
Книги по МРТ КТ на английском языке / PLUM AND POSNER S DIAGNOSIS OF STUPOR AND COM-1
.pdf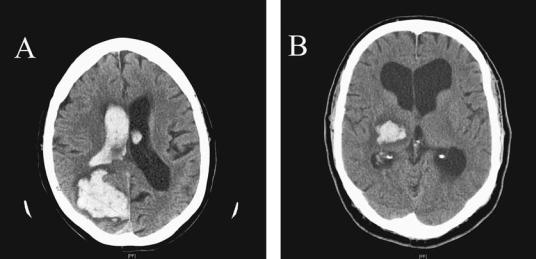
136 Plum and Posner’s Diagnosis of Stupor and Coma
cerebral end arteries, trauma, rupture of an arteriovenous malformation, rupture of a mycotic aneurysm, amyloid angiopathy, or hemorrhage into a tumor. Rupture of a saccular aneurysm can also cause an intraparenchymal hematoma, but the picture is generally dominated by the presence of subarachnoid blood. In contrast, despite their differing pathophysiology, the signs and symptoms of primary intracerebral hemorrhages are due to the compressive effects of the hematoma, and thus are more alike than different, depending more on location than on the underlying pathologic process. Spontaneous supratentorial intracerebral hemorrhages are therefore usually classified as lobar or deep, with the latter sometimes extending intraventricularly.
Lobar hemorrhages can occur anywhere in the cerebral hemispheres, and may involve one or multiple lobes (Figure 4–6A). As compared to deeper hemorrhages, patients with lobar hemorrhages are older, less likely to be male, and less likely to be hypertensive. Severe headache is a characteristic of lobar hemorrhages. Focal neurologic deficits occur in almost 90% of patients and vary somewhat depending on the site of the hemorrhage. About half the patients have a decreased level of conscious-
ness and 20% are in a coma when admitted.99 Seizures are a common occurrence and may be nonconvulsive (see page 281), so that electroencephalographic (EEG) evaluation is valuable if there is impairment of consciousness.
Deep hemorrhages in the supratentorial region include those into the basal ganglia, internal capsule, and thalamus. Hemorrhages into the pons and cerebellum are discussed in the section on infratentorial hemorrhages. Chung and colleagues divided patients with striatocapsular hemorrhages into six groups with varying clinical findings and prognoses.100 These included posterolateral (33%), affecting primarily the posterior portion of the putamen; massive (24%), involving the entire striatal capsular region but occasionally sparing the caudate nucleus and the anterior rim of the internal capsule; lateral (21%), located between the external capsule and insular cortex; anterior (11%), involving the caudate nucleus; middle (7%), involving the globus pallidus in the middle portion of the medial putamen; and posterior medial (4%), localized to the anterior half of the posterior rim of the internal capsule. Consciousness was only rarely impaired in anterior and posterior medial lesions, but was impaired in about one-third of patients
Figure 4–6. Computed tomography scans from two patients with intracerebral hemorrhages. (A) shows a large hemorrhage into the right parieto-occipital lobe in a 77-year-old woman who was previously healthy and presented with difficulty walking and a headache. Examination showed left-sided neglect. She took 325 mg aspirin at home on the advice of her primary care doctor because she suspected a stroke. The hematoma ruptured into the lateral ventricle. (B) shows a right thalamocapsular hemorrhage in a 60-year-old man with a history of hypertension who was not being treated at the time of the hemorrhage. He presented with headache, left-sided weakness and sensory loss, and some left-sided inattention.
with middle lesions. About half the patients with posterolateral lesions were drowsy, but not comatose, as were about one-half the patients with the lateral lesions who rarely become comatose. However, massive lesions usually cause severe impairment of consciousness including coma. Hemiparesis is common in posterolateral and massive lesions. Sensory deficits are relatively frequent in posterior and medial lesions. Prognosis is fair to good in patients with all of the lesions save the massive ones, where the fatality rate is about 50%. Eye deviation occurs usually toward the lesion site, but may be ‘‘wrong way’’ in those with posterolateral and massive lesions.
