
- •Vascular Surgery
- •SECTION AND BOARD OF VASCULAR SURGERY
- •Foreword to the First Edition
- •Preface to the First Edition
- •Preface to the Second Edition
- •Preface to the Third Edition
- •Contents
- •Contributors
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •1.1 Commentary
- •1.2 Beta-Adrenergic Antagonists
- •1.3 3-Hydroxy-3-Methylglutaryl Coenzyme A Reductase Inhibitors (Statins)
- •1.4 Percutaneous Revascularization
- •1.5 Coronary Artery Bypass Grafting
- •References
- •2: Abdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •2.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •Question 13
- •Question 14
- •3.1 Commentary
- •3.2 Case Analysis Quiz
- •References
- •4: Ruptured Abdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •4.1 Commentary
- •References
- •5: Thoracoabdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •5.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •Question 13
- •6.1 Commentary
- •References
- •7: Aortic Dissection
- •7.1 Dissection: Stanford A
- •Question 1
- •Question 2
- •Question 3
- •7.2 Dissection: Stanford B
- •Question 4
- •Question 5
- •7.3 Commentary
- •References
- •8: Popliteal Artery Aneurysms
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •8.1 Popliteal Artery Aneurysm
- •References
- •9: Renal Artery Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •9.1 Commentary
- •References
- •10: Anastomotic Aneurysms
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •10.1 Commentary
- •10.2 Indications for Intervention
- •10.3 Treatment for Anastomotic Aneurysms
- •10.4 Infection in Anastomotic Aneurysms
- •10.5 Outcome
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •11.1 Commentary
- •References
- •12: Acute Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •12.1 Commentary
- •References
- •13: Arterial Embolism
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •13.1 Commentary
- •References
- •14: Blast Injury to the Lower Limb
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •14.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •15.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Smoking
- •Antiplatelet Agents
- •Blood Pressure (BP)
- •Glucose Status
- •Lipids
- •Emerging Risk Factors
- •Question 4
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •17.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •18.1 Commentary
- •18.2 Clinical Assessment
- •18.3 Imaging Techniques
- •18.4 Revascularization Options
- •18.5 Aortobifemoral Bypass
- •18.6 Iliac Angioplasty and Stenting
- •18.7 Iliac Stenting Combined with Profunda Femoris Artery Revascularization
- •18.8 Rationale for Angioplasty of “Donor” Iliac Artery Prior to Femorofemoral Crossover Bypass
- •18.10 Supervision and Follow-up of the Patient
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •19.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •20.1 Commentary
- •References
- •21: Bypass to the Popliteal Artery
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •21.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •22.1 Commentary
- •References
- •23: Popliteal Artery Entrapment
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •23.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •24.1 Commentary
- •References
- •25: The Obturator Foramen Bypass
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •25.1 Commentary
- •25.2 Preoperative Measures
- •25.3 The Concept of the Obturator Foramen Bypass
- •25.4 Obturator Foramen Bypass Technique
- •References
- •26: Diabetic Foot
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •26.1 Commentary
- •References
- •27: Chronic Visceral Ischemia
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •27.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •28.1 Commentary
- •References
- •29: Renovascular Hypertension
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •29.1 Commentary
- •29.4 Intra-arterial Angiography
- •29.5 Duplex Ultrasonography (DU)
- •29.6 Treatment
- •29.6.1 Medical Treatment
- •29.6.2 Revascularization
- •29.7 Prognosis
- •References
- •30: Midaortic Syndrome
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •30.1 Commentary
- •References
- •31: Management of Portal Hypertension
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •31.1 Commentary
- •31.2 General Considerations
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •32.1 Commentary
- •References
- •33: The Carotid Body Tumor
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •33.1 Commentary
- •33.2 Clinical Presentation
- •33.3 Treatment
- •33.4 Summary
- •References
- •Question 1
- •Question 2
- •Question 3
- •34.1 Commentary
- •34.2 Vertebrobasilar Ischemia: Low-Flow Mechanism
- •Question 1
- •Question 2
- •34.3 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •35.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •36.1 Commentary
- •References
- •37: Acute Axillary/Subclavian Vein Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •37.1 Commentary
- •References
- •38: Raynaud’s Phenomenon
