
Книги по МРТ КТ на английском языке / Functional Neuroimaging in Child Psychiatry Ernst 1 ed 2000
.pdf
204 L. K. Jacobsen and A. Bertolino
Weinberger, D. R., Berman, K. F., Suddath, R. and Torrey E. F. (1992). Evidence of dysfunction of a prefrontal-limbic network in schizophrenia: a magnetic resonance imaging and regional cerebral blood Xow study of discordant monozygotic twins. Am. J. Psychiatry, 149, 890±7.
Weisel, F. A., Wik, G., Sjogren, I., Blomqvist, G., Greitz, T. and StoneElander, S. (1987). Regional brain glucose metabolism in drug free schizophrenic patients and clinical correlates. Acta Psychiatr. Scand., 76, 628±41.
Yakovlev, P. I. and Le Cours, A. R. (1964). The myelogenetic cycles of regional maturation of the brain. In Regional Development of the Brain in Early Life, ed. A. Minkowski. Boston: Blackwell ScientiWc.
Yeo, R. A., Hodde-Vargas, J., Hendren, R. L. et al. (1997). Brain abnormalities in schizophrenia-spectrum children: implications for a neurodevelopmental perspective. Psychiatry Res., 76, 1±13.
Yurgelun-Todd, D. A., Renshaw, P. F., Gruber, S. A.,Waternaux, C. M. and Cohen, B. M. (1996). Proton magnetic resonance spec-
troscopy of the temporal lobes in schizophrenics and normal controls. Schizophr. Res., 19, 55±9.
Zahn, T. P., Jacobsen, L. K., Gordon, C. T., McKenna, K., Frazier, J. A. and Rapoport, J. L. (1997). Autonomic nervous system markers of psychopathology in childhood onset schizophrenia. Arch. Gen. Psychiatry, 54, 904±12.
Zametkin, A. J., Nordahl, T. E., Gross, M. et al. (1990). Cerebral glucose metabolism in adults with hyperactivity of childhood onset. N. Engl. J. Med., 323, 1361±6.
Zametkin, A. J., Liebenauer, L. L. Fitzgerald, G. A. et al. (1993). Brain metabolism in teenagers with attention-deWcit hyperactivity disorder. Arch. Gen. Psychiatry, 50, 333±40.
Zipursky, R. B., Lim, K. O. and PfeVerbaum, A. (1991). Brain size in schizophrenia. Arch. Gen. Psychiatry, 48, 179±80.
Zipursky, R. B., Marsh, L., Lim, K. O. et al. (1994). Volumetric MRI assessment of temporal lobe structures in schizophrenia. Biol. Psychiatry, 35, 501±16.
12
Pediatric mood disorders and neuroimaging
Robert A. Kowatch, Pablo A. Davanzo and
Graham J. Emslie
Introduction
Until recently, mood disorders were thought to have their onsets in adulthood and to be rare in children and adolescents. This view failed to take into account the possibility that the clinical presentations of mood disorders might diVer with age. Research now has shown that mood disorders do occur in children and adolescents but present somewhat diVerently than in adults (Bowring and Kovacs, 1992; Birmaher et al., 1996). Recognition of this phenomenon has stimulated the use of neuroimaging techniques for research in these disorders; clinical applications have not been established.
This chapter will Wrst present the clinical characteristics of these disorders in children and adolescents, brieXy reviewing what is known about the neurobiology of these disorders; it will then present an overview of both adult and pediatric imaging studies of relevance to mood disorders.
Clinical aspects of mood disorders in children and adolescents
Child and adolescent mood disorders are complex in both their clinical presentations and neurobiology. These disorders commonly involve cognitive, aVective, vegetative, and perceptual systems. The underlying neurobiology appears to involve multiple neurotransmitter and neuroendocrine systems. The developmental course and presentation vary, depending upon the age of the patient and what other disorders are comorbid. Bipolar disorders are particularly complex because often their initial presentation is a severe, sometimes psychotic, depression that later evolves into episodes of mania or hypomania. One of the hallmarks of pediatric bipolar disorders is mood lability and marked irritability.
The development of mood and its disorders occurs at much younger ages than was previously thought. Research suggests that children develop internal mood states between the ages of 12 and 18 months (Cicchetti et al., 1997) and can discriminate facial expressions when they are as young as 4 months of age (LaBarbera et al., 1976). Whereas psychoanalytic theory once taught that children could not experience depression before adolescence (Rie, 1966), it is now well established that mood disorders occur in childhood (see Epidemiology below). Children with a mood disorder are most often referred to clinicians because of their behavior. The most common referral patterns are (i) a child who is irritable, oppositional and negative, refusing to do work in school and having severe emotional outbursts at home and school; (ii) a child with unexplained physical complaints, such as headaches and stomach aches, whose degree of disability is in excess of any clear medical cause; (iii) the hyperactive, impulsive, motor-driven child, tearing up the world around ± often with severe aggression, all along denying anything is wrong. None of these pictures Wt the lay person's perception of the mood of a depressed child, and yet the Wrst two are the typical presentations for depression and the third for bipolar disorder.