Thalamic hemorrhages can be categorized by size (smaller or larger than 2 cm in diameter) and by location (posterolateral, anterolateral, medial, and dorsal; Figure 4–6B). About one-fifth of patients with thalamic hemorrhages are stuporous or comatose at presentation.101 The loss of consciousness is usually accompanied by ocular signs including skew deviation (the lower eye on the side of the lesion); gaze preference, which may either be toward or away (wrong-way eyes) from the side of the lesion; loss of vertical gaze; and miotic pupils. ‘‘Peering at the tip of the nose’’ is an almost pathognomonic sign.102 Sensory and motor disturbances depend on the site and size of the lesion. About 25% of patients die,101 and the outcome is related to the initial consciousness, nuchal rigidity, size of the hemorrhage, and whether the hemorrhage dissects into the lateral ventricle or causes hydrocephalus.101
Intraventricular hemorrhages may be either primary or result from extension of an intracerebral hemorrhage. Intraventricular hemorrhages were once thought to be uniformly fatal, but since the advent of CT scanning, have been shown to run the gamut of symptoms from simple headache to coma and death.103 Primary intraventricular hemorrhages can result from vascular anomalies within the ventricle, surgical procedures, or bleeding abnormalities.104 Clinical findings include sudden onset of headache and vomiting sometimes followed by collapse and coma. If the hemorrhage finds its way into the subarachnoid space, nuchal rigidity occurs. The clinical findings of secondary intraventricular hemorrhage depend on the initial site of bleeding. Hemorrhage into the ventricle from a primary intracerebral hemorrhage worsens the prognosis.
Specific Causes of Structural Coma |
137 |
The treatment of intraventricular hemorrhage is aimed at controlling intracranial pressure. Ventricular drainage may help, but the catheter often becomes occluded by the blood. Injection of fibrinolytic agents (such as t-PA) has been recommended by some.104
The treatment of an intracerebral hemorrhage is controversial. Early surgery to evacuate the hematoma has not been associated with better outcome.105 However, treatment with hemostatic drugs, such as recombinant factor VIIa, which limit hematoma size, are associated with improved outcomes.106 Most patients who have relatively small lesions and do not die make good recoveries; those with massive lesions typically either die or are left devastated. Herniation should be treated vigorously in patients with relatively small hematomas because of the potential for good recovery.
Despite these similarities, the clinical setting in which one sees patients with intracerebral hemorrhage depends on the pathologic process involved. These include rupture of a deep cerebral endartery, amyloid angiopathy, mycotic aneurysm, arteriovenous malformation, or hemorrhage into a tumor, and each requires a different clinical approach.
Box 4–1 summarizes the major points that differentiate clinically between acute cerebral vascular lesions potentially causing stupor or coma.
Rupture of deep cerebral end arteries usually occurs in patients with long-term, poorly treated hypertension; it can also complicate diabetes or other forms of atherosclerotic arteriopathy. The blood vessels that are most likely to hemorrhage are the same ones that cause lacunar strokes (i.e., end arteries that arise at a right angle from a major cerebral artery): the striatocapsular arteries, which give rise to capsular and basal ganglionic bleeds; the thalamic perforating arteries, which give rise to thalamic hemorrhages; the midline perforating arteries of the pons, which give rise to pontine hemorrhages; and the penetrating branches of the cerebellar long circumferential arteries, which cause cerebellar hemorrhages. We will deal with the first two, which cause supratentorial masses, in this section, and the latter two in the section on infratentorial masses.
The focal neurologic findings in each case are characteristic of the part of the brain that is injured. Capsular or basal ganglionic hemorrhages typically present with the acute onset of
Box 4–1 Typical Clinical Profiles of Acute Cerebrovascular Lesions Affecting Consciousness
Acute massive cerebral infarction with or without hypotension
Distribution: Internal carotid-proximal middle cerebral artery or middle cerebral plus anterior cerebral arteries. Onset during wakefulness or sleep. Massive hemiplegia with aphasia, hemisensory defect. Obtundation from the start or within hours, progressing to stupor in 12 to 24 hours, coma usually in 36 to 96 hours. Convulsions rare. Pupils small and reactive, or constricted ipsilateral to lesion (Horner’s), or moderately dilated ipsilateral to lesion (III nerve). Conjugate gaze paresis to side of motor weakness; contralateral oculovestibulars can be suppressed for 12 hours or so. Contralateral hemiplegia, usually with extensor plantar response and paratonia ipsilateral to lesion. Cheyne-Stokes breathing 10% to 20%. Signs of progressive rostral caudal deterioration begin in 12 to 24 hours. Spinal fluid usually unremarkable or with mildly elevated pressure and cells.
Frontoparietal hemorrhage
Onset during wakefulness. Sudden-onset headache, followed by more or less rapidly evolving aphasia, hemiparesis to hemiplegia, conjugate ocular deviation away from hemiparesis. Convulsions at onset in approximately one-fifth. Pupils small and reactive, or ipsilateral Horner’s with excessive contralateral sweating, or stupor to coma and bilateral motor signs within hours of onset. Bloody spinal fluid.
