
5 курс / Пульмонология и фтизиатрия / Clinical_Tuberculosis_Friedman_Lloyd_N_,_Dedicoat
.pdf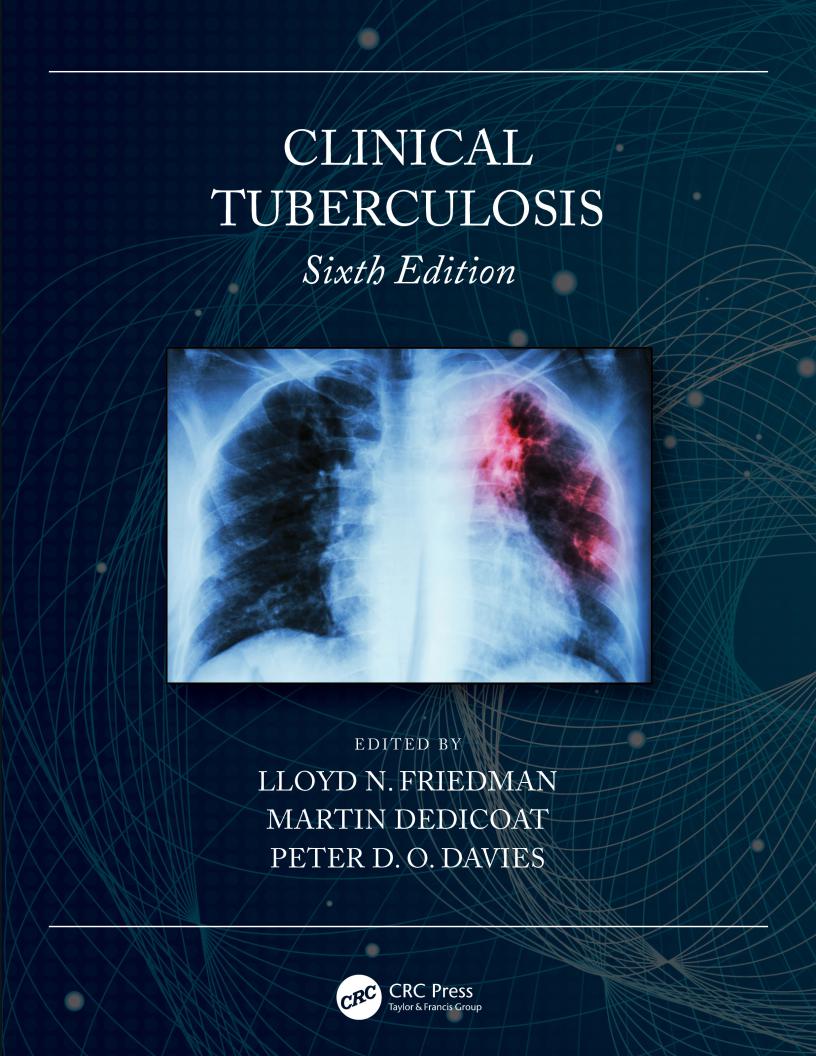
Clinical Tuberculosis
Sixth Edition

Clinical Tuberculosis
Sixth Edition
Edited by
Lloyd N. Friedman, MD
Clinical Professor of Medicine
Section of Pulmonary, Critical Care, and Sleep Medicine
Director of Inpatient Quality and Safety
Department of Internal Medicine
Yale School of Medicine
New Haven, Connecticut
Martin Dedicoat, PhD, FRCP, BSc, DTM&H
Consultant Physician in Infectious Diseases
University Hospitals Birmingham
Birmingham, United Kingdom
and
University of Warwick
Coventry, United Kingdom
Peter D. O. Davies, MA, DM, FRCP
Professor and Consultant Physician (retired)
Liverpool University
Liverpool, United Kingdom

Sixth edition published 2020 by CRC Press
6000 Broken Sound Parkway NW, Suite 300, Boca Raton, FL 33487-2742
and by CRC Press
2 Park Square, Milton Park, Abingdon, Oxon, OX14 4RN
© 2021 Taylor & Francis Group, LLC
Fourth Edition published by Hodder Arnold 2008
Fifth Edition published by CRC Press 2014
CRC Press is an imprint of Taylor & Francis Group, LLC
This book contains information obtained from authentic and highly regarded sources. While all reasonable efforts have been made to publish reliable data and information, neither the author[s] nor the publisher can accept any legal responsibility or liability for any errors or omissions that may be made. The publishers wish to make clear that any views or opinions expressed in this book by individual editors, authors or contributors are personal to them and do not necessarily reflect the views/opinions of the publishers. The information or guidance contained in this book is intended for use by medical, scientific or health-care professionals and is provided strictly as a supplement to the medical or other professional’s own judgement, their knowledge of the patient’s medical history, relevant manufacturer’s instructions and the appropriate best practice guidelines. Because of the rapid advances in medical science, any information or advice on dosages, procedures or diagnoses should be independently verified. The reader is strongly urged to consult the relevant national drug formulary and the drug companies’ and device or material manufacturers’ printed instructions, and their websites, before administering or utilizing any of the drugs, devices or materials mentioned in this book. This book does not indicate whether a particular treatment is appropriate or suitable for a particular individual. Ultimately it is the sole responsibility of the medical professional to make