Epidemiology
Prevalence estimates of depressive disorders in children and adolescents range from 0.4 to 8.3% (Lewinsohn et al., 1986, 1993, 1994; Kashani et al., 1987a,b; Fleming and OVord, 1990; Burke et al., 1991; ShaVer et al., 1996) and are greater in adolescents than in children. These prevalence rates are only slightly lower than those for adults (Kessler et al., 1994), in whom the 12-month prevalence of major depressive disorder (MDD) is reported to be 10.3"0.8% with females showing higher rates than males (12.9"0.8% females and
205

206 R. A. Kowatch, P. A. Davanzo and G. J. Emslie
7.7"0.8% males). In contrast, MDD in children appears to occur at approximately the same rate in girls and boys. The approximately 2:1 (female:male) ratio seen in adults emerges during adolescence (Emslie et al., 1990).
Bipolar disorders are equally as prevalent in children and adolescents as they are in adults, with an estimated prevalence of 1% (Kashani et al., 1987a,b; Lewinsohn et al., 1995). Bipolar disorders are also the most prevalent psychotic disorders in all age groups, including children and adolescents (Faedda et al., 1995). Wozniak et al. (1995) recently reported that of 262 children consecutively referred to a pediatric psychopharmacology clinic, 16% met DSM-III-R criteria for mania (American Psychological Association, 1989).
Signs and symptoms
Although the diagnostic criteria for MDD in children and adolescents are the same as those for adults, diVerences in symptomatic expression are substantial. Children tend to be more reactive to their environment and, therefore, may not consistently appear sad. Rather, their mood disturbance is most often expressed in variable days, consisting of normal moods and behavior interspersed with frequent periods of depressed feelings and irritability. Irritability is common in this age group, with irritable moods frequently resulting from sad feelings. Changes in social behavior may be manifested in adolescents by joining less socially desirable peer groups. Frequent complaints of boredom indicate loss of interest. School phobic reactions (fear of going to school) can also be symptomatic of depression. School refusal may constitute the primary problem for referral. With changes in appetite, children often become ªpickyº eaters, craving sweets or snack foods, and, in some instances, become voracious overeaters. Absence of usual weight gain, rather than weight loss, is common in the depressed child. Excessive weight gain is seen in some children and adolescents, but adolescents frequently lose weight. Depressed children often experience initial insomnia, not always objectively conWrmed. Middle insomnia is not uncommon in small children (getting in bed with parents and siblings). Terminal insomnia is less common than in depressed adults. Psychomotor symptoms result in agitation and oppositional behavior, which often lead to a misdiagnosis of oppositional deWant disorder. Alternatively, some depressed children and adolescents complain of feeling slowed down, both in physical movement and thinking. Children with depression often present to pediatricians or general practitioners with vague somatic complaints including headaches, stomach aches, or other physical symptoms for which the physician can Wnd no cause.
As with depression, while the DSM-IV criteria for bipolar disorders are the same for adults and children, there are developmental diVerences in symptom expression. For both children and adults, the essential feature of a bipolar I disorder is a clinical course characterized by one or more manic or mixed episodes. A child or adolescent who has had one or more episodes of major depression and at least one episode of hypomania, but no episodes of mania, is classiWed in DSM-IV as having a bipolar II disorder. Cyclothymia is a disorder of at least 1 year duration in which there are numerous periods of both hypomanic and depressive symptoms that do not meet criteria for mania or major depression. These symptoms may Xuctuate within days, weeks, or months. The child or adolescent is not without symptoms for more than 2 months at a time.
Comorbidity
The diagnosis of a mood disorder is often obscured by the presence of other comorbid psychiatric diagnoses, as well as by general medical disorders. The most common comorbid diagnoses among bipolar adolescents are anxiety disorders, attention-deWcit hyperactivity disorder (ADHD), conduct disorders, and substance abuse (Lewinsohn et al., 1995).
Natural course
The developmental course of mood disorders suggests a continuum of pathology from childhood to adulthood. Such developmental progression can be captured and utilized in brain imaging studies to further our understanding of the neural substrates of mood disorders. Similar to adults with depressive illness, depressed children and adolescents have a high rate of recurrence of their depression. Recurrence (i.e., a new episode of depression) has been reported in 54±72% of depressed children and adolescents followed for 3±8 years, with similar rates seen in inpatients (Garber et al., 1988; Emslie et al., 1997) and outpatients (Kovacs et al., 1984; McCauley et al., 1993; Rao et al., 1995).
Furthermore, early-onset depression often continues into adulthood. Kandal and Davies (1986) described poor adult outcomes in a large sample of adolescents (1004) identiWed as having depressive symptoms using a selfreport scale. Similarly, in a retrospective, long-term followup study of 80 depressed and 80 nondepressed outpatient adolescents, Harrington et al. (1990) reported that depressed adolescents were more likely than nondepressed adolescents to have depression in adulthood; however, they note that most adult depressions are not preceded by adolescent depression.

Pediatric mood disorders and neuroimaging |
207 |
|
|
The natural history of bipolar disorder in children and adolescents has received little study. McGlashen (1988) interviewed 62 adult patients who met DSM-III criteria for mania and divided them into two groups: 33 with adolescent onset of mania and 29 with adult onset of mania. He reported that among the adolescent-onset group, the mean age at which they Wrst became symptomatic was 16 years. In comparing the course of the disorder, the adoles- cent-onset group had more hospitalizations, displayed more psychotic symptoms, and were more frequently misdiagnosed as having a schizoaVective disorder than the adult-onset group. Surprisingly, the adolescent-onset group had outcomes superior to those of the adult-onset group in terms of social relationships and their ability to work.
