
5 курс / Пульмонология и фтизиатрия / Clinical_Tuberculosis_Friedman_Lloyd_N_,_Dedicoat
.pdf
90 Using Genotyping and Molecular Surveillance to Investigate Tuberculosis Transmission
Identifying how laboratory cross-contamination occurred can be further complicated by the need to refer specimens and isolates from clinical settings to commercial and reference laboratories for additional testing.
Laboratorians and TB control program staff can use genotyping data to monitor for and detect potential false-positive culture results. In countries with universal genotyping services, prospective strain typing of M. tuberculosis isolates can facilitate detection. If available, an isolate from a specimen collected on a different date can be submitted for repeat genotyping when contamination is suspected to determine if the patient’s first and second genotyping results differ from one another. Unusual genotyping results, such as matches to reference strains used for proficiency testing or quality control that are not transmitted in the community (e.g., H37Rv), may indicate that a result is either falsely positive or has resulted from an occupational laboratory exposure. Genotyping results should also be reviewed if there is no alternative explanation for an unusual increase in isolates with the same drug-resistance pattern or an unexpected increase in the percentage of culture-positive results.
False-positive investigations are a multidisciplinary endeavor that should involve laboratorians, clinicians, and other TB program staff. Clinical indicators of false positivity include a single positive culture from multiple specimens collected for a new patient, prolonged incubation time with late appearing growth (liquid media) or scanty growth (solid media), the absence of clinical or radiographic findings consistent with TB, and another confirmed diagnosis that is consistent with the patient’s clinical presentation. Indistinguishable genotyping results provide evidence for false positivity if isolates from different patients or reference strains were recently processed in the same laboratory or different patients’ specimens were collected recently in the same facility. Reference laboratories can routinely monitor for clustering of isolates from source laboratories. Many laboratories have also developed policies and procedures to minimize and detect M. tuberculosis cross-contamination.
REFERENCES
1.Thierry D, Matsiota-Bernard P, Pitsouni E, Costopoulos C, and Guesdon JL. Use of the insertion element IS6110 for DNA fingerprinting of Mycobacterium tuberculosis isolates presenting various profiles of drug susceptibility. FEMS Immunol Med Microbiol. 1993;6(4):287–97.
2.Schurch AC, and van Soolingen D. DNA fingerprinting of Mycobacterium tuberculosis: From phage typing to whole-genome sequencing. Infect Genet Evol. 2012;12(4):602–9.
3.de Boer AS, Borgdorff MW, de Haas PE, Nagelkerke NJ, van Embden JD, and van Soolingen D. Analysis of rate of change of IS6110 RFLP patterns of Mycobacterium tuberculosis based on serial patient isolates. J Infect Dis. 1999;180(4):1238–44.
4.Groenen PM, Bunschoten AE, van Soolingen D, and van Embden JD. Nature of DNA polymorphism in the direct repeat cluster of Mycobacterium tuberculosis; application for strain differentiation by a novel typing method. Mol Microbiol. 1993;10(5):1057–65.
5.Kamerbeek J et al. Simultaneous detection and strain differentiation of Mycobacterium tuberculosis for diagnosis and epidemiology. J Clin Microbiol. 1997;35(4):907–14.
6.Kremer K et al. Comparison of methods based on different molecular epidemiological markers for typing of Mycobacterium tuberculosis complex strains: Interlaboratory study of discriminatory power and reproducibility. J Clin Microbiol. 1999;37(8):2607–18.
7.Goyal M, Saunders NA, van Embden JD, Young DB, and Shaw RJ. Differentiation of Mycobacterium tuberculosis isolates by spoligotyping and IS6110 restriction fragment length polymorphism. J Clin Microbiol. 1997;35(3):647–51.
8.Tsolaki AG et al. Genomic deletions classify the Beijing/W strains as a distinct genetic lineage of Mycobacterium tuberculosis. J Clin Microbiol. 2005;43(7):3185–91.
9.Cowan LS et al. Evaluation of a two-step approach for large-scale, prospective genotyping of Mycobacterium tuberculosis isolates in the United States. J Clin Microbiol. 2005;43(2):688–95.
10.Supply P et al. Proposal for standardization of optimized mycobacterial interspersed repetitive unit-variable-number tandem repeat typing of Mycobacterium tuberculosis. J Clin Microbiol. 2006;44(12):4498–510.
11.Maes M, Kremer K, van Soolingen D, Takiff H, and de Waard JH. 24-locus MIRU-VNTR genotyping is a useful tool to study the molecular epidemiology of tuberculosis among Warao Amerindians in Venezuela. Tuberculosis. 2008;88(5):490–4.
12.Christianson S et al. Evaluation of 24 locus MIRU-VNTR genotyping of Mycobacterium tuberculosis isolates in Canada. Tuberculosis. 2010;90(1):31–8.
13.de Beer JL, Kremer K, Kodmon C, Supply P, van Soolingen D, and Global Network for the Molecular Surveillance of T. First worldwide proficiency study on variable-number tandem-repeat typing of Mycobacterium tuberculosis complex strains. J Clin Microbiol. 2012;50(3):662–9.
14.Cowan LS et al. Evaluation of mycobacterial interspersed repet- itive-unit-variable-number tandem-repeat genotyping as performed in laboratories in Canada, France, and the United States. J Clin Microbiol. 2012;50(5):1830–1.
15.National TB Controllers Association/CDC Advisory Group on Tuberculosis Genotyping. Guide to the Application of Genotyping to Tuberculosis Prevention and Control. Atlanta, GA: US Department of Health and Human Services, CDC; June 2004. Available at: https:// www.cdc.gov/tb/programs/genotyping/manual.htm.
