
- •Vascular Surgery
- •SECTION AND BOARD OF VASCULAR SURGERY
- •Foreword to the First Edition
- •Preface to the First Edition
- •Preface to the Second Edition
- •Preface to the Third Edition
- •Contents
- •Contributors
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •1.1 Commentary
- •1.2 Beta-Adrenergic Antagonists
- •1.3 3-Hydroxy-3-Methylglutaryl Coenzyme A Reductase Inhibitors (Statins)
- •1.4 Percutaneous Revascularization
- •1.5 Coronary Artery Bypass Grafting
- •References
- •2: Abdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •2.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •Question 13
- •Question 14
- •3.1 Commentary
- •3.2 Case Analysis Quiz
- •References
- •4: Ruptured Abdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •4.1 Commentary
- •References
- •5: Thoracoabdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •5.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •Question 13
- •6.1 Commentary
- •References
- •7: Aortic Dissection
- •7.1 Dissection: Stanford A
- •Question 1
- •Question 2
- •Question 3
- •7.2 Dissection: Stanford B
- •Question 4
- •Question 5
- •7.3 Commentary
- •References
- •8: Popliteal Artery Aneurysms
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •8.1 Popliteal Artery Aneurysm
- •References
- •9: Renal Artery Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •9.1 Commentary
- •References
- •10: Anastomotic Aneurysms
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •10.1 Commentary
- •10.2 Indications for Intervention
- •10.3 Treatment for Anastomotic Aneurysms
- •10.4 Infection in Anastomotic Aneurysms
- •10.5 Outcome
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •11.1 Commentary
- •References
- •12: Acute Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •12.1 Commentary
- •References
- •13: Arterial Embolism
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •13.1 Commentary
- •References
- •14: Blast Injury to the Lower Limb
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •14.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •15.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Smoking
- •Antiplatelet Agents
- •Blood Pressure (BP)
- •Glucose Status
- •Lipids
- •Emerging Risk Factors
- •Question 4
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •17.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •18.1 Commentary
- •18.2 Clinical Assessment
- •18.3 Imaging Techniques
- •18.4 Revascularization Options
- •18.5 Aortobifemoral Bypass
- •18.6 Iliac Angioplasty and Stenting
- •18.7 Iliac Stenting Combined with Profunda Femoris Artery Revascularization
- •18.8 Rationale for Angioplasty of “Donor” Iliac Artery Prior to Femorofemoral Crossover Bypass
- •18.10 Supervision and Follow-up of the Patient
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •19.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •20.1 Commentary
- •References
- •21: Bypass to the Popliteal Artery
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •21.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •22.1 Commentary
- •References
- •23: Popliteal Artery Entrapment
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •23.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •24.1 Commentary
- •References
- •25: The Obturator Foramen Bypass
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •25.1 Commentary
- •25.2 Preoperative Measures
- •25.3 The Concept of the Obturator Foramen Bypass
- •25.4 Obturator Foramen Bypass Technique
- •References
- •26: Diabetic Foot
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •26.1 Commentary
- •References
- •27: Chronic Visceral Ischemia
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •27.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •28.1 Commentary
- •References
- •29: Renovascular Hypertension
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •29.1 Commentary
- •29.4 Intra-arterial Angiography
- •29.5 Duplex Ultrasonography (DU)
- •29.6 Treatment
- •29.6.1 Medical Treatment
- •29.6.2 Revascularization
- •29.7 Prognosis
- •References
- •30: Midaortic Syndrome
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •30.1 Commentary
- •References
- •31: Management of Portal Hypertension
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •31.1 Commentary
