
- •Vascular Surgery
- •SECTION AND BOARD OF VASCULAR SURGERY
- •Foreword to the First Edition
- •Preface to the First Edition
- •Preface to the Second Edition
- •Preface to the Third Edition
- •Contents
- •Contributors
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •1.1 Commentary
- •1.2 Beta-Adrenergic Antagonists
- •1.3 3-Hydroxy-3-Methylglutaryl Coenzyme A Reductase Inhibitors (Statins)
- •1.4 Percutaneous Revascularization
- •1.5 Coronary Artery Bypass Grafting
- •References
- •2: Abdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •2.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •Question 13
- •Question 14
- •3.1 Commentary
- •3.2 Case Analysis Quiz
- •References
- •4: Ruptured Abdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •4.1 Commentary
- •References
- •5: Thoracoabdominal Aortic Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •5.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •Question 13
- •6.1 Commentary
- •References
- •7: Aortic Dissection
- •7.1 Dissection: Stanford A
- •Question 1
- •Question 2
- •Question 3
- •7.2 Dissection: Stanford B
- •Question 4
- •Question 5
- •7.3 Commentary
- •References
- •8: Popliteal Artery Aneurysms
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •8.1 Popliteal Artery Aneurysm
- •References
- •9: Renal Artery Aneurysm
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •9.1 Commentary
- •References
- •10: Anastomotic Aneurysms
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •10.1 Commentary
- •10.2 Indications for Intervention
- •10.3 Treatment for Anastomotic Aneurysms
- •10.4 Infection in Anastomotic Aneurysms
- •10.5 Outcome
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •11.1 Commentary
- •References
- •12: Acute Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •12.1 Commentary
- •References
- •13: Arterial Embolism
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •13.1 Commentary
- •References
- •14: Blast Injury to the Lower Limb
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •14.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •15.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Smoking
- •Antiplatelet Agents
- •Blood Pressure (BP)
- •Glucose Status
- •Lipids
- •Emerging Risk Factors
- •Question 4
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •17.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •18.1 Commentary
- •18.2 Clinical Assessment
- •18.3 Imaging Techniques
- •18.4 Revascularization Options
- •18.5 Aortobifemoral Bypass
- •18.6 Iliac Angioplasty and Stenting
- •18.7 Iliac Stenting Combined with Profunda Femoris Artery Revascularization
- •18.8 Rationale for Angioplasty of “Donor” Iliac Artery Prior to Femorofemoral Crossover Bypass
- •18.10 Supervision and Follow-up of the Patient
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •Question 12
- •19.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •20.1 Commentary
- •References
- •21: Bypass to the Popliteal Artery
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •21.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •22.1 Commentary
- •References
- •23: Popliteal Artery Entrapment
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •23.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •24.1 Commentary
- •References
- •25: The Obturator Foramen Bypass
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •25.1 Commentary
- •25.2 Preoperative Measures
- •25.3 The Concept of the Obturator Foramen Bypass
- •25.4 Obturator Foramen Bypass Technique
- •References
- •26: Diabetic Foot
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •26.1 Commentary
- •References
- •27: Chronic Visceral Ischemia
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •27.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •28.1 Commentary
- •References
- •29: Renovascular Hypertension
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •29.1 Commentary
- •29.4 Intra-arterial Angiography
- •29.5 Duplex Ultrasonography (DU)
- •29.6 Treatment
- •29.6.1 Medical Treatment
- •29.6.2 Revascularization
- •29.7 Prognosis
- •References
- •30: Midaortic Syndrome
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •30.1 Commentary
- •References
- •31: Management of Portal Hypertension
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •31.1 Commentary
- •31.2 General Considerations
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •32.1 Commentary
- •References
- •33: The Carotid Body Tumor
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •33.1 Commentary
- •33.2 Clinical Presentation
- •33.3 Treatment
- •33.4 Summary
- •References
- •Question 1
- •Question 2
- •Question 3
- •34.1 Commentary
- •34.2 Vertebrobasilar Ischemia: Low-Flow Mechanism
- •Question 1
- •Question 2
- •34.3 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •35.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •36.1 Commentary
- •References
- •37: Acute Axillary/Subclavian Vein Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •37.1 Commentary
- •References
- •38: Raynaud’s Phenomenon
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •38.1 Commentary
- •References
- •39: Aortofemoral Graft Infection
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •39.1 Commentary
- •References
- •40: Aortoenteric Fistulas
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •40.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •41.1 Commentary
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Questions 7 and 8
- •Question 9
- •Question 10
- •Comment
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •42.1 Commentary
- •References
- •43: Amputations in an Ischemic Limb
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •43.1 Commentary