16.Anderson L et al. The national strain typing service. Tuberculosis in the UK: annual report on tuberculosis surveillance in the UK 2010. 2010:28–30.
17.Gopaul KK, Brown TJ, Gibson AL, Yates MD, and Drobniewski FA. Progression toward an improved DNA amplification-based typing technique in the study of Mycobacterium tuberculosis epidemiology. J Clin Microbiol. 2006;44(7):2492–8.
18.Cowan LS, Mosher L, Diem L, Massey JP, and Crawford JT. Variablenumber tandem repeat typing of Mycobacterium tuberculosis isolates with low copy numbers of IS6110 by using mycobacterial interspersed repetitive units. J Clin Microbiol. 2002;40(5):1592–602.
19.Valcheva V, Mokrousov I, Narvskaya O, Rastogi N, and Markova N. Utility of new 24-locus variable-number tandem-repeat typing for discriminating Mycobacterium tuberculosis clinical isolates collected in Bulgaria. J Clin Microbiol. 2008;46(9):3005–11.
20.Barlow RE, Gascoyne-Binzi DM, Gillespie SH, Dickens A, Qamer S, and Hawkey PM. Comparison of variable number tandem repeat and IS6110-restriction fragment length polymorphism analyses for discrimination of highand low-copy-number IS6110 Mycobacterium tuberculosis isolates. J Clin Microbiol. 2001;39(7):2453–7.
21.Allix-Beguec C, Fauville-Dufaux M, and Supply P. Three-year population-based evaluation of standardized mycobacterial interspersed repetitive-unit-variable-number tandem-repeat typing of
Mycobacterium tuberculosis. J Clin Microbiol. 2008;46(4):1398–406.
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

References 91
22. Bidovec-Stojkovic U, Zolnir-Dovc M, and Supply P. One year nationwide evaluation of 24-locus MIRU-VNTR genotyping on Slovenian Mycobacterium tuberculosis isolates. Respir Med. 2011;105 Suppl 1:S67–73.
23.Sola C et al. Genotyping of the Mycobacterium tuberculosis complex using MIRUs: Association with VNTR and spoligotyping for molecular epidemiology and evolutionary genetics. Infect Genet Evol. 2003;3(2):125–33.
24.Oelemann MC et al. Assessment of an optimized mycobacterial interspersed repetitive-unit-variable-number tandem-repeat typing system combined with spoligotyping for population-based molecular epidemiology studies of tuberculosis. J Clin Microbiol. 2007;45(3):691–7.
25.Vadwai V, Shetty A, Supply P, and Rodrigues C. Evaluation of 24-locus MIRU-VNTR in extrapulmonary specimens: Study from a tertiary centre in Mumbai. Tuberculosis. 2012;92(3):264–72.
26.Cole ST, and Barrell BG. Analysis of the genome of Mycobacterium tuberculosis H37Rv. Novartis Found Symp. 1998;217:160–72; discussion 72-7.
27.Walker TM et al. Whole-genome sequencing to delineate Mycobacterium tuberculosis outbreaks: A retrospective observational study. Lancet Infect Dis. 2013;13(2):137–46.
28.Bryant JM et al. Inferring patient to patient transmission of Mycobacterium tuberculosis from whole genome sequencing data. BMC Infect Dis. 2013;13:110.
29.Ford CB et al. Use of whole genome sequencing to estimate the mutation rate of Mycobacterium tuberculosis during latent infection. Nat Genet. 2011;43(5):482–6.
30.Roetzer A et al. Whole genome sequencing versus traditional genotyping for investigation of a Mycobacterium tuberculosis outbreak: A longitudinal molecular epidemiological study. PLoS Med. 2013;10(2):e1001387.
31.Colangeli R et al. Whole genome sequencing of Mycobacterium tuberculosis reveals slow growth and low mutation rates during latent infections in humans. PLOS ONE. 2014;9(3):e91024.
32.Kohl TA et al. Whole-genome-based Mycobacterium tuberculosis surveillance: A standardized, portable, and expandable approach. J Clin Microbiol. 2014;52(7):2479–86.
33.Brown AC et al. Rapid whole-genome sequencing of Mycobacterium tuberculosis isolates directly from clinical samples. J Clin Microbiol. 2015;53(7):2230–7.
34.Votintseva AA et al. Same-day diagnostic and surveillance data for tuberculosis via whole-genome sequencing of direct respiratory samples. J Clin Microbiol. 2017;55(5):1285–98.
35.Alland D et al. Transmission of tuberculosis in New York City. An analysis by DNA fingerprinting and conventional epidemiologic methods. N Engl J Med. 1994;330(24):1710–6.
36.Small PM et al. The epidemiology of tuberculosis in San Francisco. A population-based study using conventional and molecular methods. N Engl J Med. 1994;330(24):1703–9.
37.Vynnycky E, Borgdorff MW, van Soolingen D, and Fine PE. Annual Mycobacterium tuberculosis infection risk and interpretation of clustering statistics. Emerg Infect Dis. 2003;9(2):176–83.
38.Dahle UR, Sandven P, Heldal E, and Caugant DA. Molecular epidemiology of Mycobacterium tuberculosis in Norway. J Clin Microbiol. 2001;39(5):1802–7.
39.Dahle UR, Sandven P, Heldal E, and Caugant DA. Continued low rates of transmission of Mycobacterium tuberculosis in Norway. J Clin Microbiol. 2003;41(7):2968–73.
