
Книги по МРТ КТ на английском языке / Thomas R., Connelly J., Burke C. - 100 cases in radiology - 2012
.pdfThis page intentionally left blank

CASE 82: A KNOWN CASE OF INFLAMMATORY BOWEL DISEASE
History
A barium follow-through study has been requested on a 22-year-old woman who has a history of Crohn’s disease. She presented 2 days earlier with abdominal pain localized to the left lower quadrant and occasional diarrhoea. She denies vomiting and is still passing flatus freely. Despite taking her Crohn’s medication regularly, she feels this is an acute flare-up of her disease and sought medical attention.
Examination
Examination reveals a patient who is comfortable at rest with normal observations. Her abdomen is generally soft on palpation but there is local guarding and tenderness in the left iliac fossa. Per rectal examination does not demonstrate rectal blood.
Investigations show an elevated white cell count (90 per cent neutrophils) with normal renal and liver function tests. Her C-reactive protein is 160 mg/L.
An abdominal radiograph did not demonstrate bowel obstruction and a barium followthrough study is requested to assess her bowel mucosa and look for fibrotic strictures (Figure 82.1).
Figure 82.1 Barium follow-though.
Questions
•How is this procedure performed and what does it demonstrate?
•What other imaging modalities are used to diagnose and follow-up patients with Crohn’s disease?
•What are the extra-intestinal manifestations of Crohn’s disease?
233
ANSWER 82
This is a single image of a barium follow-though study, acquired with the patient in a prone position and centred on the right lower quadrant. There is good opacification of the small bowel, and contrast appears to have passed freely into the large bowel with opacification of the descending colon. This image demonstrates a 25 cm stricture of the terminal ileum, with the adjacent caecal pole also appearing abnormal and oedematous. There is small bowel loop separation in the right lower quadrant, probably related to lymphoedema of the bowel wall and adjacent fibrofatty proliferation, however an inflammatory mass lesion (e.g. abscess) needs to be excluded. There is no prestenotic dilation and the appearance of the remaining small bowel is normal. The findings are in keeping with active inflammatory stricture related to Crohn’s disease, and a computed tomography (CT) abdomen and pelvis is recommended to exclude a drainable collection.
Local hospital policy dictates the exact procedural technique of a barium follow-through study: a patient is required to drink a set volume of radio-opaque barium, often diluted with water and mixed with a prokinetic agent (e.g. metoclopramide) to promote rapid transit through the bowel. The barium is screened though the small bowel under fluoroscopy, and sequential images are obtained at different points in time. The patient is often imaged in the prone position to splay the bowel loops and reduce composite shadowing from overlying loops of bowel. Focal compression can improve visualization as demonstrated in this image, with the compression paddle highlighting the area of tapered narrowing at the terminal ileum.
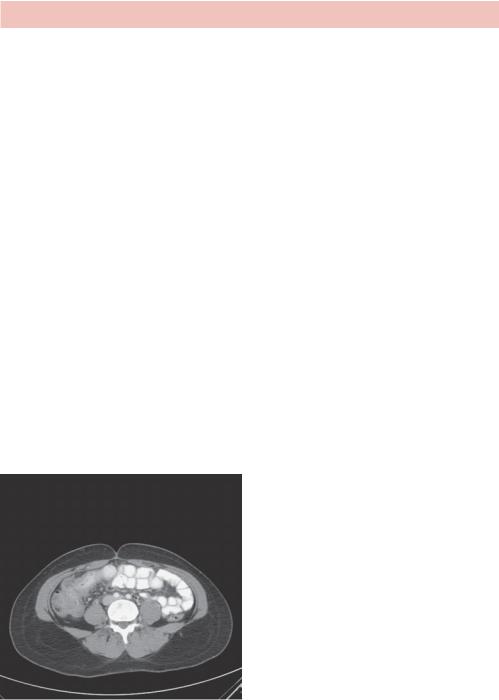
As well as small bowel follow-through studies, there is also a role for both CT and magnetic resonance imaging (MRI). A CT scan is quick to perform and usually accessible 24 hours per day, but it carries a significant radiation exposure and Crohn’s patients are often young. CT is employed in the acute setting to characterize the extent of acute inflammation and also to exclude abscess formation (Figure 82.2).