Thalamic hemorrhage
Hypertensive, onset during wakefulness. Clinical picture similar to frontoparietal hemorrhage but seizures rare, vomiting frequent, eyes characteristically deviated down and laterally to either side. Pupils small and reactive. Conscious state ranges from awake to coma. Bloody spinal fluid.
Bilateral thalamic infarction in the paramedian regions
Sudden onset of coma, akinetic mutism, hypersomnolence or altered mental status may accompany bland infarcts of the paramedian thalamus arising bilaterally as a result of a ‘‘top of the basilar’’ syndrome or a branch occlusion of a thalamopeduncular artery (Percheron’s artery) providing vascular supply to both thalami and often the tegmental mesencephalon.
Pontine hemorrhage
Hypertensive. Sudden onset of coma or speechlessness, pinpoint pupils, ophthalmoplegia with absent or impaired oculovestibular responses, quadriplegia, irregular breathing, hyperthermia. Bloody spinal fluid.
Cerebellar hemorrhage
Hypertensive and awake at onset. Acute and rapid onset and worsening within hours of occipital headache, nausea and vomiting, dizziness or vertigo, unsteadiness, dysarthria, and drowsiness. Small and reactive pupils, nystagmus or horizontal gaze paralysis toward the side of the lesion. Midline and ipsilateral ataxia, (continued)
138

Specific Causes of Structural Coma |
139 |
ipsilateral peripheral facial palsy, and contralateral extensor plantar response. Occasionally, course may proceed for 1 to 2 weeks. Spinal fluid bloody.
Acute cerebellar infarction
Mostly hypertensive, mostly males. Onset at any time. Vertigo, ataxia, nausea, dull headache, nystagmus, dysarthria, ipsilateral dysmetria; 24 to 96 hours later: drowsiness, miosis, ipsilateral gaze paresis and facial paresis, worsening ataxia, extensor plantar responses. Coma, quadriplegia, and death may follow if not decompressed. Spinal fluid sometimes microscopically bloody.
Acute subarachnoid hemorrhage
Awake at onset, sometimes hypertensive, sudden headache, often followed within minutes by unconsciousness. Pupils small or unilaterally dilated. Subhyaloid hemorrhages, hemiparesis or aphasia may or may not be present, hemisensory changes rare. Neck stiff within 24 hours. Bloody spinal fluid.
hemiplegia. Thalamic hemorrhage may present with sensory phenomena, but often the hemorrhage compresses ascending arousal systems early so that loss of consciousness is the primary presentation.101 When the hemorrhage is into the caudal part of the thalamus, such as the putamen, which overlies the posterior commissure, the initial signs may be due to dorsal midbrain compression or injury102 (see page 110), with some combination of forced downgaze and convergence (‘‘peering at the tip of the nose’’), fixed pupils, and retractory nystagmus. Another neuro-ophthalmologic presentation of thalamic hemorrhage was described by Miller Fisher as ‘‘wrong-way eyes.’’107 Whereas frontal lobe insults usually result in deviation of the eyes toward the side of the lesion (i.e., paresis of gaze to the opposite side of space), after thalamic hemorrhage (or occasionally deep intraparenchymal hemorrhage that damages the same pathways108) there may be a paresis of gaze toward the side of the lesion (see Chapter 3).
PATHOPHYSIOLOGY
Hemorrhages of the end artery type are often called hypertensive hemorrhages, although they may occur in other clinical settings. The reason for the predilection of this class of artery for both occlusion (lacunar infarction) and hemorrhage is not known. Miller Fisher attempted to identify the arteries that had caused lacunar
infarctions in postmortem examination of the brain.109 He found an eosinophilic degeneration of the wall of small penetrating arteries in the region of the infarct and proposed that this ‘‘lipohyalinosis’’ was the cause of the infarction. However, this description was based on a small number of samples and did not give any insight into the nature of the pathologic process. Given the fact that such vessels typically take off at a right angle from large cerebral arteries, one might expect high sheering forces at the vessel origin, so that high blood pressure or other atherosclerotic risk factors might cause earlier or more severe damage. However, the mechanism for this phenomenon remains unclear.
End artery hemorrhages typically produce a large hematoma with considerable local tissue destruction and edema. Because much of the clinical appearance is due to the mass effect, which eventually is resorbed, the patient may initially to be much more neurologically impaired than would be caused by a comparably sized infarct. However, if the patient can be supported through the initial event, recovery is often much greater than might be initially anticipated, and the hematoma is resorbed, leaving a slit-like defect in the brain.