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •38.1 Commentary
- •References
- •39: Aortofemoral Graft Infection
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •39.1 Commentary
- •References
- •40: Aortoenteric Fistulas
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •40.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •41.1 Commentary
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Questions 7 and 8
- •Question 9
- •Question 10
- •Comment
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •42.1 Commentary
- •References
- •43: Amputations in an Ischemic Limb
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •43.1 Commentary
- •References
- •44: Congenital Vascular Malformation
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •44.1 Clinical Evaluation
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •44.2 Commentary
- •References
- •45: Klippel-Trenaunay Syndrome
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •45.1 Commentary
- •Clinical Presentation
- •Evaluation
- •Treatment
- •References
- •46: Deep Venous Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •46.1 Commentary
- •References
- •47: Endoluminal Ablation of Varicose Veins
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •47.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •48.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •50.1 Commentary
- •References
- •51: Iliofemoral Venous Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •50.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •52.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •53.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •54.1 Commentary
- •References
- •Index

12 Acute Thrombosis |
117 |
|
|
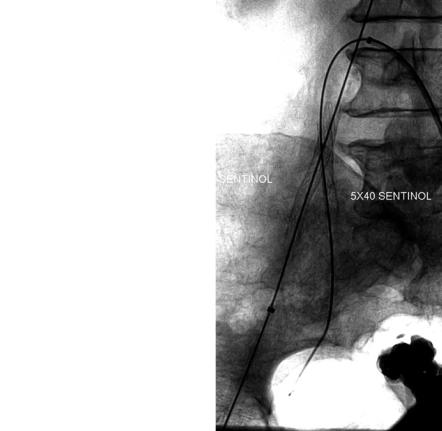
Fig. 12.4 After 48 h of thrombolysis, the right common iliac system was cleared of thrombus; however, there was still residual thrombus in the external iliac and hypogastric arteries.
Thrombolysis was continued in attempt to clear the residual thrombus
Question 7
During thrombolytic therapy for peripheral arterial occlusion, the most frequent compli cation is:
A. Pulmonary failure B. Myocardial infarction
C. Intracranial hemorrhage D. Vascular access bleeding
After 72 h of thrombolysis, there was still residual thrombus at the right hypogastric artery and external iliac artery origins (Fig. 12.5). Because of concerns over pelvic ischemia and residual thrombus in the left hypogastric artery, efforts were made to preserve the right hypogastric artery. The right hypogastric artery occlusion lesion was traversed from the left groin; the right groin was accessed and a second wire was positioned across the right external iliac artery (Fig. 12.6). From this position, opposing self-expanding stents were placed at the origins of both the external and internal iliac arteries restoring perfusion to the right lower extremity without embolization (Figs. 12.7 and 12.8).
The patient had palpable pedal pulses at completion of the procedure. In the postoperative period, a transesophageal echocardiogram documented cardiac thrombus as the source of aortoiliac embolization. She was discharged on anticoagulation.
12.1 Commentary
The etiology of acute limb ischemia can be classified into two groups. Thrombotic events occur in the setting of native arterial disease or bypass graft stenoses. In contrast, embolic phenomena usually occur in normal vessels and tend to lodge at arterial bifurcations.1

118 |
Z.M. Arthurs and V.S. Kashyap |
|
|
Fig. 12.5 After 72 h of thrombolysis, the residual clot remained at the origins of the external iliac artery and hypogastric artery
Fig. 12.6 Access was obtained from the right groin, and a wire was positioned retrograde across the external iliac thrombus. From the left groin, the right hypogastric artery was selected
Thrombotic occlusions are thought to represent progression of atherosclerotic disease and occur at sites along the arterial tree and most notably the superficial femoral artery at the adductor canal. In comparison, autologous grafts fail at sites of intimal hyperplasia, or fibrotic valves. Due to preexisting collaterals, native arterial thrombosis seldom presents with the profound ischemia seen with embolic ischemia. The presence of palpable pulses on the contralateral limb and a history of cardiac arrhythmia assist in differentiating acute embolus as opposed to thrombotic occlusions.1
12 Acute Thrombosis |
119 |
|
|
Fig. 12.7 Two self-expanding stents were deployed in an “opposing fashion” in order to maintain patency of both the external iliac and hypogastric arteries. The right hypogastric artery was treated because of concerns for pelvic ischemia and possible residual left hypogastric thrombus
[Q1: E] All of the factors listed can help in differentiating embolic versus thrombotic occlusions. Often, a definitive diagnosis cannot be made preoperatively. However, identifying an embolic source for acute limb ischemia is helpful both for the acute and long-term management of the patient.