40.de Vries G, Baars HW, Sebek MM, van Hest NA, and Richardus JH. Transmission classification model to determine place and time of infection of tuberculosis cases in an urban area. J Clin Microbiol. 2008;46(12):3924–30.
41.Fenner L et al. Mycobacterium tuberculosis transmission in a country with low tuberculosis incidence: Role of immigration and HIV infection. J Clin Microbiol. 2012;50(2):388–95.
42.Gutierrez MC et al. Molecular fingerprinting of Mycobacterium tuberculosis and risk factors for tuberculosis transmission in Paris, France, and surrounding area. J Clin Microbiol. 1998; 36(2):486–92.
43.Heldal E, Docker H, Caugant DA, and Tverdal A. Pulmonary tuberculosis in Norwegian patients. The role of reactivation, reinfection and primary infection assessed by previous mass screening data and restriction fragment length polymorphism analysis.
Int J Tuberc Lung Dis. 2000;4(4):300–7.
44.Hernandez-Garduno E et al. Predictors of clustering of tuberculosis in Greater Vancouver: A molecular epidemiologic study. CMAJ. 2002;167(4):349–52.
45.Kamper-Jorgensen Z et al. Clustered tuberculosis in a low-burden country: Nationwide genotyping through 15 years. J Clin Microbiol. 2012;50(8):2660–7.
46.Kik SV et al. Tuberculosis outbreaks predicted by characteristics of first patients in a DNA fingerprint cluster. Am J Respir Crit Care Med. 2008;178(1):96–104.
47.van Deutekom H, Gerritsen JJ, van Soolingen D, van Ameijden EJ, van Embden JD, and Coutinho RA. A molecular epidemiological approach to studying the transmission of tuberculosis in Amsterdam. Clin Infect Dis. 1997;25(5):1071–7.
48.van Deutekom H et al. Clustered tuberculosis cases: Do they represent recent transmission and can they be detected earlier? Am J Respir Crit Care Med. 2004;169(7):806–10.
49.Vanhomwegen J et al. Impact of immigration on the molecular epidemiology of tuberculosis in Rhode Island. J Clin Microbiol. 2011;49(3):834–44.
50.Verver S et al. Transmission of tuberculosis in a high incidence urban community in South Africa. Int J Epidemiol. 2004;33(2):351–7.
51.Fok A, Numata Y, Schulzer M, and FitzGerald MJ. Risk factors for clustering of tuberculosis cases: A systematic review of popula- tion-based molecular epidemiology studies. Int J Tuberc Lung Dis. 2008;12(5):480–92.
52.Borgdorff MW, Nagelkerke NJ, van Soolingen D, and Broekmans JF. Transmission of tuberculosis between people of different ages in The Netherlands: An analysis using DNA fingerprinting. Int J Tuberc Lung Dis. 1999;3(3):202–6.
53.Heldal E et al. Risk factors for recent transmission of Mycobacterium tuberculosis. Eur Respir J. 2003;22(4):637–42.
54.Maguire H et al. Molecular epidemiology of tuberculosis in London 1995–7 showing low rate of active transmission. Thorax. 2002;57(7):617–22.
55.Feng JY et al. Clinical and bacteriological characteristics associated with clustering of multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2017;21(7):766–73.
56.Glynn JR, Vynnycky E, and Fine PE. Influence of sampling on estimates of clustering and recent transmission of Mycobacterium tuberculosis derived from DNA fingerprinting techniques. Am J Epidemiol. 1999;149(4):366–71.
57.Vynnycky E, Nagelkerke N, Borgdorff MW, van Soolingen D, van Embden JD, and Fine PE. The effect of age and study duration on the relationship between ‘clustering’ of DNA fingerprint patterns and the proportion of tuberculosis disease attributable to recent transmission. Epidemiol Infect. 2001;126(1):43–62.
58.de Vries G, van Hest NA, Burdo CC, van Soolingen D, and Richardus JH. A Mycobacterium tuberculosis cluster demonstrating the use of genotyping in urban tuberculosis control. BMC Infect Dis. 2009;9(151).

92 Using Genotyping and Molecular Surveillance to Investigate Tuberculosis Transmission
59.Hamblion EL et al. Recent TB transmission, clustering and predictors of large clusters in London, 2010–2012: Results from first 3 years of universal MIRU-VNTR strain typing. Thorax. 2016;71(8):749–56.
60.Guthrie JL et al. Molecular epidemiology of tuberculosis in British Columbia, Canada: A 10-year retrospective study. Clin Infect Dis. 2018;66(6):849–56.
61.Powell KM et al. Outbreak of drug-resistant Mycobacterium tuberculosis among homeless people in Atlanta, Georgia, 2008–2015. Public Health Rep. 2017;132(2):231–40.
62.Noppert GA, Yang Z, Clarke P, Ye W, Davidson P, and Wilson ML. Individualand neighborhood-level contextual factors are associated with Mycobacterium tuberculosis transmission: Genotypic clustering of cases in Michigan, 2004–2012. Ann Epidemiol. 2017;27(6):371–6 e5.
63.Wang T, Xue F, Chen Y, Ma Y, and Liu Y. The spatial epidemiology of tuberculosis in Linyi City, China, 2005–2010. BMC Public Health. 2012;12:885.
64.Ribeiro FK et al. Genotypic and spatial analysis of Mycobacterium tuberculosis transmission in a high-incidence urban setting. Clin Infect Dis. 2015;61(5):758–66.