Amyloid angiopathy results from deposition of beta-amyloid peptide in the walls of cerebral blood vessels.110 These deposits disrupt the arterial elastic media resulting in predisposition to bleeding. Because amyloid deposits occur along blood vessels as they penetrate the
140 Plum and Posner’s Diagnosis of Stupor and Coma
cerebral cortex, the hemorrhages are typically lobar (i.e., into a specific lobe of the cerebral cortex).111 The arteries that hemorrhage tend to be small vessels, which seal spontaneously, so that the patient usually survives but may have multiple recurrences in later years.112 Acute onset of focal hemispheric signs and a headache are the most common presentation. As with end artery hemorrhages, the severity of the initial presentation often is misleading, and as the hemorrhage is resorbed, there may be much greater return of function than in a patient with a similarly placed infarction. Gradient echo MRI may reveal additional areas of small, subclinical cortical and subcortical hemorrhage.113
Mycotic aneurysms are typically seen in the setting of a patient who has subacute bacterial endocarditis.114 Infected emboli that reach the brain lodge in small penetrating arteries in the white matter just deep to the cerebral cortex. The wall of the blood vessel is colonized by bacteria, resulting in aneurysmal dilation several millimeters in diameter. These aneurysms, which may be visualized on cerebral angiography, may be multiple. Because there may be multiple mycotic aneurysms, and to eliminate an arteriovenous malformation or saccular aneurysm as the source, an angiogram is generally necessary. Unruptured mycotic aneurysms are treated by antibiotics, but ruptured aneurysms may require endovascular or open surgical intervention.115
Vascular malformations may occur in any location in the brain. They range from small cavernous angiomas to large arteriovenous malformations that are life threatening. MRI identifies many more cavernous angiomas than are seen on conventional arteriography or CT scanning. The abnormal vessels in these malformations are thin-walled, low-pressure and lowflow venous channels. As a result, cavernous angiomas bleed easily, but rarely are life threatening. Cavernous angiomas of the brainstem may cause coma if they hemorrhage and have a tendency to rebleed.116 They can often be removed successfully.117 Radiosurgery may also
reduce the risk of hemorrhage, but can cause local edema or even hemorrhage acutely.118,119
Complex arteriovenous malformations (AVMs) contain large arterial feeding vessels and are often devastating when they bleed.120 Although somewhat less likely to cause im-
mediate death than are saccular aneurysms, arteriovenous malformations may be much harder to treat and bleeding may recur multiple times with gradually worsening outcome. AVMs may also cause symptoms by inducing epilepsy, or by causing a vascular steal from surrounding brain. AVMs that come to attention without hemorrhage have about a 2% to 4% per year chance of bleeding, but those that have previously bled have a much higher risk. AVMs are typically treated by a combination of endovascular occlusion of the arterial supply followed, if necessary, by surgery, although radiosurgery may also shrink AVMs in inaccessible regions.
Hemorrhage into a tumor typically occurs in the setting of a patient with known metastatic cancer. However, in some cases, the hemorrhage may be the first sign of the tumor. A higher percentage of metastatic melanoma, thyroid carcinoma, renal cell carcinoma, and germ cell tumors hemorrhage than is true for other tumor types, but lung cancer is so much more common than these tumors that it is the single most common cause of hemorrhage into a tumor.121 Primary brain tumors, particularly oligodendrogliomas, may also present with a hemorrhage into the tumor. Because it is often difficult to see contrast enhancement of the tumor amidst the initial blood on MRI or CT scan, it is generally necessary to reimage the brain several weeks later, when the acute blood has been resorbed, if no cause of the hemorrhage is seen on initial imaging.
Intracerebral Tumors
Both primary and metastatic tumors may in-
vade the brain, resulting in impairment of consciousness.121,122 Primary tumors are typically
either gliomas or primary CNS lymphomas, whereas metastatic tumors may come from many types of systemic cancer. Certain principles apply broadly across these classes of tumors.
Gliomas include both astrocytic tumors and oligodendrogliomas.122 Astrocytic tumors typically invade the substance of the brain, and in extreme cases (gliomatosis cerebri), may diffusely infiltrate the entire brain.123 Oligodendrogliomas typically are slower growing, and may contain calcifications visible on CT or MRI.