Clinical classification and diagnosis of acute occlusion of the lower extremity is based on the symptoms of the patient. The severity of symptoms is associated with the extent of the occlusion and the presence of pre-existing vessels. Patients with thrombotic occlusions from underlyingdiseaseoftheSFAattheadductorcanalmayonlyexperienceworseningclaudicationwhileemboliceventsareusuallyassociatedwithrapidonsetandsevereischemiabecause of the lack of preexisting collateral flow. Limb ischemia has been classified into three categoriesbyanSVS/ISCVSadhoccommittee,basedonseverityofischemia.2 CategoryIlimbsare viable, not immediately threatened and have no motor or sensory loss. There are clearly audible arterial Doppler signals in the foot. Category II includes threatened limbs where salvage may be possible with timely intervention. Importantly, this category is divided into two subgroups, a and b which distinguish the time interval necessary for treatment. Group IIa require prompttreatmentwhereasGroupIIbneedimmediatetherapytopreventamputation.InGroup

120 |
Z.M. Arthurs and V.S. Kashyap |
|
|
Fig. 12.8 Completion imaging documents rapid flow through the aortoiliac system without any residual thrombus. Bilateral lower extremity runoff documented good runoff without embolization
II,audiblevenousDopplersignalsarepresent,butthereisnoarterialsignalinthefoot.Group IIa patients have minimal sensory loss and have no motor loss. However, patients with Group IIb ischemia, have muscle weakness, and sensory loss encompasses more than the toes. Category III is characterized by irreversible ischemia with profound and permanent neuromuscular damage where amputation may be the only recourse.
[Q2: C] This patient has Category IIb limb ischemia characterized by lack of distal arterial signals in the foot, sensory loss, and motor weakness. [Q3:C]Motor loss separates Category IIa from IIb ischemia and determines the urgency on which to proceed to revascularization.
The sequence of clinical events in patients with lower extremity ischemia is often predictable. [Q4: A] Most patients with acute ischemia, especially from of an embolic nature, will have pulselessness followed by pain and pallor. Paresthesia indicates sensory nerve ischemia and occurs usually from 1 to 3 h after the onset of acute ischemia. Paralysis indicatesmotornervedamagethatisoftenirreversible.Inthesettingofacuteischemiawithout collateral flow, paralysis occurs approximately 6 h after the onset of ischemia.3 Any motor dysfunction should be seen as a worrisome sign and should prompt urgent intervention. Poikilothermia indicates that the foot or limb has approximated ambient temperature. In these irreversible cases (Category III), amputation may be the only option and often has to be done quickly to avoid systemic complications.
Both the diagnosis and localization of acute arterial occlusion is based upon the findings on physical exam and imaging studies. A “waterhammer” pulse signifies outflow obstruction, as observed with a common femoral embolus. By contrast, calcified vessels
12 Acute Thrombosis |
121 |
|
|
are common with thrombosis from underlying atherosclerotic disease. Multiple options are available for localization of the occlusion. Noninvasive testing with segmental pressures, pulse volume recording and measurement of the ankle brachial indices can provide a baseline study for comparison after treatment. Both vertical and horizontal pressure gradients of 30 mmHg or more in the lower extremity can accurately identify the site of occlusion. Duplex ultrasonography can also be utilized to examine the femoral and popliteal vessels and localize area of occlusion. Other causes such as thrombosed popliteal aneurysm can be easily diagnosed in this manner. MRA and CTA are emerging as noninvasive techniques for arteriographic imaging and localization of thrombosis. However, angiography remains the gold standard for localization of arterial occlusion. As importantly, angiography allows percutaneous access to the site of thrombosis and an array of treatment options for restoring blood flow to the limb.
Treatment for limb ischemia has evolved over the past two decades with advances in both pharmacologic therapy and endovascular options. [Q5: B, C, D] In patients with acute limb ischemia secondary to iliac occlusion, operative thrombectomy of the occluded iliac system may be feasible. In the setting of profound ischemia and a diseased iliac artery precluding successful thrombectomy, extra-anatomic bypass can be performed to provide expeditious blood flow into the ischemic limb. In these cases, either femoral-femoral bypass or axillo-femoral bypass can be contemplated depending on the inflow source. Aortofemoral bypass is a very durable option for patients with chronic occlusion and chronic ischemia of the limb. However, in patients with acute ischemia ill-prepared for major surgery, proceeding with direct reconstruction with the aorta as the inflow is sometimes hazardous. Multiple endovascular devices are available in the setting of acute throm- bosis.Percutaneousmechanicalthrombectomywiththrombolysiseitherviathepower-pulse technique or via a standard infusion often quickly resolves the acute ischemia. Continued thrombolytic infusion is required for complete resolution of thrombus. Often, a “culprit” lesion will be unmasked by dissolving all of the acute thrombus, allowing percutaneous treatment of the offending lesion. Systemic thrombolytic therapy has been used to treat peripheral arterial occlusions, but results have been disappointing owing to a significant incidenceofbleedingcomplications.Currently,systemictherapyisusuallyusedforvenous thromboembolic states. Regional intravascular infusion of the lytic agent avoids some of the systemic complications and is largely used for peripheral arterial thromboses and graft occlusions. Because a systemic lytic state may occur with prolonged regional intravascular thrombolytictherapy,patientselectioniscritical.Absolutecontraindicationsincludeactive internal bleeding, recent surgery or trauma to the area to be perfused, recent cerebrovascular accident, or documented left heart thrombus.3 Relative contraindications include recent surgery, gastrointestinal bleeding or trauma, severe hypertension, mitral valve disease, endocarditis, hemostatic defects, or pregnancy.