65.Jenkins HE et al. Assessing spatial heterogeneity of multidrugresistant tuberculosis in a high-burden country. Eur Respir J. 2013;42(5):1291–301.
66.Lin HH, Shin SS, Contreras C, Asencios L, Paciorek CJ, and Cohen
T.Use of spatial information to predict multidrug resistance in tuberculosis patients, Peru. Emerg Infect Dis. 2012;18(5):811–13.
67.Dowdy DW, Golub JE, Chaisson RE, and Saraceni V. Heterogeneity in tuberculosis transmission and the role of geographic hotspots in propagating epidemics. Proc Natl Acad Sci USA. 2012;109(24):9557–62.
68.Shaweno D et al. Methods used in the spatial analysis of tuberculosis epidemiology: A systematic review. BMC Med. 2018;16(1):193.
69.Althomsons SP et al. Statistical method to detect tuberculosis outbreaks among endemic clusters in a low-incidence setting. Emerg Infect Dis. 2018;24(3):573–5.
70.Moonan PK, Ghosh S, Oeltmann JE, Kammerer JS, Cowan LS, and Navin TR. Using genotyping and geospatial scanning to estimate recent Mycobacterium tuberculosis transmission, United States. Emerg Infect Dis. 2012;18(3):458–65.
71.France AM, Grant J, Kammerer JS, and Navin TR. A field-validated approach using surveillance and genotyping data to estimate tuberculosis attributable to recent transmission in the United States. Am
JEpidemiol. 2015;182(9):799–807.
72.Yuen CM, Kammerer JS, Marks K, Navin TR, and France AM. Recent transmission of tuberculosis—United States, 2011–2014. PLOS ONE. 2016;11(4):e0153728.
73.Teeter LD et al. Evaluation of 24-locus MIRU-VNTR genotyping in Mycobacterium tuberculosis cluster investigations in four jurisdictions in the United States, 2006–2010. Tuberculosis. 2017;106:9–15.
74.Centers for Disease Control and Prevention. Reported Tuberculosis in the United States, 2017. Available at: https://www.cdc.gov/tb/statistics/reports/2017/2017_Surveillance_FullReport.pdf.
75.Bothamley GH. Strain typing and contact tracing—A clinician’s viewpoint. Tuberculosis. 2007;87(3):173–5.
76.Ghosh S, Moonan PK, Cowan L, Grant J, Kammerer S, and Navin TR. Tuberculosis genotyping information management system: Enhancing tuberculosis surveillance in the United States. Infect Genet Evol. 2012;12(4):782–8.
77.Centers for Disease Control and Prevention. Prioritizing tuberculosis genotype clusters for further investigation and public health action [updated 2017]. Available at: https://www.cdc.gov/ tb/programs/genotyping/Prioritizing_Tuberculosis_Genotype_ Clusters_August2017.pdf.
78.Davidson JA, Anderson LF, Adebisi V, de Jongh L, Burkitt A, and Lalor MK. Creating a web-based electronic tool to aid tuberculosis (TB) cluster investigation: Data integration in TB surveillance activities in the United Kingdom, 2013 to 2016. Euro Surveill. 2018;23(44).
79.Hamblion EL et al. Public health outcome of Tuberculosis Cluster Investigations, England 2010–2013. J Infect. 2019;78(4):269–74.
80.Diel R, Rusch-Gerdes S, and Niemann S. Molecular epidemiology of tuberculosis among immigrants in Hamburg, Germany. J Clin Microbiol. 2004;42(7):2952–60.
81.Gardy JL et al. Whole-genome sequencing and social-network analysis of a tuberculosis outbreak. N Engl J Med. 2011;364(8):730–9.
82.Stucki D et al. Standard genotyping overestimates transmission of Mycobacterium tuberculosis among immigrants in a low-incidence country. J Clin Microbiol. 2016;54(7):1862–70.
83.Jamieson FB, Teatero S, Guthrie JL, Neemuchwala A, Fittipaldi N, and Mehaffy C. Whole-genome sequencing of the Mycobacterium tuberculosis Manila sublineage results in less clustering and better resolution than mycobacterial interspersed repetitive-unit-vari- able-number tandem-repeat (MIRU-VNTR) typing and spoligotyping. J Clin Microbiol. 2014;52(10):3795–8.
84.Koster KJ et al. Genomic sequencing is required for identification of tuberculosis transmission in Hawaii. BMC Infect Dis. 2018;18(1):608.
85.Gurjav U et al. Whole genome sequencing demonstrates limited transmission within identified Mycobacterium tuberculosis clusters in New South Wales, Australia. PLOS ONE. 2016;11(10):e0163612.
86.Bjorn-Mortensen K et al. Tracing Mycobacterium tuberculosis transmission by whole genome sequencing in a high incidence setting: A retrospective population-based study in East Greenland. Sci Rep. 2016;6:33180.
87.Meehan CJ et al. The relationship between transmission time and clustering methods in Mycobacterium tuberculosis epidemiology. EBioMedicine. 2018;37:410–6.
88.Casali N, Broda A, Harris SR, Parkhill J, Brown T, and Drobniewski F. Whole genome sequence analysis of a large isoniazid-resistant tuberculosis outbreak in London: A Retrospective Observational Study. PLoS Med. 2016;13(10):e1002137.
89.Tyler AD et al. Application of whole genome sequence analysis to the study of Mycobacterium tuberculosis in Nunavut, Canada. PLOS ONE. 2017;12(10):e0185656.
90.Didelot X, Gardy J, and Colijn C. Bayesian inference of infectious disease transmission from whole-genome sequence data. Mol Biol Evol. 2014;31(7):1869–79.