- •31.2 General Considerations
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •32.1 Commentary
- •References
- •33: The Carotid Body Tumor
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •33.1 Commentary
- •33.2 Clinical Presentation
- •33.3 Treatment
- •33.4 Summary
- •References
- •Question 1
- •Question 2
- •Question 3
- •34.1 Commentary
- •34.2 Vertebrobasilar Ischemia: Low-Flow Mechanism
- •Question 1
- •Question 2
- •34.3 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •35.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •36.1 Commentary
- •References
- •37: Acute Axillary/Subclavian Vein Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •37.1 Commentary
- •References
- •38: Raynaud’s Phenomenon
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •38.1 Commentary
- •References
- •39: Aortofemoral Graft Infection
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •39.1 Commentary
- •References
- •40: Aortoenteric Fistulas
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •40.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •41.1 Commentary
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Questions 7 and 8
- •Question 9
- •Question 10
- •Comment
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •42.1 Commentary
- •References
- •43: Amputations in an Ischemic Limb
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •43.1 Commentary
- •References
- •44: Congenital Vascular Malformation
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •44.1 Clinical Evaluation
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •44.2 Commentary
- •References
- •45: Klippel-Trenaunay Syndrome
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •45.1 Commentary
- •Clinical Presentation
- •Evaluation
- •Treatment
- •References
- •46: Deep Venous Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •46.1 Commentary
- •References
- •47: Endoluminal Ablation of Varicose Veins
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •47.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •48.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •50.1 Commentary
- •References
- •51: Iliofemoral Venous Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •50.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •52.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •53.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •54.1 Commentary
- •References
- •Index

20 Endovascular Management of Non-Healing Leg Ulceration |
217 |
|
|
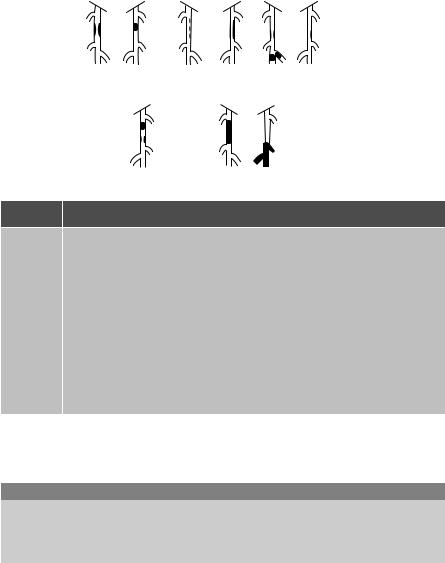
Fig. 20.2 Distal popliteal and proximal tibial anatomy
Question 3
The TASC (Trans-Atlantic Societal Classification) category of the superficial femoral artery segment is best identified as:
A.TASC A
B.TASC B
C.TASC C
D.TASC D
E.TASC E
Question 4
The best treatment option for this patient is:
A.Medical management with Cilostazol, Clopidigrel, and referral to a wound care center.
B.Percutaneous revascularization of the femoral artery lesions, with distal synthetic popliteal to anterior tibial bypass at the ankle.

218 |
J. Starr and P. Vaccaro |
|
|
Fig. 20.3 Distal anterior tibial stenoses
C. Percutaneous revascularization of the femoral and anterior tibial arteries. D. Right femoral to anterior tibial composite bypass graft.
Discussion with the patient occurred pre-procedurally in the office setting. She was offered concomitant intervention if deemed appropriate at the time and informed consent was obtained. The patient was given appropriate sedation and anticoagulated with heparin. The diagnostic 5Fr sheath was exchanged for a 6Fr RDC angled guiding sheath. Cannulation of the contralateral common iliac was performed with the aid of a SOS catheter and 0.035 stiff hydrophilic guidewire under constant fluoroscopic guidance. The sheath was advanced to therightexternaliliacartery.Roadmaptechniquesandsmallamountsofcontrastwereused tocrosstheSFAlesions.Anangled,hydrophiliccoated5Frcatheterwasemployedtoassist in crossing the stenoses. The tip of the guidewire was placed in the distal popliteal artery. A 5 mm x 4 cm cryoplasty balloon was inflated at each diseased area with an adequate angiographic appearance and no evidence of dissection or other complication (Fig. 20.4).