[Q6: A, D, E] Several multicenter trials have examined groups of patients treated with surgical therapy or thrombolysis. The Rochester trial randomized patients to surgery or thrombolysis and demonstrated a lower mortality in the thrombolysis group.4 Following successful thrombolysis, unmasked “culprit lesions” were treated with angioplasty or surgery of a lesser magnitude, thereby reducing the severity of the intervention and overall morbidity. The finding of a lesion that precipitated the thrombosis is critical to avoiding re-thrombosis. The STILE trial (Surgery versus Thrombolysis for Ischemia of the Lower
122 |
Z.M. Arthurs and V.S. Kashyap |
|
|
Extremity) compared optimal surgical therapy to intraarterial catheter-directed thrombolysis for native arterial or bypass graft occlusions.5,6 Stratification by duration of ischemic symptoms revealed that patients with ischemia of less than 14 days duration had lower amputation rates with thrombolysis and shorter hospital stays, while patients with ischemia for longer than 14 days who were treated surgically had less ongoing or recurrent ischemia and trends toward lower morbidity. At 6 months, amputation-free survival was improved in patients with acute ischemia treated with thrombolysis, but patients with chronic ischemia had lower amputation rates when treated surgically. Fifty-five percent of patients treated with thrombolysis had a reduction in magnitude of their surgical procedure. Of note, no difference was seen between the use of rt-PA and urokinase.5
A multicenter, randomized, prospective trial comparing thrombolysis to surgery for acute lower extremity ischemia of less than 14 days duration has been performed. The Thrombolysis or Peripheral Arterial Surgery trial (TOPAS) randomized 757 patients to surgery or thrombolytic therapy.7 The most effective dose for recombinant urokinase was determined to be 4,000 U/min with complete thrombolysis in 71% (mean duration of therapy 24 ± 0.8 h) of patients. After successful thrombolytic therapy, either surgical or endovascular intervention was performed on the lesion responsible for the occlusion if found. When compared to the surgical arm, the 1-year limb salvage rates and mortality were not statistically different. However, although no statistical differences between the two groups were seen with respect to amputation-free survival, thrombolysis was associated with a reduction in the number and magnitude of open surgical interventions over a 1-year follow up period.
Perhaps, unlike thrombolysis in coronary or venous systems, dissolution of the larger peripheral arterial thrombi requires direct infusion of thrombolytic agent into the clot. The thrombosed artery or bypass graft must be accessed with a wire, followed by placement of an infusion system into the thrombus. There are multiple dosing regimens for urokinase (UK), t-PA and other thrombolytic agents. A plethora of strategies for thrombolysis have been used and are described in a consensus document.8 In this comprehensive review, 33 recommendations were made by a panel of experienced hematologists, radiologists, and vascularsurgeons fromNorthAmerica and Europe. Of note, over 40 dosageschemes were reviewed and described for thrombolytic infusion. This included strategies of continuous versus stepwise infusion, bolusing or lacing the clot, and intraoperative thrombolysis. The most popular strategies included using UK 4,000 u/min for 4 h, and then decreasing to 2,000 u/min for a maximum of 48 h, t-PA at a dose of 1 mg/h and lacing the clot to increase thrombolytic efficiency. Our preferred current technique is to use low-dose t-PA (0.5–1.0 mg/h) after initial percutaneous mechanical thrombectomy. Low-dose heparin (300–400 u/h) is infused via the arterial sheath side arm to prevent pericatheter thrombosis, but full anticoagulation is avoided.
Following successful thrombolysis, any unmasked lesion can be addressed with balloon angioplasty and stenting or with an open surgical procedure. Even when a surgical procedure is necessary, it can usually be performed electively, in a well-prepared patient and is often of a lesser magnitude than what would have been required without thrombolysis. Thrombolytic therapy is an effective option for selected patients with acute thrombotic occlusion.