Strober et al. (1993) followed 58 adolescents who had been admitted to a psychiatric unit for a major depressive episode and found that during the 24-month follow-up period, mania occurred only in those patients who had a psychotic depression. In this psychotically depressed group, 28% went on to develop bipolar I disorder. In a similar follow-up study of depressed prepubertal children, Geller et al. (1994) reported that bipolarity was predicted by a family history of major mood disorders, major depressive disorder, or schizoaVective disorder. These studies show that bipolar disorders may Wrst occur in childhood or adolescence, may sometimes present with schizophreniclike symptoms, may be predicted by a past history of psychotic depression, and are associated with a family history of major mood disorders.
The neurobiology of mood disorders
Most neurotransmitter systems have been proposed as playing a role in mood disorders (Rush et al., 1998). Evidence from neuroanatomic, neurophysiologic, neurochemical, and behavioral studies in humans and animals also support the view that mood disorders are mediated by networks of interacting neural regions that are often widely spatially distributed (Mesulam, 1990; Sackeim et al., 1990; Soares and Mann, 1997b).
Neurotransmitter studies
Peripheral studies of neurotransmitters have primarily focused on norepinephrine, serotonin, and acetylcholine (Willner, 1985; Coyle, 1987; Gold et al., 1988; Zubenko et al., 1990). The interest in the bioamine hypothesis for depression originally arose from observations of depression caused by reserpine. Reserpine is an antihypertensive
which depletes noradrenaline, dopamine, and serotonin and which can cause a depression, suggesting that depression, in part, results from a decrease in the availability of the mode of action of known antidepressant drugs, such as the speciWc serotonin-reuptake inhibitors, which increase serotonergic activity.
Although noradrenaline (norepinephrine) has been the most studied neurotransmitter in depression (Bunney and Davis, 1965; Schatzberg et al., 1982; Golden and Potter, 1986), results have been disappointing. Cerebrospinal Xuid (CSF) concentrations of noradrenaline metabolite 3- methoxy-4-hydroxyphenylglycol have not clearly diVered in adult patients with depression from those in controls, although Maas et al. (1968) reported decreased urinary excretion of the metabolite in bipolar patients in the depressed phase. Studies of children and adolescents are limited, although De Villiers et al. (1989) found no diVerence in noradrenergic function between depressed adolescents and controls.
Similarly, peripheral studies of serotonin (5-hydroxy- tryptamine) in adults with depression have not been helpful (Prange et al., 1974; van Pragg, 1977; Agren, 1980; Glennon, 1987), except for a subgroup of depressed patients. This subgroup, characterized by aggression, anxiety, impulsivity, and suicidality, showed low CSF 5- hydroxyindoleacetic acid, a product of serotonin metabolism. In children and adolescents, Ryan et al. (1992) reported abnormal neuroendocrine response to l-5- hydroxytryptophan in 37 prepubertal depressed children compared with 23 normal controls, suggesting a dysregulation of central serotonergic systems in childhood depression.
A theoretical framework characterizing the neurotransmitter systems involved in child and adolescent depression has been proposed by Rogeness et al. (1992), who adapted the model of Gray et al. (1981) for the neurobiology of anxiety disorders. Posited is an imbalance between a behavioral facilitory system (BFS) and a behavioral inhibitory system (BIS). The BFS is thought to be a primarily dopaminergic system, whereas the BIS is thought to involve noradrenergic and serotonergic systems. Rogeness et al. (1992) proposed that in child and adolescent major depression dopaminergic function (BFS) is depressed and noradrenergic and serotonergic (BIS) functions are elevated (Rogeness et al., 1992).
Neuroendocrine studies
Evidence implicating dysfunction of the hypothalamic± pituitary±adrenal axis, the hypothalamic±pituitary±thyroid axis, and the hypothalamic±pituitary±growth hormone axis

208R. A. Kowatch, P. A. Davanzo and G. J. Emslie
has been reported in depression in adults. The neuroregulatory control of these axes involves many neurotransmitters including noradrenaline, acetylcholine, serotonin, and gamma-aminobutyric acid (GABA). Cortisol hypersecretion, present in adult depression, has not been identiWed in depressed children and adolescents (Puig-Antich et al., 1989; Kutcher et al., 1991), although depressed adolescents have shown a cortisol elevation at the approximate time of sleep onset (Dahl et al., 1989). However, nonsuppression of cortisol by dexamethasone has been found in many studies of depressed children and adolescents (Extein et al., 1982; Poznanski et al., 1982; Robbins et al., 1982; Doherty et al., 1986; Emslie et al., 1987). Inconsistent Wndings between studies may reXect diVerences in sampling, dosages, and the pharmacokinetics of dexamethasone (McCracken et al., 1988; Naylor et al., 1990).
Growth hormone releasing factor release is stimulated by noradrenergic, dopaminergic, and serotonergic neuronal input (Mendelson et al., 1978). Blunting of growth hormone release in response to hypoglycemia, desipramine, clonidine, and growth hormone releasing factor in depressed children and adolescents has been reported (Ryan et al., 1994). While these are among the most replicated results in this age group, the regulation of growth hormone by many neurotransmitters complicates their interpretation. Studies of thyroid axis abnormalities in children and adolescents are few. Kutcher et al. (1991) reported that nocturnal thyroid stimulating hormone values at 1.00 a.m. were elevated in 12 depressed adolescents, relative to normal controls, but there was no signiWcant diVerence in the total amount secreted throughout the night.