Next, the 0.035 guidewire was exchanged for a 0.014 exchange length guidewire and the lesionsintheanteriortibialarterywerecrossed.Thestenosesweretreatedwitha2.5mm × 5cm balloon with good results and no complications (Fig. 20.5). The sheath was partially withdrawn and the left femoral artery was imaged. The access site was felt to be adequate for an arterial closure device which was placed without complication. The heparin was not reversed.
Following treatment, her post procedure anterior tibial ankle waveform was multiphasic. Her ulcer improved with a reduction in diameter, however the first metatarsal head was exposed. The patient underwent right first toe transmetatarsal amputation 2 weeks later

20 Endovascular Management of Non-Healing Leg Ulceration |
219 |
|
|
Fig. 20.4 Result after SFA cryoplasty with improvement in all three stenoses
which healed nicely. Six months later, routine lower extremity arterial non-invasive testing showed a flat right ankle PVR. The patient denied new ulceration or rest pain.
Question 5
The patient should be offered:
A.Repeat angiogram and intervention if anatomically appropriate.
B.Operative revascularization.
C.Medical management with warfarin therapy and risk factor modification.
D.Risk factor modification and protective orthotics.
20.1 Commentary
Critical limb ischemia may include ischemic rest pain, non-healing ulcers, or gangrene, all of which may lead to limb loss if left untreated, and at the very least cause significant lifestyle changes. Initial evaluation should include lower extremity arterial dopplers with

220 |
J. Starr and P. Vaccaro |
|
|
Fig. 20.5 Results after PTA of distal anterior tibial artery
waveforms which serve to give an idea of disease distribution and severity. Testing is noninvasive, inexpensive, and widely available. Non-invasive vascular testing, especially duplex imaging, may help to rule out more proximal occlusive disease, and allow less contrast to be used during angiography and interventional procedures.1 Adding arterial duplex imaging may also help plan an interventional procedure by identifying target lesions. Additionally, a baseline ankle-brachial index (ABI) or waveform may be utilized to assess the adequacy of an intervention and is one means of following a patient’s vascular status over time, especially if there is a worsening in the clinical situation. [Q1: B]
Although magnetic resonance (MR) angiography may help delineate extent and location of disease, a pre-planned intervention obviously cannot be performed simultaneously. There are additional risks to patients with chronic kidney disease, related to Gadolinium administration. The most severe involves nephrogenic systemic fibrosis which is characterized by thickening and tightening of the skin and subcutaneous tissues and can involve theskeletalmuscle,lung,liver,testes,ormyocardium.Theoutcomecanbefatal.2 Adequate
20 Endovascular Management of Non-Healing Leg Ulceration |
221 |
|
|
MR vascular imaging equipment and software are not uniform, nor widely available. Interpretation, especially with total occlusions, may be subjective as well. Advantages may include the avoidance of an iodinated contrast study if an intervention is not feasible or indicated. Exposure to a radiation source is also avoided. The local complications of a percutaneous procedure, including pseudoaneurysm formation, hematoma, arterial occlusion, and bleeding, are averted.