Figure 82.2 Axial CT scan.
A CT scan of the same patient, acquired at the level of the terminal ileum following intravenous and oral contrast administration was performed. It confirms an acute inflammatory reaction centred on the terminal ileum and caecal pole with bowel wall thickening, mucosal hyperenhancement and perinephric fat stranding with small volume pericolic lymph nodes seen. There is no evidence of an inflammatory mass lesion or drainable collection.
234
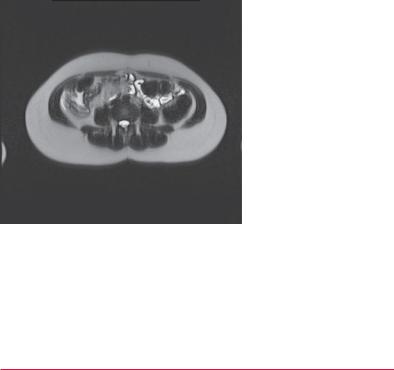
MRI is preferable for the long-term follow-up of Crohn’s disease patients, and has a high sensitivity for disease evaluation without exposing the patient to ionizing radiation. MRI has good soft tissue contrast and provides further information to differentiate between fibrosis and inflammation.1 This can dictate whether a patient continues medical treatment or requires surgery. However, MRI is expensive and time consuming to perform and does not provide accurate mucosal detail obtained in a follow-through study.
Figure 82.3 is a single image from an MRI half Fourier acquisition single shot turbo spin echo (HASTE) sequence of the same patient taken 6 months later, and demonstrates a fibrotic stricture of the terminal ileum measuring approximately 6 cm, with no evidence of active inflammation.
Figure 82.3 Axial MRI image from HASTE sequence.
Crohn’s disease is an inflammatory condition that can affect the bowel anywhere from the mouth to the anus. Gastrointestinal symptoms include diarrhoea, rectal bleeding, malabsorption and abdominal pain. Patients suffer from bowel strictures causing obstruction, adhesion formation and fistulation, often resulting in surgery. As well as an increased risk of malignancy, patients have a range of extraintestinal manifestations (Table 82.1).
Table 82.1 Extraintestinal manifestations of Crohn’s disease
Hepatobiliary |
Fatty liver |
|
Gallstone disease |
|
Pancreatitis |
Genitourinary |
Urolithiasis |
|
Renal amyloidosis |
Musculoskeletal |
Clubbing |
|
Hypertropthic osteoarthropathy |
|
Avascular necrosis |
Erythema nodosum |
|
Uveitis |
|
Growth retardation (childhood onset) |
|
|
|
235

KEY POINTS
•Fluoroscopy studies are still widely used in the diagnosis of Crohn’s disease but are being superseded by MRI and CT techniques.
•CT is often performed in the acute setting to exclude other pathology, with MRI more appropriate for long-term follow-up.
•Crohn’s disease is an inflammatory condition of the bowel with a wide range of extraintestinal manifestations.
References
1.Lawrance, I.C., Welman, C.J., Shipman, P. and Murray, K. (2009) Correlation of MRI-determined small bowel Crohn’s disease categories with medical response and surgical pathology. World Journal of Gastroenterology 15: 3367–75.
236

CASE 83: A TOURIST FROM NEW ZEALAND
History
A 44-year-old woman attends the accident and emergency department with a painful leg. She is a tourist on holiday, and flew in from New Zealand on a 23-hour flight arriving 2 days ago. Since landing in the UK, her left leg has developed an achy pain with associated swelling and erythema. It has become increasingly difficult to walk, and despite analgesia with elevation of the leg her symptoms have not resolved. She is alarmed by the swelling and attended hospital with near complete immobility due to the pain.
She is normally a fit and healthy individual with no significant medical history. Apart from occasional homeopathic remedies for insomnia, she is taking no regular prescribed medication other than the oral contraceptive pill.
Examination
On examination there is swelling of the left ankle, calf and thigh with marked tenderness in the calf muscles and some tenderness medially in the thigh. There is some redness of the leg. There is no knee joint effusion and peripheral pulses are present.