Whereas several neurobiologic Wndings, like cortisol hypersecretion and reduced REM (rapid eye movement) latency, are present in mood disorders in adults, studies of pediatric patients are only suggestive of similar Wndings. Further research is needed to determine how these neurobiologic factors are involved in pediatric mood disorders. Functional neuroimaging studies are likely to be informative in this respect.
Neuroimaging studies
Most neuroimaging studies have been conducted in adults. Findings from these studies need to be compared with those in children to understand the developmental trajectory of neural abnormalities and their signiWcance. This section will cover neuroimaging studies in adults, including activation studies using neurobehavioral probes, and the few imaging studies performed in children and adolescents.
Single-state studies of adults with mood disorders
Since 1972, more than 100 functional imaging studies using positron emission tomography (PET), single photon emission computed tomography (SPECT), or magnetic resonance spectroscopy (MRS) to study mood disorders in adults have been published. Most of these studies were completed with subjects scanned in a resting state. The results have been variable, likely because of diVerences in factors such as subject selection, diagnostic procedures, severity of illness, medication status, demographic characteristics, imaging techniques and analytic methods, and inadequate control over or variations in the state in which subjects were scanned. A thorough review of these studies is beyond the scope of this chapter, and the interested reader is referred to recent reviews by Drevets (1998), Mayberg (1997), and Soares and Mann (1997b).
The most replicated Wndings in well-designed PET and SPECT studies of cerebral blood Xow and metabolism in depression, not confounded by medication eVects (Drevets, 1998; Mayberg et al., 1994; Soares and Mann, 1997b), include (i) reductions in dorsolateral and dorsomedial prefrontal blood Xow and glucose metabolism, with some, but not all, studies indicating that these abnormalities are reversed by antidepressant therapy; (ii) reduction in blood Xow and glucose metabolism in the anterior cingulate gyrus in both unipolar and bipolar depression, which does not normalize following treatment, possibly because anatomic volumetric reductions may account, at least in part, for the apparent functional Wnding; (iii) increased blood Xow and metabolism in the amygdala (left and possibly right) and medial thalamus in both unipolar and bipolar depression; and (iv) reduced blood Xow and metabolism in the caudate in unipolar, but not bipolar, depression.
Abnormalities in the prefrontal cortex may be linked to neuropsychologic impairments in depression, and those in the anterior cingulate may reXect emotional processing and/or obsessive ruminations (Drevets, 1998). Drevets (1998) has highlighted the amygdala as the only structure in which blood Xow and metabolism consistently show positive correlations with the severity of depression. Abnormal elevations of amygdala activity may be seen during sleep and in asymptomatic (remitted) subjects with familial depression who are not receiving treatment. Antidepressants that ameliorate symptoms and help to prevent relapse normalize amygdalar activity. Baseline amygdalar activity may predict relapse induced by a tryp- tophan-free diet (thought to deplete brain serotonin) in successfully treated, remitted patients, suggesting that it confers susceptibility to depression. Finally, resting-state
Pediatric mood disorders and neuroimaging |
209 |
|
|
amygdalar hypermetabolism at present appears to be unique to mood disorders.
Less consistent Wndings include reductions of blood Xow and metabolism in the lateral temporal and parietal cortex, which may relate to neuropsychologic impairments associated with depression (Drevets, 1998; Soares and Mann, 1997b). Finally, increased blood Xow has been reported in the cerebellar vermis in major depression, a Wnding that aVects the interpretation of many SPECT studies which have normalized regional cerebral blood Xow (rCBF) using the cerebellum as a reference (Drevets, 1998).
Alterations in blood Xow and metabolism primarily reXect changes in synaptic activity (see Chapter 1). Regional brain diVerences may arise from increases or decreases in excitatory or inhibitory projections either within or distal to the region in which they are measured. The regions identiWed as abnormal by imaging studies agree with lesion studies in implicating neural circuits involving the frontal and temporal lobes and portions of the striatum, pallidum, and thalamus in the pathophysiology of depression (Drevets, 1998). Secondary depression, such as that seen in basal ganglia disorders (e.g., Huntington's or Parkinson's disease) or in other neuropsychiatric syndromes (e.g., obsessive-compulsive disorder), is likely to involve dysfunctional interactions between strucures within these same circuits, although the speciWc characteristics of these interactions are likely to diVer.
Among the studies with the best control groups are two blood Xow studies of adults with MDD. The Wrst one used a two-dimensional probe 133Xe method to study the resting rCBF patterns of a group of 41 depressed adults and 40 ageand gender-matched controls (Sackeim et al., 1990). This study, which carefully controlled for diagnosis, age, gender, handedness, and medication status, found that depressed subjects had both reduced global CBF and an abnormal topographic distribution of blood Xow, with bilateral relative decreases in frontal, central, superior temporal, and anterior parietal regions compared with controls. These investigators postulated that blood Xow decreases in these areas reXected dysfunction in a parallel distributed cortical network involving frontal and temporoparietal polymodal association areas. These polymodal association areas are thought to be directly involved in mood changes in depressed patients (Tucker, 1988).