91.Stimson J, Gardy J, Mathema B, Crudu V, Cohen T, and Colijn C. Beyond the SNP threshold: Identifying outbreak clusters using inferred transmissions. Mol Biol Evol. 2019;36(3):587–603.
92.Jajou R et al. Epidemiological links between tuberculosis cases identified twice as efficiently by whole genome sequencing than conventional molecular typing: A population-based study. PLOS ONE. 2018;13(4):e0195413.
93.Walker TM et al. Assessment of Mycobacterium tuberculosis transmission in Oxfordshire, UK, 2007–12, with whole pathogen genome sequences: An observational study. Lancet Respir Med. 2014;2(4):285–92.
94.Lalor MK et al. The use of whole-genome sequencing in cluster investigation of a multidrug-resistant tuberculosis outbreak. Eur Respir J. 2018;51(6).
95.Teeter LD et al. Validation of genotype cluster investigations for Mycobacterium tuberculosis: Application results for 44 clusters from four heterogeneous United States jurisdictions. BMC Infect Dis. 2016;16(1):594.
96.Dahle UR et al. Tuberculosis in contacts need not indicate disease transmission. Thorax. 2005;60(2):136–7.
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

References 93
97.Bennett DE et al. DNA fingerprinting of Mycobacterium tuberculosis isolates from epidemiologically linked case pairs. Emerg Infect Dis. 2002;8(11):1224–9.
98.Borrell S et al. Factors associated with differences between conventional contact tracing and molecular epidemiology in study of tuberculosis transmission and analysis in the city of Barcelona, Spain. J Clin Microbiol. 2009;47(1):198–204.
99.Verver S et al. Proportion of tuberculosis transmission that takes place in households in a high-incidence area. Lancet. 2004;363(9404):212–4.
100.Glynn JR et al. Whole genome sequencing shows a low proportion of tuberculosis disease is attributable to known close contacts in rural Malawi. PLOS ONE. 2015;10(7):e0132840.
101.Sintchenko V, and Gilbert GL. Utility of genotyping of Mycobacterium tuberculosis in the contact investigation: A decision analysis. Tuberculosis. 2007;87(3):176–84.
102.Jackson AD et al. Characterising transmission of a tuberculosis genotype in Scotland: A qualitative approach to social network enquiry. Int J Tuberc Lung Dis. 2009;13(4):486–93.
103.Fleischmann RD et al. Whole-genome comparison of Mycobacterium tuberculosis clinical and laboratory strains. J Bacteriol. 2002;184(19):5479–90.
104. Gagneux S et al. Variable host-pathogen compatibility in Mycobacterium tuberculosis. Proc Natl Acad Sci USA. 2006;103(8):2869–73.
105.Kato-Maeda M et al. Strain classification of Mycobacterium tuberculosis: Congruence between large sequence polymorphisms and spoligotypes. Int J Tuberc Lung Dis. 2011;15(1):131–3.
106.Brown T, Nikolayevskyy V, Velji P, and Drobniewski F. Associations between Mycobacterium tuberculosis strains and phenotypes. Emerg Infect Dis. 2010;16(2):272–80.
107.Ghebremichael S et al. Drug resistant Mycobacterium tuberculosis of the Beijing genotype does not spread in Sweden. PLOS ONE. 2010;5(5):e10893.
108.Phyu S, Stavrum R, Lwin T, Svendsen OS, Ti T, and Grewal HM. Predominance of Mycobacterium tuberculosis EAI and Beijing lineages in Yangon, Myanmar. J Clin Microbiol. 2009;47(2):335–44.
109.Coscolla M, and Gagneux S. Does M. tuberculosis genomic diversity explain disease diversity? Drug Discov Today Dis Mech. 2010;7(1):e43–59.
110.Hershberg R et al. High functional diversity in Mycobacterium tuberculosis driven by genetic drift and human demography. PLoS Biol. 2008;6(12):e311.
111.Huang SF et al. Association of Mycobacterium tuberculosis genotypes and clinical and epidemiological features—A multi-center study in Taiwan. Infect Genet Evol. 2012;12(1):28–37.
112.Arora J et al. Characterization of predominant Mycobacterium tuberculosis strains from different subpopulations of India. Infect Genet Evol. 2009;9(5):832–9.
113.Lahlou O et al. The genotypic population structure of Mycobacterium tuberculosis complex from Moroccan patients reveals a predominance of Euro-American lineages. PLOS ONE. 2012;7(10):e47113.
114.GibsonA, Brown T, Baker L, and DrobniewskiF. Can 15-locus mycobacterial interspersed repetitive unit-variable-number tandem repeat analysis provide insight into the evolution of Mycobacterium tuberculosis? Appl Environ Microbiol. 2005;71(12):8207–13.
115.Filliol I et al. Global distribution of Mycobacterium tuberculosis spoligotypes. Emerg Infect Dis. 2002;8(11):1347–9.
116.Brudey K et al. Mycobacterium tuberculosis complex genetic diversity: Mining the fourth international spoligotyping database (SpolDB4) for classification, population genetics and epidemiology. BMC Microbiol. 2006;6:23.
117.Gutacker MM et al. Single-nucleotide polymorphism-based population genetic analysis of Mycobacterium tuberculosis strains from 4 geographic sites. J Infect Dis. 2006;193(1):121–8.