They more often present as seizures than as mass lesions.124 Astrocytomas typically present either with seizures or as a mass lesion, with headache and increased intracranial pressure. In other cases, the patients may present with focal or multifocal signs of cerebral dysfunction. As they enlarge, astrocytomas may outgrow their blood supply, resulting in internal areas of necrosis or hemorrhage and formation of cystic components. Impairment of consciousness is usually due to compression or infiltration of the diencephalon or herniation. Surprisingly, primary brainstem astrocytomas, which are typically seen in adolescents and young adults, cause mainly impairment of cranial motor nerves while leaving sensory function and consciousness intact until very late in the course.
Primary CNS lymphoma (PCNSL) was once considered to be a rare tumor that was seen mainly in patients who were immune suppressed; however, PCNSL has increased in frequ-
ency in recent years in patients who are not immune compromised.123,125 The reason for the
increased incidence is not known. PCNSL behaves quite differently from systemic lymphomas.122 The tumors invade the brain much like astrocytic tumors. They often occur along the ventricular surfaces and may infiltrate along white matter tracts. In this respect, primary CNS lymphomas present in ways that are similar to astrocytic tumors. However, it is unusual for a primary CNS lymphoma to reach so large a size, or to present by impairment of consciousness, unless it begins in the diencephalon.
Metastatic tumors are most often from lung, breast, or renal cell cancers or melanoma.121 Tumors arising below the diaphragm usually do not invade the brain unless they first cause pulmonary metastases. Unlike primary brain tumors, metastases rarely infiltrate the brain, and can often be shelled out at surgery. Metastatic tumors usually present either as seizures or as mass lesions, and often enlarge quite rapidly. This tendency also results in tumors outgrowing their blood supply, resulting in infarction and hemorrhage (see previous section).
The ease of removing metastatic brain tumors has led to some controversy over the optimal treatment. Patients who have solitary metastatic tumors removed on average survive longer than patients who are treated with corticosteroids and radiation.126 Occasional pa-
Specific Causes of Structural Coma |
141 |
tients with lung cancer may have long-term survival and even apparent cure has been reported after removal of a single brain metastasis as well as the lung primary tumor. Patients with brain tumors frequently suffer from seizures, but prophylactic administration of anticonvulsants has not been found to be of value.127 Small, surgically inaccessible metastases can be treated by stereotactic radiosurgery.128
Brain Abscess and Granuloma
A wide range of microorganisms, including viruses, bacteria, fungi, and parasites, can invade the brain parenchyma, producing an acute destructive encephalitis (see page 156). However, if the immune response is successful in containing the invader, a more chronic abscess or granuloma may result, which may act more as a compressive mass.
A brain abscess is a focal collection of pus within the parenchyma of the brain. The infective agents reach the brain hematogenously or by direct extension from an infected contiguous organ (paranasal sinus, middle ear).129 Most bacterial brain abscesses occur in the cerebral hemispheres, particularly in the frontal or temporal lobes. In many countries in Central and South America, cysticercosis is the most common cause of infectious mass lesions in the cerebral hemispheres. However, cysticercosis typically presents as seizures, and only occasionally as a mass lesion.130 In countries in which sheep herding is a major activity, echinococcal (hydatid) cyst must also be considered, although these can usually be recognized because they are more cystic in appearance than abscesses on CT or MRI scan.131 Patients with HIV infection present a special challenge in the diagnosis of coma, as they may have a much wider array of cerebral infectious lesions and are also disposed to primary CNS lymphoma. However, toxoplasmosis is so common in this group of patients that most clinicians begin with 2 weeks of therapy for that organism.132 When the appearance on scan is unusual, though, early biopsy is often indicated to establish the cause of the lesion(s) and optimal mode of treatment.
Other organisms may cause chronic infection resulting in formation of granulomas that
142 Plum and Posner’s Diagnosis of Stupor and Coma
Table 4–6 Presenting Signs and
Symptoms in 968 Patients With
Brain Abscess
|
Frequency |
|
Sign or Symptom |
Range |
Mean |
|
|
|
Headache |
55%–97% |
77% |
Depressed consciousness |
28%–91% |
53% |
Fever |
32%–62% |
53% |
Nausea with vomiting |
35%–85% |
51% |
Papilledema |
9%–56% |
39% |
Hemiparesis |
23%–44% |
36% |
Seizures |
13%–35% |
24% |
Neck stiffness |
5%–41% |
23% |
From Kastenbauer et al.,133 with permission.
may reach sufficient size to act as a mass lesion. These include tuberculomas in tuberculosis, torulomas in cryptococcal infection, and gummas in syphilis.