The other study (Drevets et al., 1992) used PET to study rCBF in a homogenous sample of patients who met criteria for familial pure depressive disease (i.e., these subjects had primary MDD, as did a Wrst-degree relative). Because neuroimaging changes may represent trait markers of the illness (Schlaepfer et al., 1997), state-dependent abnor-
malities (Bench et al., 1995), or a combination of the two (Drevets, 1998), two patients groups ± one symptomatic and one remitted ± were compared with normal controls (10 per group). Symptomatic MDD subjects showed increased relative rCBF in the left prefrontal cortex, left amygdala, and left medial thalamus and decreased relative rCBF in the caudate bilaterally compared with normal controls. Remitted subjects also showed increased amygdalar activity, implicating this as a trait-related marker of depression. Remitted patients failed to show the increased left prefrontal rCBF seen in symptomatic subjects, suggesting that this Wnding is state related.
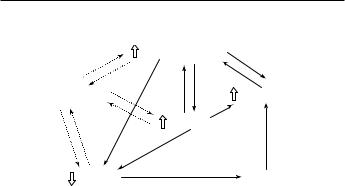
Drevets and Raichle (1992) postulate that two separate, but interconnected anatomic circuits are involved in adult MDD. One circuit involves the amygdala, the mediodorsal nucleus of the thalamus, and the ventrolateral and medial prefrontal cortex. This limbic±thalamo±cortical circuit, thought to act as an excitatory triangular circuit, is hypothesized to be overactive in symptomatic depression, as reXected in the increased rCBF in these areas. A second circuit, the limbic±striatal±pallidal±thalamic circuit, involves the striatum and the ventral pallidum and is connected to the Wrst as a disinhibitory sideloop. Drevets and Raichle (1992) felt that their rCBF PET Wndings in this group of depressed and remitted subjects was compatible with a neural model of depression proposed by Swerdlow and Koob (1987), which hypothesized that underactivation of forebrain dopamine systems with a resultant enhancement of limbic±thalamo±cortical positive feedback leads to symptoms of MDD (Fig. 12.1).
Neuroreceptor imaging studies, reviewed by Soares and Mann (1997b), have provided evidence of alterations in the serotonergic system (e.g., a blunted metabolic response to serotonin release) in depressed patients, as well as possible alterations in the dopaminergic system (e.g., increased D2 receptor binding and receptor density in the basal ganglia) of unipolar and bipolar patients.
Metabolic studies using 31P and 1H MRS, reviewed by Kato et al. (1998), suggest several abnormalities, including decreased phosphomonoester and phosphodiester levels in the frontal lobes and decreased phosphomonoesters in the temporal lobes, in patients with bipolar disorder in the euthymic state (Kato et al., 1998). The 31P MRS studies have reported signiWcant membrane phospholipid and energy metabolism abnormalities in the frontal and temporal lobes of adult bipolar patients (Kato et al., 1992, 1993; Deicken et al., 1995a,b; Moore et al., 1997). Several 1H MRS studies reported signiWcant choline abnormalities in the parietal lobes and basal ganglia of adult bipolar patients (Sharma et al., 1992; Stoll et al., 1992; Renshaw et al., 1997).
210 R. A. Kowatch, P. A. Davanzo and G. J. Emslie
±Prefrontal cortex
|
|
|
+ |
+ |
|
+ |
|
|
|
|
|
|
|
|
+ |
|
|
|
|
Mediodorsal thalamus |
A9 and A10 |
±? |
|
|
|
||
+? |
|
|
± |
|||
± |
+? |
|
+ |
|||
|
Amygdala |
|
|
|||
|
|
|
|
|
|
|
± |
+ + |
|
|
|
± |
|
Striatum |
|
|
|
|||
|
|
|
|
Pallidum |
||
Fig. 12.1. Neuroanatomic circuits hypothesized to participate in the functional anatomy of unipolar major depression. Regions showing blood Xow diVerences have adjacent open arrows, which indicate the direction of differences in Xow in the depressives relative to controls. The regions' monosynaptic connections with each other are illustrated (solid arrows) with 1 indicating excitatory and 2 inhibitory projections, and with ? indicating where experimental evidence is limited. The portions of the prefrontal cortex affected involve primarily the ventrolateral and medial prefrontal cortex. The parts of the striatum under consideration are the ventromedial caudate and nucleus accumbens, which particularly project to the ventral pallidum. The major dopaminergic projections from the substantia nigra (A9) and the ventral tegmental area (A10) to these structures are illustrated with the dotted lines. (Reprinted with permission from Drevets et al. (1992). Journal of Neuroscience, 12, 3637.)
Structural neuroimaging studies of adults with mood disorders
The possibility exists that at least some trait-related abnormalities seen in mood disorders with functional neuroimaging may be attributable to anatomic deviations (Drevets, 1998). Structural imaging studies of adults with major depressive disorder and bipolar disorder have reported a variety of neuroanatomic abnormalities, the most consistent of which include an increased rate of subcortical white matter hyperintensities, increased ventricular size, decreased temporal lobe volume, decreased frontal lobe volume and changes in basal ganglia structures (Soares and Mann, 1997a). Recently, Drevets et al. (1997) have shown structural abnormalities in the subgenual prefrontal cortex of patients with both unipolar and bipolar disorder compared with normal controls. The subgenual prefrontal cortex consists of agranular cortex on the anterior cingulate gyrus ventral to the genu of the corpus callosum (corresponding to Brodmann areas 24 and 32). This area has extensive connections with the amygdala, hypothalamus, and brainstem monoaminergic nuclei (i.e., locus ceruleus, raphe). These structures have been associated with the regulation of emotion, autonomic function, sleep, appetite, and monoamine transmission. It has been postulated that a disruption of this neuronal pathway may
produce a disturbance in any or all of the functions associated with mood disorders (Drevets et al., 1997).