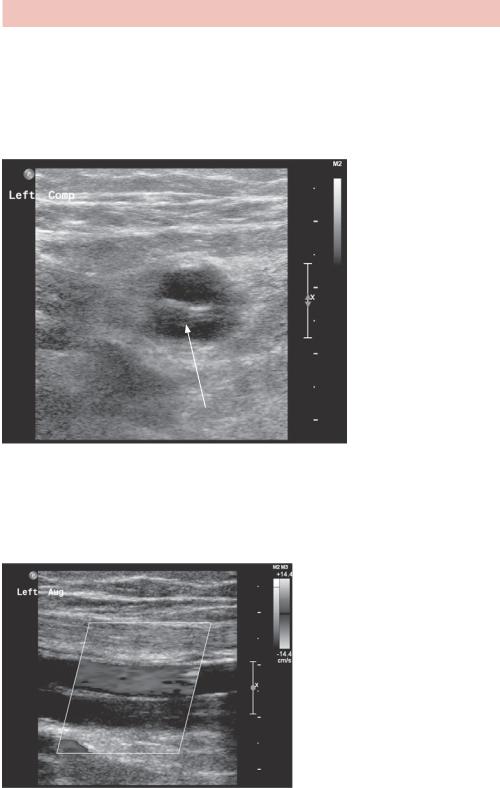
As part of her investigations, a lower limb ultrasound is organized with the radiology department (Figure 83.1).
Figure 83.1 Ultrasound.
Questions
•What does this ultrasound image demonstrate?
•How does ultrasound work?
•What are the strengths and limitations of ultrasound?
237
ANSWER 83
This static image is a cross-sectional view of the superficial femoral vein (SFV) lying adjacent to the superficial femoral artery (Figure 83.2). Fluid on ultrasound is normally hypoechoic in appearance as demonstrated by the flowing blood within the femoral artery. The intraluminal appearances of the adjacent vein are not anechoic, and return a heterogeneous echogenic signal. Subsequent images demonstrate non-compressibility of this SFV in keeping with a solid intraluminal venous component.
Echogenic thrombus within vessel
Figure 83.2 Ultrasound with echogenic thrombus indicated.
Figure 83.3 shows a longitudinal Doppler image of the same region with flow demonstrated within the femoral artery. The SFV again demonstrates an ill-defined heterogeneous echogenic appearance, and only a trace of flow is demonstrated.
Figure 83.3 Longitudinal Doppler image.
238
In summary, there is echogenic thrombus seen within the left SFV with reduced patency, compressibility and flow in keeping with a deep vein thrombosis (DVT). The possible complications are pulmonary embolism and post-phlebitic problems in the limb. Anticoagulation is indicated. The risk factors in this case are the long flight and the oral contraceptive pill. The oral contraceptive pill should be stopped, with appropriate contraceptive advice, and anticoagulation would normally be continued for 6 months with a first thrombus and an identified precipitant.
Ultrasound is the use of sound waves to image the human body. The sound waves are of such high frequency that they are inaudible to the human ear (e.g. 2–20 MHz). An ultrasound probe is designed to convert an electrical signal into acoustic energy and does so by utilizing the unique properties of piezoelectric crystals (most commonly microcrystalline lead zirconate titanate (PZT)). The ultrasound probe comprises a compressed layer of PZT, which is coated in silver to allow electrical conduction. Passing an alternating electrical current causes the PZT to expand and contract with the production of a sinusoidal sound wave of a particular frequency and wavelength. The shape of the ultrasound probe and a rubber-coated window can focus the sound wave, allowing an operator to control its direction.
The sound waves do not pass through the body freely, and tissues of differing density cause the beam to be reflected back towards the probe. The degree of sound wave transmission through a tissue before it is reflected is dictated by the acoustic impedance of the tissue through which it is passing. Subtle density changes (e.g. within soft tissue) cause the reflected ‘echoes’ to return to the probe at different times. The returning sinusoidal sound wave compresses the PZT, which converts the acoustic echo back into electrical energy and allows complex computer programs to form a picture on the operator’s screen. When there is a sudden density change (e.g. muscle to bone/muscle to gas) the majority of the sound wave is either transmitted or reflected and no images beyond this density interface can be generated. This limits the use of ultrasound in imaging the lungs or deep to bone.