Because the symptoms are mainly due to brain compression, the clinical symptoms of brain abscess are similar to those of brain neoplasms, except they usually evolve more rapidly (Table 4–6).
Headache, focal neurologic signs, and seizures are relatively common. Fever and nuchal rigidity are generally present only during the early encephalitic phase of the infection, and are uncommon in encapsulated brain abscesses. The diagnosis may be suspected in a patient with a known source of infection or an immunosuppressed patient.
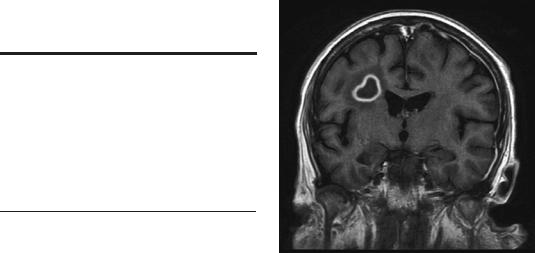
On imaging with either CT or MRI, the enhanced rim of an abscess is usually thinner and more regular than that of a tumor and may be very thin where it abuts the ventricle, sometimes leading to ventricular rupture (Figure 4–7). The infective nidus is often surrounded by more vasogenic edema than usually surrounds brain neoplasms. Diffusion-weighted images indicate restricted diffusion within the abscess, which can be distinguished from the cystic areas within tumors, which represent areas of infarction. The presence of higher levels of amino acids within the abscess on magnetic resonance spectroscopy (MRS) may also be helpful in differentiating the pathologies (Table 4–7).
Figure 4–7. A 49-year-old man with AIDS was admitted for evaluation of headache, nausea, and bilateral weakness and intermittent focal motor seizures. MRI showed multiple ring-enhancing lesions. Note that the smooth, contrast-enhancing wall of this right parietal lesion is typical of an abscess. He was treated with broad spectrum antibiotics and improved.
If the lesion is small and the organism can be identified, antibiotics can treat the abscess successfully. Larger lesions require drainage or excision.
INFRATENTORIAL COMPRESSIVE LESIONS
The same mass lesions that affect the supratentorial space can also occur infratentorially (i.e., in the posterior fossa). Hence, while both the focal symptoms caused by posterior fossa masses and the symptoms of herniation differ substantially from those of supratentorial masses, the pathophysiologic mechanisms are similar. For that reason, we will focus in this section on the ways in which posterior fossa compressive lesions differ from those that occur supratentorially. Depending on the site of the lesion, compressive lesions of the posterior fossa are more likely to cause cerebellar signs and eye movement disorders and less likely to cause isolated hemiplegia. Herniation may be either downward as the cerebellar tonsils are forced through the foramen magnum or upward as the cerebellar vermis pushes the up-

|
|
Specific Causes of Structural Coma |
143 |
|
Table 4–7 Imaging Findings in Brain Abscess |
|
|
||
|
|
|
|
|
Finding |
CT |
MR* |
Sensitivity |
|
|
|
|
|
|
Capsule |
Isodense |
T1WI: Isointense to hyperintense |
Plain: MR>CT |
|
|
|
Enhances T2WI: Hypointense |
CE: MR>CT |
|
|
|
to hyperintense |
|
|
Vasogenic edema |
Hypodense |
T1WI: Hypointense |
Plain: MR>CT |
|
|
|
T2WI: Hyperintense |
|
|
Abscess contents |
Hypodense |
T1WI: Hypointense |
Plain: MR ¼ CT |
|
|
|
T2WI: Hyperintense |
|
|
|
|
MRS: Amino acid, lactate, |
|
|
acetate, succinate, and pyruvate peaks
DWI: Bright (white) ADC: Dark (black)
ADC, apparent diffusion coefficient map; CE, contrast enhanced; CT, computed tomography; DWI, diffusion-weighted image; MR, magnetic resonance spectroscopy; T1WI, T1-weighted image; T2WI, T2-weighted image.
*Intensity relative to normal brain.
From Zimmerman et al.,98 with permission.
per brainstem through the tentorium, or usually both.
EPIDURAL AND DURAL MASSES
Epidural Hematoma
Epidural hematomas of the posterior fossa are much less common than their supratentorial counterparts, representing about 10% of all epidural hematomas.134 Posterior fossa epidural hematomas typically follow fracture of the occipital bone; they are usually arterial, but may occasionally result from venous bleed-
ing.135 The hematomas are bilateral in about one-third of cases.134
Patients present with headache, nausea and vomiting, and loss of consciousness.136,137 Neuro-ophthalmologic signs are relatively uncommon, usually consisting of abducens paresis due to the increased intracranial pressure. Occasionally a stiff neck is seen as an early sign of tonsillar herniation.