In bipolar disorder, many of the adult studies that acquired T2-weighted magnetic resonance imaging (MRI) images have also reported Wnding white matter signal hyperintensities in the periventricular space of patients with bipolar I disease (Altshuler et al., 1995). These white matter signal hyperintensities could represent areas of astrogliosis, demyelination, encephalomalacia, or loss of axons (Bradley et al., 1984).
Neurobehavioral probes: recognition of facial expressions
The use of neurobehavioral probes in conjunction with functional imaging techniques may increase sensitivity and speciWcity in identifying the neural correlates of mood disorders. However, this involves a number of design challenges to insure valid experimental results (see Chapter 9). Sound task development may be conceptualized as involving the following stages (Gur et al., 1992): (i) selection of a unitary behavioral dimension for measurement; (ii) selection of tasks that tap into the chosen behavioral dimension and that have been validated within the constraints of experimental imaging paradigms; (iii) application of the chosen task with normal subjects to determine which brain areas are involved in the processing required by the neurobehavioral probe; and (iv) application of the neurobehavioral probe to well-characterized neuropsychiatric samples and matched normal control subjects.
Because impairments of social functioning in depressed adults have been hypothesized to stem, at least in part, from an inability to recognize facial expressions of emotion accurately (Persad and Polivy, 1993), several paradigms involving judgments of facial aVect perception have been developed and implemented to investigate the functional neuroanatomy of depression. One such paradigm, the Ekman facial recognition paradigm, requires subjects to discriminate and name the emotions of 14 photographed facial expressions depicting seven primary human emotions: fear, anger, surprise, contempt or disgust, happiness, sadness, and indiVerence (Ekman and Oster, 1979). The Ekman photographs have been used in a variety of experiments to study the mechanisms of facial recognition and mood in brain-damaged, normal, and depressed subjects.
In 1994, Adolphs et al. studied S.M., a 30-year-old woman with Urbach±Wiethe disease using the Ekman facial recognition paradigm. Urbach±Wiethe disease is a rare, autosomal recessive condition that causes nearly complete bilateral destruction of the amygdala and in which aVected individuals often show defective personal
Pediatric mood disorders and neuroimaging |
211 |
|
|
and social decision making (Hofer, 1973; Hofer et al., 1974). A T1-weighted MRI of S.M.'s brain demonstrated extensive bilateral amygdala damage with sparing of the neocortex and hippocampus. When S.M. was tested with the Ekman facial recognition paradigm, her mood was rated as normal and she had normal visual±perceptual skills. Although S.M. was able to recognize familiar faces, she was unable to recognize the emotion of fear in any of the Ekman photographs. She was also unable to recognize similarities between expressions of diVerent facial emotions. From these results, the authors concluded that the amygdala is necessary in humans both to recognize the emotion of fear and to recognize blends of multiple facial emotions.
These same authors expanded this study to three patients with damage to the left amygdala, three patients with damage to the right amygdala, 12 controls with brain damage but intact amygdalae, and seven normal subjects (Adolphs et al., 1995). In this experiment, which again used the Ekman facial recognition paradigm, subjects were asked to identify familiar faces, to draw pictures of facial expressions from memory, and to sort labels of emotions (e.g., happy, surprised, afraid) on the basis of the similarity and intensity of the emotion they denoted. Only bilateral, and not unilateral, damage to the amygdala impaired the processing of fearful facial emotions, while leaving the recognition of facial identity intact.
The Ekman facial photographs have proven less than ideal for neuroimaging studies because these photographs are asymmetrical, lit in varied ways, and contain both clothing and hair cues, thus introducing a number of potential confounds into studies of facial perception. To better control for such variables, the neuropsychiatry group at the University of Pennsylvania led by Ruben Gur and Roland Erwin created a more controlled set of facial photographs of professional actors and actresses portraying three emotions: happy, sad, or neutral (the PENN facial photographs). These photographs of faces are symmetrical, lighted in a standard way, and devoid of clothing or hair cues. In their Wrst behavioral study using these photographs, Erwin et al. (1992) tested a group of young normal adults and reported a gender diVerence in the discrimination of facial emotions, with males being less sensitive than females to sad emotions in female faces, and females being more sensitive than males to all emotional expressions in male faces. Therefore, it appears that another factor ± gender ± also aVects how facial emotions are perceived. Self-report mood ratings performed by the subjects during an emotion-discrimination task found that this task did not induce any changes in self-rated mood states.