Computed tomographic angiography (CTA) is sometimes used as a minimally invasive diagnostic tool for the evaluation of vascular disease. Drawbacks include the inability to perform a concomitant intervention, as with MRA, the need for iodinated contrast with the known inherent risks, and the use of radiation. CTA has the additional disadvantage of difficulty imaging accurately in the presence of heavily calcified lesions.3
ABI’s have also been suggested for patients free from clinical signs and symptoms of vascular disease with other risk factors. They have been shown to correlate with long term survival. An ABI of < 0.9 has been shown to have double the 10 year overall mortality, cardiovascular mortality, and major coronary event rate.4 Digital-brachial waveforms may be more reliable than ABI’s in patients with large vessel calcifications, such as is commonly found in diabetics.5 Digital vessels are often spared calcification and therefore are compressible and allow non-invasive pressure measurements. Direct popliteal pressures may help predict the healing potential in patients undergoing below the knee amputation.6 A pulsus tardus waveform indicates a more proximal obstruction and may arise due to a post-stenotic pressure drop or changes in post-stenotic vessel compliance. It is used most commonly for evaluation of renal artery stenosis.7 [Q2: A]
The initial TASC recommendations, originally published in 2000,8 were more recently revised in 2007 by representatives from 16 different societies and all concerned specialties.9 In both TASC publications, anatomic criteria are grouped into four classifications as an effort to give clinical management guidelines based on severity of disease. Since the 2000 inception, more evidence has emerged in support of endovascular therapies and this has beenincorporatedintothelatestrecommendations.Thelevelofavailableevidencereviewed (levelA,B,orC)wasalsoanalyzedbycontentexpertsandapplied.The2007femoralartery criteriaarelistedinFig.20.6.RecommendationsforinterventionaredescribedinTable20.1. There are separate categories for iliac artery atherosclerotic disease. No recommendations for tibial occlusive disease are currently available. This patient’s SFA lesions are best categorized as TASC class B and an endovascular approach is recommended as the first line of treatment. There is no TASC class E category in any anatomic distribution. [Q3: B]
This patient’scritical limb threateningischemiawarrants timely intervention inorder to prevent further tissue and potential limb loss. Restoration of direct flow to the area of ischemia is ideal and may provide better healing rates.10 She has limited autogenous vein available, with potentially short segments of great saphenous vein below the knee, small saphenous vein, and cephalic vein. Consideration should be given to obtaining non-inva- sive mapping of these venous segments. Distal tibial and pedal revascularization with prosthetic or composite grafts has poorer long term patency than autogenous bypasses, but there has been no direct comparison to endovascular intervention, solely for the infrapopliteal vascular bed. There is evidence that infrainguinal angioplasty may be a better first alternative for patients who are anatomically suitable and have a life expectancy less than 2 years, especially when autogenous vein is unavailable.11 There may be a high restenosis
222 |
J. Starr and P. Vaccaro |
|
|
Type A |
Type B |
Type C |
Type D |
Lesion type Description
ASingle stenosis ≤10 cm in length
Single occlusion £5 cm in length
BMultiple lesions (stenoses or occlusions), each ≤5 cm
Single stenosis or occlusion £15 cm not involving the infrageniculate popliteal artery
Single or multiple lesions in the absence of continous tibial vessels to improve inflow for a distal bypass
Heavily calcified occlusion £15 cm in length
Single popliteal stenosis
CMultiple stenoses or occlusions totaling >15 cm with or without heavy calcification
Recurrent stenoses or occlusions that need treatment after two endovascular interventions
DChronic total occlusions of CFA or SFA (>20 cm, involving the popliteal artery)
Chronic total occlusion of popliteal artery and proximal trifurcation vessels
Fig. 20.6 TASC II infrainguinal classification
Table 20.1 Preferred options for treating femoropopliteal lesions
Type of lesion |
Treatment recommendations |
TASC A |
Endovascular therapy is the treatment of choice |
TASC B |
Endovascular therapy is the preferred treatment |
TASC C |
Surgery is preferred for good risk patients |
TASC D |
Surgery is the treatment of choice |
rate,butthereisacceptablelimbsalvagerateinpatientswithlimbthreateningischemia.12,13 This patient has limited autogenous vein and an appropriate primary intervention is percutaneous revascularization. Options include balloon angioplasty, cryoplasty, stenting, and atherectomy, in addition to other techniques. [Q4: C]
Consensus does not exist regarding the type of endovascular management for atherosclerotic infrainguinal disease. Balloon angioplasty was the first modality introduced and is still advocated by some for short segment, uncomplicated lesions. Nitinol stenting has recently shown superiority over simple balloon angioplasty but debate continues.14 Covered stent