his or her own professional judgements, so as to advise and treat patients appropriately. The authors and publishers have also attempted to trace the copyright holders of all material reproduced in this publication and apologize to copyright holders if permission to publish in this form has not been obtained. If any copyright material has not been acknowledged please write and let us know so we may rectify in any future reprint.
Except as permitted under U.S. Copyright Law, no part of this book may be reprinted, reproduced, transmitted, or utilized in any form by any electronic, mechanical, or other means, now known or hereafter invented, including photocopying, microfilming, and recording, or in any information storage or retrieval system, without written permission from the publishers.
For permission to photocopy or use material electronically from this work, access www.copyright.com or contact the Copyright Clearance Center, Inc. (CCC), 222 Rosewood Drive, Danvers, MA 01923, 978-750-8400. For works that are not available on CCC please contact mpkbookspermissions@ tandf.co.uk
Trademark notice: Product or corporate names may be trademarks or registered trademarks, and are used only for identification and explanation without intent to infringe.
Library of Congress Cataloging-in-Publication Data
Names: Friedman, Lloyd N., editor. | Dedicoat, Martin, editor. | Davies, P. D. O., editor.
Title: Clinical tuberculosis / edited by Lloyd N. Friedman, Martin Dedicoat, Peter D.O. Davies.
Description: Sixth edition. | Boca Raton, FL : CRC Press/Taylor & Francis Group, 2020. | Includes bibliographical references and index. | Summary: “Entirely updated and revised, the 6th edition of Clinical Tuberculosis continues to provide the TB physician with a definitive and erudite account of the latest techniques in diagnosis, treatment and control of TB, including an overview of the latest guidelines from the CDC and WHO”-- Provided by publisher.
Identifiers: LCCN 2020013349 (print) | LCCN 2020013350 (ebook) | ISBN 9780815370239 (hardback) | ISBN 9781351249980 (ebook) Subjects: MESH: Tuberculosis
Classification: LCC RC311 (print) | LCC RC311 (ebook) | NLM WF 200 | DDC 616.99/5--dc23 LC record available at https://lccn.loc.gov/2020013349
LC ebook record available at https://lccn.loc.gov/2020013350
ISBN 9780815370239 (hbk)
ISBN: 9781351249980 (ebk)
Typeset in Minion Pro
by Nova Techset Private Limited, Bengaluru & Chennai, India
We would like to dedicate this book to all people in the world who are suffering from tuberculosis. Also to our wives and children who have supported us in our work.