Several behavioral studies have found that depressed adult subjects have diYculty recognizing facial emotional
cues (Feinberg et al., 1986; Sweeney et al., 1989; Gaebel and Wolwer, 1992; Rubinow and Post, 1992). Various explanations have been oVered for this deWcit, including perceptual inaccuracies (Mandal and Bhattacharya, 1985) and slow processing of facial emotional cues (Cooley and Nowicki, 1989), but the source of this deWcit is not yet fully understood. An alternative hypothesis proposed by Persad and Polivy (1993) was that the type of behavioral and emotional responses that facial cues elicit in depressed individuals lay at the core of their interactional diYculties.
Using a modiWed Ekman facial recognition paradigm, these investigators asked subjects to identify the emotion depicted in the Ekman photographs, identify what their behavioral response would be, explain their emotional reaction to the cue, and rate their degree of comfort with the cue (Persad and Polivy, 1993). Four groups of subjects were examined: 16 depressed college students enrolled in an introductory psychology course, 16 depressed psychiatric inpatients who met DSM-III criteria for major depression, 16 nondepressed college students also enrolled in an introductory psychology course, and 11 nondepressed psychiatric inpatients (two with anorexia, three with personality disorders, two with anxiety disorders, one with a pain disorder, and one with post-traumatic stress disorder). The depressed college student sample had a mean Beck Depression Inventory Score of 16, indicating mild depression, and the depressed inpatients a mean score of 37, indicating severe depression. Both depressed groups made more errors in facial recognition than did normal controls and nondepressed psychiatric inpatients, but neither of the depressed groups performed more poorly on any particular expression. Compared with the control groups, both depressed groups also reported more ªfreezing responsesº (tensing up) toward the facial expressions, higher levels of fear ratings, and less comfort with their emotional reactions to the expressions of fear, anger, disgust, sadness, and indiVerence. Persad and Polivy concluded that depressed individuals have a generalized, nonspeciWc deWcit in their perception of emotional cues, which includes problems at the level of facial recognition, behavioral reactions, and their own emotional reactions. Limitations of Persad and Polivy's study include their reliance on self-reports, the ecological validity (i.e., the relationship of responses to the Ekman paradigm versus real-life situations) of which is unknown. Nonetheless, these results suggest that the Ekman facial recognition paradigm not only involves the perceptual system but also stimulates behavioral and emotional responses that are aVected in depression.
Gur et al. (1992) reported that depressed patients misinterpret neutral faces as sad and happy faces as neutral

212R. A. Kowatch, P. A. Davanzo and G. J. Emslie
and that patients with more negative aVect, as measured on the Positive and Negative AVect Scale, show less ability to discriminate neutral versus sad faces. This Wnding is in general agreement with the cognitive theory of depression by Beck (1971), which holds that cognitive dysfunctions are at the core of depressive illness. The data of Gur et al. suggest that not only is cognition impaired in depressive illness but also impaired are the perceptual processes involved in the discrimination of facial emotions.
Activation studies of facial recognition in normal adults and adolescents
The Ekman facial recognition paradigm described above and variations of it have been used in the study of emotion in functional imaging studies. Table 12.1 summarizes the various functional imaging studies that have used such neurobehavioral probes. This table reXects an evolution of the imaging modalities used and the types of neurobehavioral paradigm employed. The earliest studies used facial recognition tasks with PET or SPECT, while the later studies used paradigms involving Wlm clips and autobiographical scripts with fMRI (discussed in a later section).
In an early 15O PET study, Sergent et al. (1992) measured rCBF in seven normal adults, aged 22±31 years, during facial discrimination. Subjects were scanned during three visual tasks: discrimination of the gender of faces, identiWcation of the faces of famous persons, and recognition of common objects. The gender discrimination task elicited activation (increased rCBF when subtracted from a grating control condition) in the right extrastriate cortex, while the face identiWcation task additionally elicited activation of the fusiform gyrus and anterior temporal cortex of both hemispheres and the right parahippocampal gyrus. The object-recognition task increased rCBF in the left occipitotemporal cortex but failed to aVect the right hemisphere regions activated during facial identiWcation. In general, several cortical areas were involved in the processing of faces, but it appeared that the ventromedial region of the right anterior temporal lobe was uniquely activated during facial identiWcation.
Using fMRI in conjunction with Ekman facial photographs, Breiter et al. (1996) measured activity in the amygdala of 18 normal men (mean age 26.5 years). In separate experiments, photographs of fearful versus neutral faces and happy versus neutral faces were presented. The amygdala was preferentially activated in response to fearful versus neutral faces, as well as in response to happy versus neutral faces, suggesting a possible generalized response to emotionally valenced stimuli. The fMRI measurements also indicated a rapid habituation of this neural response
in the healthy subjects. Similarly, using fMRI, Schneider et al. (1997) measured a signiWcant increase in signal intensity in response to sad, as well as happy, facial expressions in the left amygdala in 12 right-handed normal subjects (seven males, Wve females) using the PENN facial photographs.
Finally, in a recent fMRI study of adolescents, Baird and colleagues (1999) studied 12 normal adolescents, ages 12±17 years (mean 13.9 years) using a facial discrimination paradigm that required the labeling of the emotional expressions of six diVerent faces, all with fearful expressions. A signiWcant increase in signal intensity in both amygdalae was seen in response to fearful facial expressions compared with the control task of viewing nonsense gray-scale images.
