
|
|
a dislocation, or to evaluate the status of the rotator cu in |
|
|
patients preoperatively. |
|
|
The MRI findings of anterior instability vary depending |
|
|
on the degree of instability and the chronicity of instability. |
|
|
The most common pathologies associated with traumatic |
|
|
anterior shoulder instability are detachment of the ante- |
|
|
rior-inferior labrum (known as a Perthes-Bankart lesion) |
|
|
and tears of the anterior capsule.5 The Bankart lesion (Figs. |
|
|
4.1 and 4.2) represents an avulsion of the anterior-inferior |
|
|
glenoid labrum from the glenoid rim (soft-tissue Bankart |
|
|
lesion). When this lesion is associated with an intact an- |
|
|
terior scapular periosteum, it is called an anterior labrum |
|
|
periosteal sleeve avulsion lesion. There may be an associated |
|
|
fracture of the anterior inferior glenoid rim (osseous Bankart |
|
|
lesion)6 or a contusion of the posterior aspect of the humeral |
|
|
head (Hill-Sachs lesion).6 |
|
|
The MRI appearance of a Bankart lesion includes the |
|
|
following7: |
|
|
• A linear high signal intensity coursing through the |
|
|
normally homogeneously low signal intensity labral |
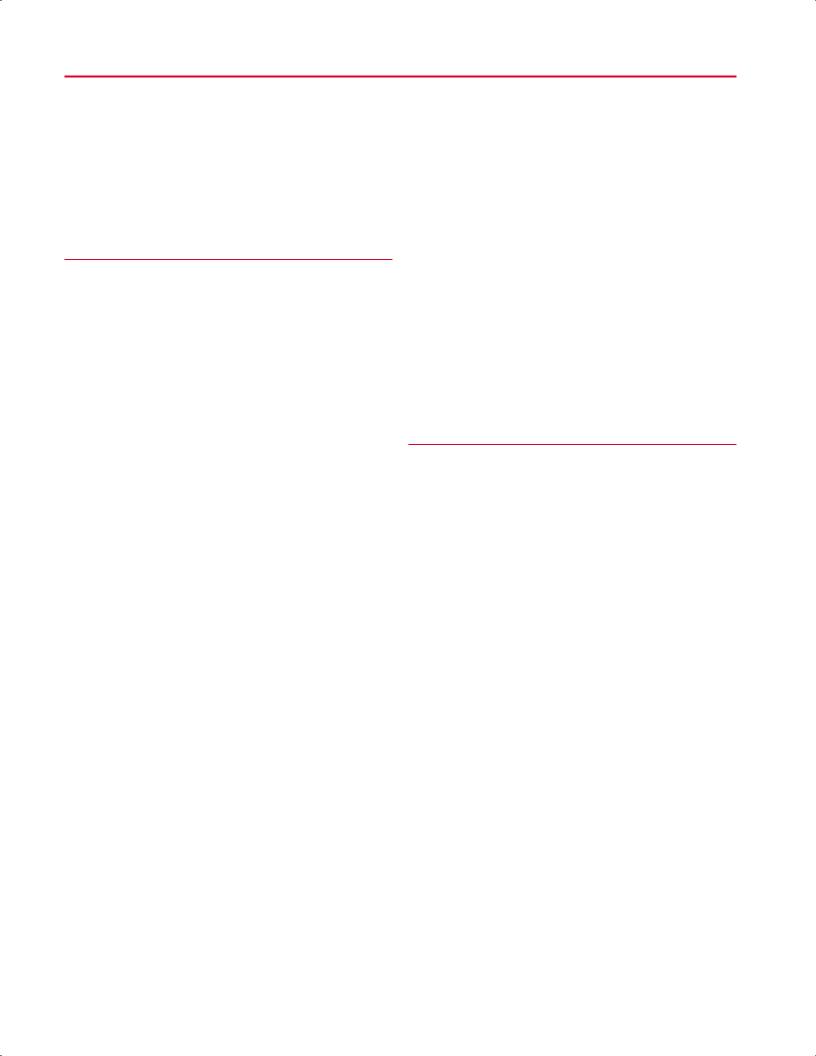
Fig. 4.2 An axial fat-suppressed proton-density image of the right |
|
substance, |
shoulder showing the labral tear of a Bankart lesion (arrow). |
4 The Shoulder 99
Fig. 4.3 An axial fat-suppressed T2-weighted image of an anterior labroligamentous periosteal sleeve avulsion lesion in the right shoulder showing the medially displaced anterior labrum (arrow).