- •References
- •44: Congenital Vascular Malformation
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •44.1 Clinical Evaluation
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •44.2 Commentary
- •References
- •45: Klippel-Trenaunay Syndrome
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •45.1 Commentary
- •Clinical Presentation
- •Evaluation
- •Treatment
- •References
- •46: Deep Venous Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •46.1 Commentary
- •References
- •47: Endoluminal Ablation of Varicose Veins
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •47.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •48.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •50.1 Commentary
- •References
- •51: Iliofemoral Venous Thrombosis
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •50.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •Question 11
- •52.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •Question 6
- •Question 7
- •Question 8
- •Question 9
- •Question 10
- •53.1 Commentary
- •References
- •Question 1
- •Question 2
- •Question 3
- •Question 4
- •Question 5
- •54.1 Commentary
- •References
- •Index

18 Lower Limb Claudication Due to Bilateral Iliac Artery Occlusive Disease |
197 |
|
|
femorofemoral bypass was deemed necessary in this case because of the extensive left femoralarterylesionsthatrenderanyattempttoleftiliacendovascularrecanalizationquite hazardous with the distal end of the stent below the inguinal ligament. As said previously, it is important to have for both angioplasty and open surgery an adequate outflow. The use of such a combined approach to lower extremity revascularization is not new and many authors reported excellent long-term results after combined iliac angioplasty/stenting and profunda or distal revascularization.24 [Q2:D]
18.10
Supervision and Follow-up of the Patient
A follow-up visit at yearly intervals with duplex evaluation and a structured or supervised walking program are essential in patients operated for CLI. Three concepts need to be explained to the patients: (1) A dedicated walking time should be tailored to each patient (e.g. 30–45 min, 3–5 days per week), (2) Walking instructions to walk at a comfortable pace and stop for a brief rest whenever leg pain becomes severe, (3) recording walking time, length and weight loss. This program should be associated with smoking cessation, use of statins and antiplatelet therapy.25 [Q3:F]
References
1. Criqui MH, Langer RD, Fronek A, et al. Mortality over a period of 10 years in patients with peripheral arterial disease. N Engl J Med. 1992;326:381-386.
2. McKenna M, Wolfson S, Kuller L. The ratio of ankle and arm arterial pressure as an independent predictor of mortality. Atherosclerosis. 1991;87:119-128.
3. Murabito JM, Evans JC, Nieto K, Larson MG, Levy D, Wilson PW. Prevalence and clinical correlates of peripheral arterial disease in the Framingham Offspring Study. Am Heart J. 2002;143:961-965.
4. Howell MA, Colgan MP, Seeger RW, Ramsey DE, Sumner DS. Relationship of severity of lower limb peripheral vascular disease to mortality and morbidity: a six-year follow-up study. J Vasc Surg. 1989;9:691-696.
5. Adam DJ, Beard JD, Cleveland T, et al. Bypass versus angioplasty in severe ischaemia of the leg (BASIL): multicentre, randomised controlled trial. Lancet. 2005;366:1925-1934.
6. Stoyioglou A, Jaff MR. Medical treatment of peripheral arterial disease: a comprehensive review. J Vasc Interv Radiol. 2004;15:1197-1207.
7. Schanzer A, Mega J, Meadows J, Samson RH, Bandyk DF, Conte MS. Risk stratification in critical limb ischaemia: derivation and validation of a model to predict amputation-free survival using multicenter surgical outcomes data. J Vasc Surg. 2008;48:1464-1471.
8. Schanzer A, Goodney PP, YouFu L, et al. Validation of the PIII CLI Risk Score for the predic- tionofamputation-freesurvivalinpatientsundergoingsurgicalbypassforcriticallimbischae- mia. J Vasc Surg. 2009;50:769-775.
9. Rose SC. Noninvasive vascular laboratory for evaluation of peripheral arterial occlusive disease. Part II. Clinical applications: chronic atherosclerotic, lower extremity ischaemia. J Vasc Interv radiol. 2000;11:1257-1275.
198 |
J.-B. Ricco and O. Page |
|
|
10.Brewster DC. Current controversies in the management of aortoiliac occlusive disease. J Vasc Surg. 1997;25:365-379.
11.Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA. Fowkes FGR on behalf of the TASC II working group. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg. 2007;33:S54-S57.
12.Pursell R, Sideso E, Magee TR, Galland RB. Critical appraisal of femorofemoral crossover grafts. Br J Surg. 2005;92:565-569.
13.Kim YW, Lee JH, Kim HG, Huh S. Factors affecting the long-term patency of crossover femorofemoral bypass graft. Eur J Vasc Endovasc Surg. 2005;30:376-380.
14.AbuRahma AF, Robinson PA, Cook CC, Hopkins ES. Selecting patients for combined femorofemoral bypass grafting and iliac balloon angioplasty and stenting for bilateral iliac disease. J Vasc Surg. 2001;33:S93-S99.
15.Ricco JB, Probst H, French University Surgeons Association. Long-term results of a multicenter randomized study on direct versus crossover bypass for unilateral iliac artery occlusive disease. J Vasc Surg. 2008;47:45-53.
16.Porter JM, Eidemiller LR, Dotter CT, Rosch J. Vetto RM. Combined arterial dilatation and femorofemoral bypass for limb salvage. Surg Gynecol Obstet. 1973;137:409-412.
17.Walker PJ, Harris JP. May J. Combined percutaneous transluminal angioplasty and extraanatomic bypass for symptomatic unilateral iliac occlusion with contralateral iliac artery stenosis. Ann Vasc Surg. 1991;5:209-217.