Neuroimaging using mood induction paradigms with normal adults
A number of functional imaging studies have used a variety of mood induction paradigms (see Table 12.1). Pardo et al. (1993) measured rCBF using 15O PET in seven normal adult subjects (mean age of 24 years) scanned at rest and while they recalled or imagined a sad situation. Females activated areas in bilateral inferior and orbitofrontal cortex, while males activated the left and orbitofrontal cortex.
Similarly, George et al. (1995) used 15O PET to study 11 normal female subjects (mean age 33 years) while they recalled speciWc happy, sad, or neutral life events. Compared to the resting condition in which subjects were told to close their eyes and concentrate on their sensory and emotional experience, transient sadness signiWcantly increased rCBF bilaterally in the regions of the cingulate gyrus, right medial frontal gyrus, left dorsolateral prefrontal cortex, bilateral caudate, bilateral putamen, bilateral thalamus, bilateral fornix, left insula, and left midline cerebellum. In contrast, transient happiness resulted in no areas of signiWcantly increased activity but rather was associated with signiWcant and widespread reductions in cortical rCBF, especially in the right prefrontal and bilateral temporoparietal regions.
Using a cognitive task with 15O PET to elicit aVect, Schneider et al. (1996) imaged 12 normal subjects while they attempted to solve anagrams, some of which were designed to be unsolvable to induce learned helplessness, sadness, and anxiety. Compared with rest, both solvable and unsolvable anagram tasks increased activity in frontal and temporal regions. Dissociations seen in limbic structures suggested their involvement in the aVective aspects of these tasks. The solvable task condition increased hippocampal rCBF and decreased

Table 12.1. Functional imaging studies and neurobehavioral probes
|
|
Age (mean" |
Imaging modality |
|
|
|
|
|
SD or range, |
spatial resolution; |
|
|
|
Study |
Subjects (No.) |
years) |
acquisition parameters |
Probes |
Control task |
Results |
|
|
|
|
|
|
|
Sergent |
Normal males (7) |
22±31 |
PET H 15O; 5±6mm |
Facial gender |
Visual Wxation |
Face gender task: activation in the right |
|
|
|
2 |
|
|
|
et al. (1992) |
|
|
|
categorization |
|
extrastriate cortex |
|
|
|
|
Facial identity |
Passive viewing of face |
Face identity: activation of the fusiform gyrus |
|
|
|
|
|
|
and anterior temporal cortex of both |
|
|
|
|
|
|
hemispheres and the right parahippocampal |
|
|
|
|
|
|
gyrus |
|
|
|
|
Object recognition |
Sine-wave gratings |
Object recognition: increased rCBF in the left |
|
|
|
|
|
|
occipitotemporal cortex |
Pardo et al. |
Normal males (4) |
26"7 |
PET H 15O; 17mm |
Imagine or recall of |
Resting, eyes closed |
Females: bilateral inferior and orbitofrontal |
|
|
|
2 |
|
|
|
(1993) |
Normal females (3) |
24"2 |
|
a sad situation |
|
cortices activation |
|
|
|
|
|
|
Males: left inferior and orbitofrontal cortices |
|
|
|
|
|
|
activation |
Gur et al. |
Normal males (21) |
26"8 |
133Xe SPECT; |
Facial discrimination |
Resting baseline |
All three tasks produced right hemisphere |
(1994) |
Normal females (19) |
24"6 |
10mm |
using PENN facial |
|
activation |
|
|
|
|
photographs, happy± |
|
Happy and sad discrimination produced right |
|
|
|
|
neutral, sad±neutral |
|
parietal activation |
|
|
|
|
age discrimination |
|
Happy discrimination produced greater left |
|
|
|
|
|
|
frontal activation relative to sad |
|
|
|
|
|
|
discrimination |
Schneider |
Normal males (5) |
22"18 |
133Xe SPECT; |
Mood induction |
Resting baseline, |
CBF increased during sad and happy inductions |
et al. (1994) Normal females (7) |
|
10mm |
using PENN facial |
eyes open |
relative to sex discrimination and resting |
|
|
|
|
|
photographs: |
|
states |
|
|
|
|
happy, sad, sex |
|
Sad mood induction activated occipital |
|
|
|
|
discrimination |
|
temporal cortices |
George et al. |
Normal females (11) |
33.3"12.3 |
PET H 15O; 6.9mm |
Recall of sad and |
Resting baseline, |
Transient sadness increased rCBF in bilateral |
|
|
|
2 |
|
|
|
(1995) |
|
|
|
happy life events |
eyes closed |
cingulate, medial prefrontal and mesial |
|
|
|
|
followed by PENN |
|
temporal cortices |
|
|
|
|
facial photographs |
|
Transient happiness decreased rCBF in right |
|
|
|
|
|
|
prefrontal and bilateral temporoparietal |
|
|
|
|
|
|
cortices |
Schneider |
Normal males (8) |
24.8"4.5 |
PET H 15O; 6mm; |
Unsolvable anagrams |
Solvable anagrams |
Both anagram tasks increased activity in frontal |
|
|
|
2 |
|
|
|
et al. (1996) Normal females (4) |
|
coregistered with |
|
and a resting |
and temporal regions. The solvable task |
|
|
|
|
T2-weighted MRI |
|
baseline, eyes open, |
increased hippocampal activation and |
|
|
|
|
|
ears unoccluded |
decreased mamillary bodies activity, while |
unsolvable anagrams increased CBF to the mamillary bodies and amygdala and decreased hippocampal activity