Each probe has a fixed frequency, with a higher frequency returning more echoes over a period of time and forming an image of superior resolution compared to probes of a lower frequency. Unfortunately, the acoustic impedance of higher frequency and shorter wavelength sound waves, limits the depth they can travel. Higher frequencies are therefore recommended for the imaging of superficial pathology (e.g. a subcutaneous lump), while deeper imaging (e.g. abdomen) requires a probe of increased wavelength, and the reduced frequency allows only for an image of reduced resolution. As with many other aspects of radiology (e.g. CT dose versus noise), image resolution and depth penetration is a trade-off.
As an imaging modality that does not involve the use of ionizing radiation, ultrasound is preferred, if appropriate, to CT or X-ray. Some of the strengths and weaknesses of ultrasound are listed in Table 83.1.
239

Table 83.1 Strengths and weaknesses of ultrasound
Strengths
•No ionizing radiation: This is especially important in the young people and pregnant women
•Cheap: Compared to a CT or MRI scanner, ultrasound machines are inexpensive
•Readily available: No patient preparation or other healthcare professionals required
•Real time: Allows for functional imaging (e.g. contrast enhancement) and needle guidance for biopsy procedures
•Portable: Ultrasound machines can be taken to immobile patients (e.g. ITU)
Weaknesses
•Operator dependent: Experience may dictate a more accurate report
•Body habitus: It is more difficult to generate a diagnostic image in larger people
•Density changes: Images are limited by bone, bowel gas and normal aerated lung
KEY POINTS
•Ultrasound has a high sensitivity for the diagnosis of a DVT and carries no risk of ionizing radiation exposure to the patient.
•Ultrasound assesses compressibility, patency and flow of the deep venous system.
•The major limitations of ultrasound are operator dependence and patient body habitus.
240
CASE 84: SPONTANEOUS NOSE BLEEDS IN A YOUNG PERSON
History
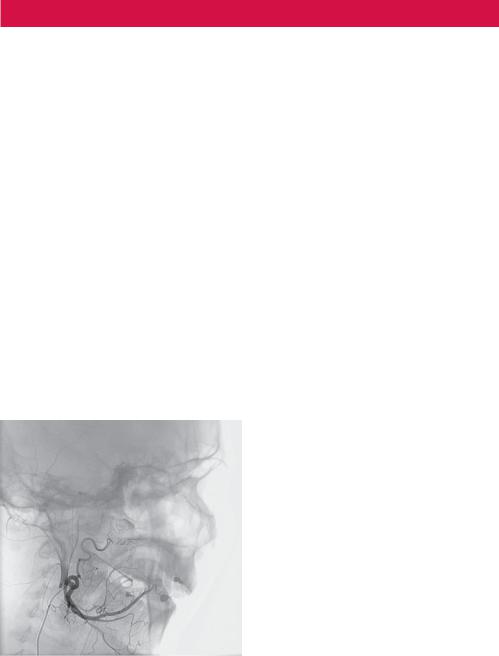
A 14-year-old boy is referred to the interventional radiology department following an ear, nose and throat (ENT) multidisciplinary meeting (MDM). He complains of a 6-week history of epistaxis that has been increasing in frequency, currently with approximately eight episodes of bleeding per day. No predisposing factors are to be found on history and the spontaneous bleeds can occur at any time. The worst bleeds are at night and he recently reports a single episode when he woke from sleep feeling as though he was choking from a spontaneous episode of bleeding. At that time the bleeding lasted more than 30 minutes and required hospital attendance for nasal packing. He has never needed a blood transfusion.
Examination
On review by the ENT registrar on call at the accident and emergency department, initial screening bloods were unremarkable but the patient was kept in hospital overnight for observation. The next morning the nasal packing was removed and direct visualization with a flexible nasendoscope revealed an area of friable soft tissue abnormality on the right side. The patient was referred for a contrast-enhanced computed tomography (CT) scan, which revealed an avidly arterially enhancing soft tissue mass in the post-nasal space with extension into the retroantral region. The pterygopalatine fossa was widened and a diagnosis of juvenile angiofibroma was made with supply from the right sphenopalatine artery. The patient was discussed at the ENT MDM and referred for embolization under the interventional radiologists (Figure 84.1).
Figure 84.1 Digital subtraction angiography.
Questions
•How was this procedure performed?
•How are catheters and sheaths sized?
•What embolization materials are available?
241