118.Weniger T, Krawczyk J, Supply P, Niemann S, and Harmsen D. MIRU-VNTRplus: A web tool for polyphasic genotyping of
Mycobacterium tuberculosis complex bacteria. Nucleic Acids Res. 2010;38:W326–31.
119.Shabbeer A et al. TB-Lineage: An online tool for classification and analysis of strains of Mycobacterium tuberculosis complex. Infect Genet Evol. 2012;12(4):789–97.
120. Merker M et al. Evolutionary history and global spread of the Mycobacterium tuberculosis Beijing lineage. Nat Genet. 2015;47(3):242–9.
121.Metcalfe JZ et al. Determinants of multidrug-resistant tuberculosis clusters, California, USA, 2004–2007. Emerg Infect Dis. 2010;16(9):1403–9.
122.Click ES, Moonan PK, Winston CA, Cowan LS, and Oeltmann JE. Relationship between Mycobacterium tuberculosis phylogenetic lineage and clinical site of tuberculosis. Clin Infect Dis. 2012;54(2):211–9.
123.Pareek M et al. Ethnicity and mycobacterial lineage as determinants of tuberculosis disease phenotype. Thorax. 2013;68(3):221–9.
124.van der Spuy GD et al. Changing Mycobacterium tuberculosis population highlights clade-specific pathogenic characteristics. Tuberculosis. 2009;89(2):120–5.
125.Reed MB et al. A glycolipid of hypervirulent tuberculosis strains that inhibits the innate immune response. Nature. 2004;431(7004):84–7.
126.Sinsimer D et al. The phenolic glycolipid of Mycobacterium tuberculosis differentially modulates the early host cytokine response but does not in itself confer hypervirulence. Infect Immun. 2008;76(7):3027–36.
127.Hanekom M, Gey van Pittius NC, McEvoy C, Victor TC, Van Helden PD, and Warren RM. Mycobacterium tuberculosis Beijing genotype: A template for success. Tuberculosis. 2011;91(6):510–23.
128.Yang C et al. Mycobacterium tuberculosis Beijing strains favor transmission but not drug resistance in China. Clin Infect Dis. 2012;55(9):1179–87.
129.Ribeiro SC et al. Mycobacterium tuberculosis strains of the modern sublineage of the Beijing family are more likely to display increased virulence than strains of the ancient sublineage. J Clin Microbiol. 2014;52(7):2615–24.
130.van Laarhoven A et al. Low induction of proinflammatory cytokines parallels evolutionary success of modern strains within the Mycobacterium tuberculosis Beijing genotype. Infect Immun. 2013;81(10):3750–6.
131.Chen YY et al. The pattern of cytokine production in vitro induced by ancient and modern Beijing Mycobacterium tuberculosis strains. PLOS ONE. 2014;9(4):e94296.
132.Albanna AS et al. Reduced transmissibility of East African Indian strains of Mycobacterium tuberculosis. PLOS ONE. 2011;6(9):e25075.
133.Nebenzahl-Guimaraes H, Verhagen LM, Borgdorff MW, and
van Soolingen D. Transmission and progression to disease of Mycobacterium tuberculosis phylogenetic lineages in the Netherlands. J Clin Microbiol. 2015;53(10):3264–71.
134.Guerra-Assuncao JA et al. Large-scale whole genome sequencing of M. tuberculosis provides insights into transmission in a high prevalence area. Elife. 2015;4.
135.Feng JY et al. Impact of Euro-American sublineages of Mycobacterium tuberculosis on new infections among named contacts. Int J Tuberc Lung Dis. 2017;21(5):509–16.
136.Lee RS et al. Population genomics of Mycobacterium tuberculosis in the Inuit. Proc Natl Acad Sci USA. 2015;112(44):13609–14.

94 Using Genotyping and Molecular Surveillance to Investigate Tuberculosis Transmission
137.World Health Organization. Global tuberculosis report 2017, 2017. Available at: http://www.whoint/tb/publications/global_report/ en/.
138.Dye C, Williams BG, Espinal MA, and Raviglione MC. Erasing the world’s slow stain: Strategies to beat multidrug-resistant tuberculosis. Science. 2002;295(5562):2042–6.
139.Borrell S, and Gagneux S. Infectiousness, reproductive fitness and evolution of drug-resistant Mycobacterium tuberculosis. Int J Tuberc Lung Dis. 2009;13(12):1456–66.
140.Cohen T, Sommers B, and Murray M. The effect of drug resistance on the fitness of Mycobacterium tuberculosis. Lancet Infect Dis. 2003;3(1):13–21.
141.Fox GJ, Schaaf HS, Mandalakas A, Chiappini E, Zumla A, and Marais BJ. Preventing the spread of multidrug-resistant tuberculosis and protecting contacts of infectious cases. Clin Microbiol Infect. 2017;23(3):147–53.
142.Kendall EA, Fofana MO, and Dowdy DW. Burden of transmitted multidrug resistance in epidemics of tuberculosis: A transmission modelling analysis. Lancet Respir Med. 2015;3(12):963–72.
143.Middlebrook G, and Cohn ML. Some observations on the pathogenicity of isoniazid-resistant variants of tubercle bacilli. Science. 1953;118(3063):297–9.
144.Mitchison DA. Tubercle bacilli resistant to isoniazid; virulence and response to treatment with isoniazid in guinea-pigs. Br Med J. 1954;1(4854):128–30.
145.Pym AS, Saint-Joanis B, and Cole ST. Effect of katG mutations on the virulence of Mycobacterium tuberculosis and the implication for transmission in humans. Infect Immun. 2002;70(9):4955–60.