Contents
Foreword |
ix |
|
Preface |
xiii |
|
Editors |
xv |
|
Contributors |
xvii |
|
Part I BACKGROUND |
1 |
|
1 |
The History of Tuberculosis from Earliest Times to the Development of Drugs |
3 |
|
Charlotte A. Roberts and Jane E. Buikstra |
|
2 |
Epidemiology |
17 |
|
Grant Theron, Ted Cohen, and Christopher Dye |
|
Part II PATHOLOGY AND IMMUNOLOGY |
39 |
|
3 |
Mycobacterium tuberculosis: The Genetic Organism |
41 |
|
William R. Jacobs, Jr. |
|
4 |
Pathogenesis of Tuberculosis |
51 |
|
Divya B. Reddy and Jerrold J. Ellner |
|
Part III TRANSMISSION |
77 |
|
5 |
Using Genotyping and Molecular Surveillance to Investigate Tuberculosis Transmission |
79 |
|
Sarah Talarico, Laura F. Anderson, and Benjamin J. Silk |
|
6 |
Tuberculosis Transmission Control |
97 |
|
Edward A. Nardell |
|
Part IV DIAGNOSIS OF ACTIVE DISEASE AND LATENT INFECTION |
113 |
|
7 |
Diagnosis of Active Pulmonary Tuberculosis |
115 |
|
J. Lucian Davis |
|
8 |
Radiology of Mycobacterial Disease |
129 |
|
Anne McB. Curtis |
|
9 |
Diagnosis of Latent TB Infection |
153 |
|
Ajit Lalvani, Clementine Fraser, and Manish Pareek |
|
Part V DRUGS AND VACCINES FOR TUBERCULOSIS |
173 |
|
10 |
Clinical Pharmacology of the Anti-Tuberculosis Drugs |
175 |
|
Gerry Davies and Charles Peloquin |
|
11 |
New Developments in Drug Treatment |
203 |
|
Alexander S. Pym, Camus Nimmo, and James Millard |
|
12 |
BCG and Other Vaccines |
217 |
|
Rachel Tanner and Helen McShane |
|
vii

viii Contents
Part VI CLINICAL ASPECTS AND TREATMENT |
235 |
|
13 |
Pulmonary Tuberculosis |
237 |
|
Charles S. Dela Cruz, Barbara Seaworth, and Graham Bothamley |
|
14 |
Extrapulmonary Tuberculosis |
249 |
|
Charles L. Daley |
|
15 |
Tuberculosis and Human Immunodeficiency Virus Coinfection |
267 |
|
Charisse Mandimika and Gerald Friedland |
|
16 |
Drug-Resistant Tuberculosis |
301 |
|
Keertan Dheda, Aliasgar Esmail, Anzaan Dippenaar, Robin Warren, Jennifer Furin, and Christoph Lange |
|
17 |
The Surgical Management of Tuberculosis and Its Complications |
327 |
|
Richard S. Steyn |
|
18 |
Tuberculosis in Childhood and Pregnancy |
343 |
|
Lindsay H. Cameron and Jeffrey R. Starke |
|
19 |
Treatment of Latent Tuberculosis Infection Including Risk Factors for the Development of Tuberculosis |
373 |
|
Martin Dedicoat |
|
Part VII OFFICIAL STATEMENTS: COMPARISON OF NATIONAL AND INTERNATIONAL RECOMMENDATIONS |
391 |
|
20 |
Treatment Guidelines for Active Drug-Susceptible and Drug-Resistant Pulmonary Tuberculosis, and Latent |
|
|
Tuberculosis Infection |
393 |
|
Lynn E. Sosa and Lloyd N. Friedman |
|
Part VIII CONTROL |
399 |
|
21 |
Tuberculosis Epidemic Control: A Comprehensive Strategy to Drive Down Tuberculosis |
401 |
|
Salmaan Keshavjee, Tom Nicholson, Aamir J. Khan, Lucica Ditiu, Paul E. Farmer, and Mercedes C. Becerra |
|
Part IX RELATED ASPECTS |
413 |
|
22 |
Animal Tuberculosis |
415 |
|
Catherine Wilson |
|
Index |
437 |
|
Foreword
Intro
This is the story of one overprotective mother and one lazy teenager. That “overprotective” mother turned out to be right and that “lazy teenager” went on to study English Literature and Language at Oxford University. Both lived with undiagnosed TB for over 18 years.