displacement and inferior rotation of a torn anterior labrum (Fig. 4.3).10
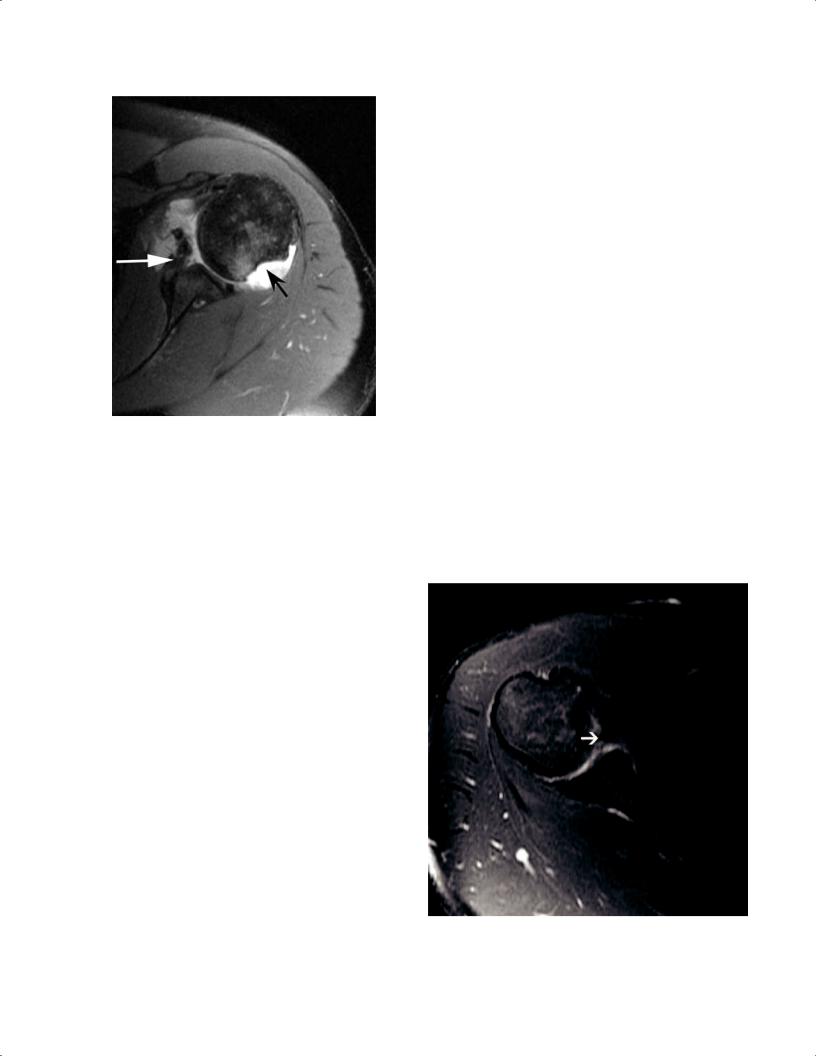
Anterior shoulder dislocations may also produce a posterolateral impression fracture in the humeral head, known as a Hill-Sachs lesion.11 This lesion is seen on MRI as a flattening or concavity of the posterolateral humeral head detected on the two most superior axial images through the level of the humeral head; on those superior images, the humeral head is normally round above the bicipital groove and tuberosities (Fig. 4.4).12,13
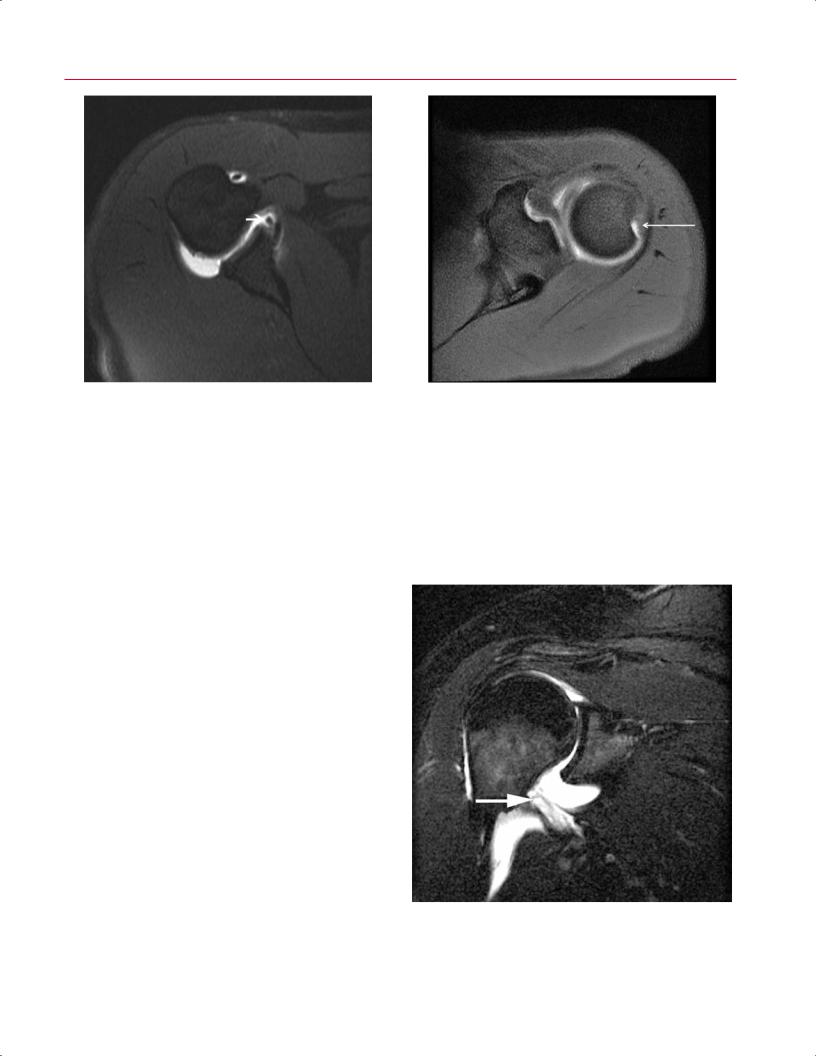
Finally, an anterior shoulder dislocation may tear the IGHL without injuring the anterior labrum. This injury, known as a HAGHL, is defined as an avulsion of the IGHL from the anatomic neck of the humerus.14,15 On MRI, a HAGHL shows morphologic disruption of the normally low signal intensity IGHL on axial images.14 In addition, fluid signal intensity often is seen within the soft tissues anterior and inferior to the shoulder joint, which likely represents edema, hematoma, or extravasated joint fluid (Fig. 4.5).14 The HAGHL is frequently associated with tears of the subscapularis tendon.14
Posterior instability of the shoulder is much less common than anterior instability. MRI findings of posterior instability are analogous to the findings seen with anterior instability, but the word reverse is used to describe lesions that convey a posterior direction to the instability. Therefore, in a patient who has sustained posterior shoulder instability in which the humeral head has subluxated or dislocated posterior to the glenoid, a reverse Bankart lesion represents an avulsion of the posterior-inferior capsulolabral structures from the glenoid rim (Fig. 4.6); similarly, a reverse Hill-Sachs lesion represents edema or an impaction fracture of the anterome-
Fig. 4.4 An axial fat-suppressed T1-weighted image showing a HillSachs impression fracture (arrow) on the posterolateral aspect of the humeral head in a left shoulder.
dial humeral head16 (Fig. 4.7). In addition to these findings, MRI typically reveals posterior capsular disruption, which is evident as a disruption or marked irregularity of the normally low signal intensity line representing the posterior capsule.16
Fig. 4.5 A coronal fat-suppressed T2-weighted image of a HAGHL lesion in the right shoulder showing fluid signal passage through the anterior band of the IGHL (arrow).