A typical lucid interval occurs in only a minority of patients138: after initial injury, those patients either continue to be alert or rapidly recover after a brief loss of consciousness only to subsequently, after minutes to days, first become lethargic and then lapse into coma. Without treatment death ensues from acute respi-
ratory failure (tonsillar herniation). Even those patients with a lucid interval suffer headache and often cerebellar ataxia after the injury. If not treated, symptoms progress to vertigo, stiff neck, ataxia, nausea, and drowsiness.
It is important to identify an occipital fracture even in the absence of a hematoma because of the possibility of delayed development of an epidural hematoma.134 If a fracture crosses the transverse sinus, it may cause thrombosis of that vessel, causing a supratentorial hemorrhagic infarct or increased ICP. Because of the small amount of space in the posterior fossa and the narrow exit foramina of CSF (Sylvian aqueduct and fourth ventricle), obstructive hydrocephalus is often an early problem that may require emergent therapy.139 About one-half of patients have evidence of other injury, such as cerebellar hemorrhage or supratentorial bleeding.140
Most patients with posterior fossa epidural hematomas are treated surgically,134 although alert patients with small lesions may be treated conservatively.141 A hematoma with a volume under 10 mL, a thickness under 15 mm, and a midline shift of no more than 5 mm may be treated conservatively but requires careful watching for increase in the size of the lesion. In the supratentorial space, epidural hematomas with volumes up to 30 mL may be treated conservatively.141 The availability of rapid
144 Plum and Posner’s Diagnosis of Stupor and Coma
imaging has substantially reduced the mortality from about 25% in older series142 to about 5% in more modern series.134 Most current mortality and morbidity is related not to the hematoma, but to other brain injuries sustained in the trauma.
Epidural Abscess
Epidural abscesses in the posterior fossa are rare, representing only nine out of almost 4,000 patients with intracranial infections in one series.143 Most were complications of ear infections and mastoiditis. Unlike epidural hematomas, fever and meningismus, as well as evidence of a chronic draining ear, are common. Focal neurologic signs are similar to those of epidural hematomas, but develop over days to weeks rather than hours. Cerebellar signs occur in a minority of patients. The CT scan demonstrates a hypodense or isodense extraaxial mass with a contrast-enhancing rim. Hydrocephalus is common. Diffusion-weighted MRI identifies restricted diffusion, as in supratentorial empyemas and abscesses.41 The prognosis is generally good with evacuation of the abscess and treatment with antimicrobials, except in those patients suffering venous sinus thrombosis as a result of the infection.
Dural and Epidural Tumors
As with supratentorial lesions, both primary and metastatic tumors can involve the dura of the posterior fossa. Meningioma is the most common primary tumor.144 Meningiomas usually arise from the tentorium or other dural structures, but can occur in the posterior fossa without dural attachment.145 Meningiomas produce their symptoms both by direct compression and by causing hydrocephalus. However, because they grow slowly, focal neurologic symptoms are common and the diagnosis is generally made long before they cause alterations of consciousness. Dural metastases from myelocytic leukemia, so-called chloromas or granulocytic sarcomas,146 have a particular predilection for the posterior fossa. Although more rapidly growing than primary tumors, these tumors rarely cause alterations of consciousness. Other metastatic tumors to the pos-
terior fossa meninges may cause symptoms by involving cranial nerves.
SUBDURAL POSTERIOR FOSSA COMPRESSIVE LESIONS
Subdural hematomas of the posterior fossa are rare. Only 1% of traumatic acute subdural hematomas are found in the posterior fossa.147 Chronic subdural hematomas in the posterior fossa, without a clear history of head trauma, are even rarer. A review in 2002 reported only 15 previous cases, including those patients taking anticoagulants.148 Patients with acute subdural hematomas can be divided into those who are stuporous or comatose on admission and those who are alert. Patients with chronic subdural hematomas, many of whom had been on anticoagulation therapy or have sustained very mild head trauma, usually present with headache, vomiting, and cerebellar signs. The diagnosis is made by CT or MRI and treatment is usually surgical. Stupor or coma portends a poor outcome, as do the CT findings of obliterated basal cisterns and fourth ventricle with resultant hydrocephalus.147
Subdural Empyema
Posterior fossa subdural empyemas are rare.149 They constitute less than 2% of all subdural empyemas.143 Like their epidural counterparts, ear infections and mastoiditis are the major cause. Headache, lethargy, and meningismus are common symptoms. Ataxia and nystagmus are less common.143 The diagnosis is made by CT, which reveals a hypoor isodense extraaxial collection with enhancement. On MRI, diffusion is restricted,41 unlike tumors or hemorrhage. Treatment with drainage and antibiotics is usually successful.