18.Shah RM, Peer RM, Upson JF, Ricotta JJ. Donor iliac angioplasty and crossover femorofemoral bypass. Am J Surg. 1992;164:295-298.
19.Perler BA, Williams GM. Does donor iliac artery percutaneous transluminal angioplasty or stent placement influence the results of femorofemoral bypass. Analysis of 70 consecutive cases with long-term follow-up. J Vasc Surg. 1996;24:363-370.
20.Schneider JR, Besso SR, Walsh DB, Zwolack RM, Cronenwett JL. Femorofemoral versus aortofemoral bypass. Outcome and hemodynamic results. J Vasc Surg. 1994;19:43-57.
21.Criado E, Burnham SJ, Tinsley EA, Johnson G, Keagy BA. Femorofemoral bypass graft: analysis of patency and factors influencing long-term outcome. J Vasc Surg. 1993;18: 495-505.
22.Brewster DC, Cambria RF, Darling RC, et al. Long-term results of combined iliac balloon angioplasty and distal surgical revascularization. Ann Surg. 1989;210:324-331.
23.Marin ML, Veith FJ, Sanchez LA, et al. Endovascular aortoiliac grafts in combination with standard infrainguinal arterial bypasses in the management of limb-threatening ischemia. J Vasc Surg. 1995;22:316-325.
24.Cynamon J, Marin ML, Veith FJ, et al. Stent-graft repair of aortoiliac occlusive disease coexisting with common femoral artery disease. J Vasc Interv Radiol. 1997;8:19-26.
25.Heart Protection Study Collaborative Group. Randomised trial of the effects of cholesterollowering with simvastatin on peripheral vascular and other major vascular outcomes in 20, 536 people with peripheral arterial disease and other high-risk conditions. J Vasc Surg. 2007;45:645-654.

Endovascular Management of Lower Limb |
19 |
Claudication due to Infra-Inguinal Disease |
Daniel J. Reddy and Mitchell R. Weaver
An unemployed 56 year old man presents with several months duration of worsening left calf pain upon ambulation. After less than ½ block he must cease walking owing to the calf and foot pain which is relieved by rest. Occasionally he has nocturnal rest pain affecting his left foot. The patient must rely on walking for transportation and the activities of daily life. Past medical history is significant for 45 pack-years of tobacco cigarette smoking, bronchitis, hypertension, hyperlipidemia, previous polysubstance abuse and extensive varicose veins of both lower extremities. Serology is positive for syphilis and hepatitis C.
Physical exam: both femoral pulses are palpable as is the right popliteal pulse. The left popliteal and both dorsalis pedis and posterior tibial pulses are absent to palpation. The envelope of skin is intact and there is normal motor and sensory functionofbothlowerextremities.Pertinentmedicationsincludeclopidogrel,amlodipine and hydrochlorothiazide. The referring physician has initiated narcotic pain medicines for the rest pain. The serum creatinine is normal.
Question 1
Which of the following would be the optimal management plan?
A. Primaryamputationoftheleftlegtocontroltherestpainandavoidrelapseintonarcotic addiction
B. Risk factor modification, lower extremity non-invasive arterial studies and plans for angiography
C. Smoking cessation clinic referral and follow up in 4–6 months D. Initiate supervised exercise program and return in 6 months E. A 6 week trial of pentoxifylline or cilostazol
D.J. Reddy ( )
Department of Surgery, Wayne State University, Detroit, MI, USA
G. Geroulakos and B. Sumpio (eds.), Vascular Surgery, |
199 |
DOI: 10.1007/978-1-84996-356-5_19, © Springer-Verlag London Limited 2011 |
|
200 |
D.J. Reddy and M.R. Weaver |
|
|
The patient agrees to attend the smoking cessation clinic and will go to see the exercise therapist as well. You have applied for approval to prescribe pentoxifylline. Moreover, you have counseled the patient about the seriousness of his condition and the threat it poses to the viability of his left leg. After segmental arterial pressure studies are obtained, you discuss the pros and cons of diagnostic and possible interventional angiography and recommended it to him. He gives his informed consent.
Question 2
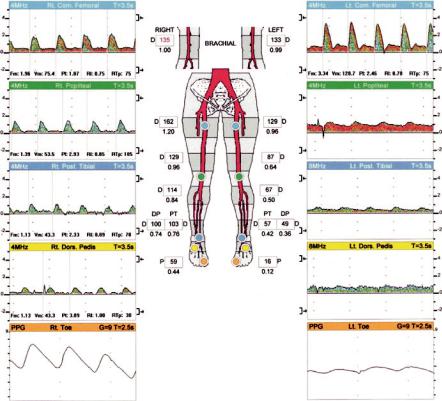
What do these lower extremities non-invasive segmental arterial studies demonstrate? (Fig . 19.1)
A. Moderate occlusive disease on the right and much more severe disease on the left B. Normal study
C. Mild to moderate occlusive arterial disease on the left
D. Normal waveforms on the right and slight dampening of the waveforms on the left E. Incompressibility consistent with diabetes mellitus and, therefore, not diagnostic
Fig. 19.1 Presenting lower extremity segmental arterial pressures