1997
In 1997, I (Kate) was 5 years old and had always been a happy and healthy child. My mum (Lorraine) was diagnosed with celiac disease when she was 20 years old but this was now 17 years on and it was very much under control. My grandparents, on my father’s side, owned dairy farms in Ireland and it was on a visit to County Kerry in the summer of 1997 that our lives changed. We were given a jug of warm, creamy milk to put on our cornflakes. Looking back now, it seems so obvious but back then it was nothing out of the ordinary.
Lorraine
Less than two weeks after returning from this trip to Ireland, I started to rapidly lose weight. Within a week I had lost over half a stone. At this point I had no other symptom. The following week I developed night sweats and vividly remember lying in bed, watching beads of sweat spring from nowhere and roll down my legs. By now, I also had a persistent dry, non-productive cough, accompanied by an overwhelming feeling of weakness. During this period I had seen my GP three times but there was nothing remarkable to guide him to a diagnosis. Later that week, I was admitted to the hospital, having lost over a stone of weight in less than two weeks and was subsequently diagnosed with “pneumonia.” I was told that the “pneumonia” hadn’t presented itself in the usual way—no temperature, no chesty cough, no chest pain or breathing difficulties, and only a faint mark on the chest x-ray. The consultants asked whether I had been outside of Europe but no one asked about Ireland. After a week of IVs I was discharged. However, on returning home I was still too weak to walk and would have to crawl on my hands and knees to make it up the stairs. The weakness remained overwhelming and even trying to lift the kettle to make a drink caused me to retch. A physio was sent to the house to try to help me to get back on my feet. It took weeks for me to master even climbing up the stairs which eventually led the medics to believe this weakness must be in some way psychosomatic. Three months later I still had no appetite and had not put on any weight.
I was later given a pneumonia vaccine but within just a few weeks, I was told the pneumonia had returned. This characterized the next few years: recurrent chest infections, antibiotics, and IVs.
I underwent extensive tests, but no one could identify the cause. In the end I was told that it must be because I was a celiac; I “obviously had a weak immune system.”
Kate
Aged 10, I came home from school and collapsed in the hallway with what I can only describe as extreme weakness, a feeling I came to recognize as the years progressed. Prior to this, I had been an active and energetic child. That evening, the shivers began and then the sickness. At this point, I had no cough and no temperature. Yet, my “overprotective” mother recognized the sensation of being too exhausted and feeling too weak to even speak. “I think my daughter has pneumonia,” she said to the local GP’s surgery, to which they told her to calm down, “Stop overreacting, Mrs. Tuohy.” Later that day, I was admitted to the hospital and diagnosed with pneumonia.
The following year my appendix burst. Meanwhile, I continued to have recurrent chest infections which were treated with oral antibiotics. A chest infection meant losing weight, extreme weakness, feeling too unwell to speak or move, no appetite, and feeling sick. Our infections were 100% debilitating.
I was aged 14 when the situation worsened. I lost a stone in a month, next my appetite went (and never returned), then the sweats and shivers began, and only when I began to feel really ill did the dry cough emerge. This was a pattern which repeated itself over the next 8 years; that dry cough used to send us into panic mode. I was constantly being diagnosed with “pneumonia” and the endless tests began. I was referred to numerous hospitals but every test came back negative. Then my tummy began to grow, a bit of bloating to start with; “Stop fussing and do some exercise,” I was told again and again. The reality, without laxatives I never went to the toilet and, by the time I was 16, I was regularly being asked by doctors whether I was, in fact, pregnant.
My body was slim but my tummy was rock solid and distended. They ruled out celiac disease with a biopsy and then I underwent x-rays, ultrasounds, barium meals, and MRIs. The consultants eventually concluded that they had never seen anything like it and the only option was a laparoscopy.
In the middle of the laparoscopy, the surgeon came out to my parents and informed them that he was going to have to resect part of my terminal ileum which, for no apparent reason, was nonfunctioning and blocked with undigested food. The surrounding intestine also didn’t look normal. The surgeon had never come across this before. Over four hours later, I emerged from the operation. For a few weeks, my gastro symptoms improved, but slowly my lower abdomen began to grow and was doughy in texture, I was back to taking laxatives, on painkillers for spasms, and occasionally admitted with violent sickness and given IV pain relief. This was my GCSE year and, by this point, there had been large
ix