146.Ordway DJ, Sonnenberg MG, Donahue SA, Belisle JT, and Orme IM. Drug-resistant strains of Mycobacterium tuberculosis exhibit a range of virulence for mice. Infect Immun. 1995;63(2):741–3.
147.van Soolingen D, de Haas PE, van Doorn HR, Kuijper E, Rinder H, and Borgdorff MW. Mutations at amino acid position 315 of the katG gene are associated with high-level resistance to isoniazid, other drug resistance, and successful transmission of
Mycobacterium tuberculosis in the Netherlands. J Infect Dis. 2000;182(6):1788–90.
148.Hu Y, Mathema B, Jiang W, Kreiswirth B, Wang W, and Xu B. Transmission pattern of drug-resistant tuberculosis and its implication for tuberculosis control in eastern rural China. PLOS ONE. 2011;6(5):e19548.
149.Gagneux S et al. Impact of bacterial genetics on the transmission of isoniazid-resistant Mycobacterium tuberculosis. PLoS Pathog. 2006;2(6):e61.
150.Gagneux S, Long CD, Small PM, Van T, Schoolnik GK, and Bohannan BJ. The competitive cost of antibiotic resistance in
Mycobacterium tuberculosis. Science. 2006;312(5782):1944–6.
151.Gilpin CM et al. Evidence of primary transmission of multidrugresistant tuberculosis in the Western Province of Papua New Guinea. Med J Aust. 2008;188(3):148–52.
152.Streicher EM et al. Emergence and treatment of multidrug resistant (MDR) and extensively drug-resistant (XDR) tuberculosis in South Africa. Infect Genet Evol. 2012;12(4):686–94.
153.Leung EC et al. Transmission of multidrug-resistant and extensively drug-resistant tuberculosis in a metropolitan city. Eur Respir J. 2013;41(4):901–8.
154.Senghore M et al. Whole-genome sequencing illuminates the evolution and spread of multidrug-resistant tuberculosis in Southwest Nigeria. PLOS ONE. 2017;12(9):e0184510.
155.Black PA et al. Whole genome sequencing reveals genomic heterogeneity and antibiotic purification in Mycobacterium tuberculosis isolates. BMC Genomics. 2015;16:857.
156.Nsofor CA et al. Transmission is a noticeable cause of resistance among treated tuberculosis patients in Shanghai, China. Sci Rep. 2017;7(1):7691.
157.Shah NS et al. Transmission of extensively drug-resistant tuberculosis in South Africa. N Engl J Med. 2017;376(3):243–53.
158.Drobniewski F et al. Rifampinand multidrug-resistant tuberculosis in Russian civilians and prison inmates: Dominance of the Beijing strain family. Emerg Infect Dis. 2002;8(11):1320–6.
159.Tanveer M et al. Genotyping and drug resistance patterns of M. tuberculosis strains in Pakistan. BMC Infect Dis. 2008;8:171.
160.Niemann S, Diel R, Khechinashvili G, Gegia M, Mdivani N, and Tang YW. Mycobacterium tuberculosis Beijing lineage favors the spread of multidrug-resistant tuberculosis in the Republic of Georgia. J Clin Microbiol. 2010;48(10):3544–50.
161.Kubica T et al. The Beijing genotype is a major cause of drugresistant tuberculosis in Kazakhstan. Int J Tuberc Lung Dis. 2005;9(6):646–53.
162.Sun YJ et al. Genotype and phenotype relationships and transmission analysis of drug-resistant tuberculosis in Singapore. Int J Tuberc Lung Dis. 2007;11(4):436–42.
163.Werngren J, and Hoffner SE. Drug-susceptible Mycobacterium tuberculosis Beijing genotype does not develop mutation-con- ferred resistance to rifampin at an elevated rate. J Clin Microbiol. 2003;41(4):1520–4.
164.Cowley D et al. Recent and rapid emergence of W-Beijing strains of Mycobacterium tuberculosis in Cape Town, South Africa. Clin Infect Dis. 2008;47(10):1252–9.
165.Interrante JD, Haddad MB, Kim L, and Gandhi NR. Exogenous reinfection as a cause of late recurrent tuberculosis in the United States. Ann Am Thorac Soc. 2015;12(11):1619–26.
166.Kim L, Moonan PK, Yelk Woodruff RS, Kammerer JS, and Haddad MB. Epidemiology of recurrent tuberculosis in the United States, 1993–2010. Int J Tuberc Lung Dis. 2013;17(3):357–60.
167.Nunn AJ, Phillips PP, and Mitchison DA. Timing of relapse in short-course chemotherapy trials for tuberculosis. Int J Tuberc Lung Dis. 2010;14(2):241–2.
168.Kim L, Moonan PK, Heilig CM, Yelk Woodruff RS, Kammerer JS, and Haddad MB. Factors associated with recurrent tuberculosis more than 12 months after treatment completion. Int J Tuberc Lung Dis. 2016;20(1):49–56.
169.Cohen T et al. Multiple introductions of multidrug-resistant tuberculosis into households, Lima, Peru. Emerg Infect Dis. 2011;17(6):969–75.
170.Sonnenberg P, Murray J, Glynn JR, Shearer S, Kambashi B, and Godfrey-Faussett P. HIV-1 and recurrence, relapse, and reinfection of tuberculosis after cure: A cohort study in South African mineworkers. Lancet. 2001;358(9294):1687–93.
171.van Rie A et al. Exogenous reinfection as a cause of recurrent tuberculosis after curative treatment. N Engl J Med. 1999;341(16):1174–9.