Subdural Tumors
Isolated subdural tumors are exceedingly rare. Meningioma and other tumors of the dura may invade the subdural space. Subdural metastases from leukemia or solid tumors rarely occur in isolation. They can be differentiated from hematomas and infection on scans by their uniform contrast enhancement.

SUBARACHNOID POSTERIOR FOSSA LESIONS
Subarachnoid blood, infection, or tumor usually occurs in the posterior fossa in association with similar supratentorial lesions. Exceptions include subdural or parenchymal posterior fossa lesions that rupture into the subarachnoid space and posterior fossa subarachnoid hemorrhage.150
Posterior fossa subarachnoid hemorrhages are caused either by aneurysms or dissection of vertebral or basilar arteries or their branches. Unruptured aneurysms of the basilar and vertebral arteries sometimes grow to a size of several centimeters and act like posterior fossa extramedullary tumors. However, they generally do not cause coma unless they rupture. When a vertebrobasilar aneurysm ruptures, the event is characteristically abrupt and frequently is marked by the complaint of sudden weak legs, collapse, and coma. Most patients also have sudden occipital headache, but in contrast with anterior fossa aneurysms in which the history of coma, if present, is usually clear cut, it sometimes is difficult to be certain whether a patient with a ruptured posterior fossa aneurysm had briefly lost consciousness or merely collapsed because of paralysis of the lower extremities. Ruptured vertebrobasilar aneurysms are often reported as presenting few clinical signs that clearly localize the source of the subarachnoid bleeding to the posterior fossa. In Logue’s 12 patients,151 four had unilateral sixth nerve weakness (which can occur with any subarachnoid hemorrhage), one had bilateral sixth nerve weakness, and only two had other cranial nerve abnormalities to signify a posterior fossa localization. Duvoisin and Yahr152 reported that only about one-half of their patients with ruptured posterior fossa aneurysms had signs that suggested the origin of their bleeding. Jamieson reported 19 cases with even fewer localizing signs: five patients suffered third nerve weakness and two had sixth nerve palsies.153
Our own experience differs somewhat from the above. We have had eight patients with ruptured vertebrobasilar aneurysms confirmed at arteriography or autopsy, and six had pupillary, motor, or oculomotor signs indicating a posterior fossa lesion (Table 4–8).
The diagnosis is usually obvious on CT. Blood isolated to the fourth ventricle suggests
Specific Causes of Structural Coma |
145 |
Table 4–8 Localizing Signs in Six
Cases of Ruptured Vertebrobasilar
Aneurysms
Occipital headache |
5 |
Skew deviation of the eyes |
3 |
Third nerve paralysis |
2 |
Cerebellar signs |
3 |
Acute paraplegia before loss |
|
of consciousness |
2 |
|
|
a ruptured posterior inferior cerebellar artery aneurysm.150 Perimesencephalic hemorrhage is characterized by subarachnoid blood accumulating around the midbrain. While this often presents with a headache and loss of consciousness, it has a relatively benign prognosis.154 Unlike most subarachnoid hemorrhage, the bleeding is usually venous in origin155; cerebral angiograms are negative and bleeding rarely recurs.
INTRAPARENCHYMAL
POSTERIOR FOSSA MASS
LESIONS
Intraparenchymal mass lesions in the posterior fossa that cause coma usually are located in the cerebellum. In part this is because the cerebellum occupies a large portion of this compartment, but in part because the brainstem is so small that an expanding mass lesion often does more damage by tissue destruction than as a compressive lesion.
Cerebellar Hemorrhage
About 10% of intraparenchymal intracranial hemorrhages occur in the cerebellum. A cerebellar hemorrhage can cause coma and death by compressing the brainstem. Increasing numbers of reports in recent years indicate that if the diagnosis is made promptly, many patients can be treated successfully by evacuating the clot or removing an associated angioma.156,157 However, for those patients who are comatose, mortality is high despite prompt surgical intervention.156,158 Approximately three-quarters of patients with cerebellar hemorrhage have hypertension; most of the remaining ones have