172.Verver S et al. Rate of reinfection tuberculosis after successful treatment is higher than rate of new tuberculosis. Am J Respir Crit Care Med. 2005;171(12):1430–5.
173.Bryant JM et al. Whole-genome sequencing to establish relapse or re-infection with Mycobacterium tuberculosis: A retrospective observational study. Lancet Respir Med. 2013;1(10):786–92.
174.Witney AA et al. Use of whole-genome sequencing to distinguish relapse from reinfection in a completed tuberculosis clinical trial. BMC Med. 2017;15(1):71.
175.Guerra-Assuncao JA et al. Recurrence due to relapse or reinfection with Mycobacterium tuberculosis: A whole-genome sequencing approach in a large, population-based cohort with a high HIV infec- tionprevalenceandactivefollow-up.J Infect Dis.2015;211(7):1154–63.
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

References 95
176.Korhonen V, Soini H, Vasankari T, Ollgren J, Smit PW, and Ruutu P. Recurrent tuberculosis in Finland 1995–2013: A clinical and epidemiological cohort study. BMC Infect Dis. 2017;17(1):721.
177.Parvaresh L, Crighton T, Martinez E, Bustamante A, Chen S, and Sintchenko V. Recurrence of tuberculosis in a low-incidence setting: A retrospective cross-sectional study augmented by whole genome sequencing. BMC Infect Dis. 2018;18(1):265.
178.Benator D et al. Rifapentine and isoniazid once a week versus rifampicin and isoniazid twice a week for treatment of drug-sus- ceptible pulmonary tuberculosis in HIV-negative patients: A randomised clinical trial. Lancet. 2002;360(9332):528–34.
179.Romanowski K et al. Predicting tuberculosis relapse in patients treated with the standard 6-month regimen: An individual patient data meta-analysis. Thorax. 2019;74(3):291–7.
180.Huyen MN et al. Mixed tuberculosis infections in rural South Vietnam. J Clin Microbiol. 2012;50(5):1586–92.
181.Garcia de Viedma D, Marin M, Ruiz Serrano MJ, Alcala L, and Bouza E. Polyclonal and compartmentalized infection by Mycobacterium tuberculosis in patients with both respiratory and extrarespiratory involvement. J Infect Dis. 2003;187(4):695–9.
182.Kaplan G et al. Mycobacterium tuberculosis growth at the cavity surface: A microenvironment with failed immunity. Infect Immun. 2003;71(12):7099–108.
183.Baldeviano-Vidalon GC, Quispe-Torres N, Bonilla-Asalde C, Gastiaburu-Rodriguez D, Pro-Cuba JE, and Llanos-Zavalaga F. Multiple infection with resistant and sensitive M. tuberculosis strains during treatment of pulmonary tuberculosis patients. Int J Tuberc Lung Dis. 2005;9(10):1155–60.
184.Das S et al. Simultaneous infection with multiple strains of Mycobacterium tuberculosis identified by restriction fragment length polymorphism analysis. Int J Tuberc Lung Dis. 2004;8(2):267–70.
185. Fang R et al. Mixed infections of Mycobacterium tuberculosis in tuberculosis patients in Shanghai, China. Tuberculosis. 2008;88(5):469–73.
186.Lazzarini LC et al. Discovery of a novel Mycobacterium tuberculosis lineage that is a major cause of tuberculosis in Rio de Janeiro, Brazil. J Clin Microbiol. 2007;45(12):3891–902.
187.Richardson M et al. Multiple Mycobacterium tuberculosis strains in early cultures from patients in a high-incidence community setting. J Clin Microbiol. 2002;40(8):2750–4.
188.Shamputa IC et al. Genotypic and phenotypic heterogeneity among Mycobacterium tuberculosis isolates from pulmonary tuberculosis patients. J Clin Microbiol. 2004;42(12):5528–36.
189.Stavrum R et al. High diversity of Mycobacterium tuberculosis genotypes in South Africa and preponderance of mixed infections among ST53 isolates. J Clin Microbiol. 2009;47(6):1848–56.
190.Warren RM et al. Patients with active tuberculosis often have different strains in the same sputum specimen. Am J Respir Crit Care Med. 2004;169(5):610–4.
191.Yeh RW, Hopewell PC, and Daley CL. Simultaneous infection with two strains of Mycobacterium tuberculosis identified by restriction
fragment length polymorphism analysis. Int J Tuberc Lung Dis. 1999;3(6):537–9.
192.Cohen T et al. Within-host heterogeneity of Mycobacterium tuberculosis infection is associated with poor early treatment response: A prospective Cohort Study. J Infect Dis. 2016;213(11):1796–9.
193.van Rie A et al. Reinfection and mixed infection cause changing
Mycobacterium tuberculosis drug-resistance patterns. Am J Respir Crit Care Med. 2005;172(5):636–42.
194.Theisen A et al. Mixed-strain infection with a drug-sensitive and multidrug-resistant strain of Mycobacterium tuberculosis. Lancet. 1995;345(8963):1512.
195.Niemann S, Richter E, Rusch-Gerdes S, Schlaak M, and Greinert U. Double infection with a resistant and a multidrug-resistant strain of Mycobacterium tuberculosis. Emerg Infect Dis. 2000;6(5):548–51.
196.Bauer J, Thomsen VO, Poulsen S, and Andersen AB. False-positive results from cultures of Mycobacterium tuberculosis due to laboratory cross-contamination confirmed by restriction fragment length polymorphism. J Clin Microbiol. 1997;35(4):988–91.
197.Bhattacharya M et al. Cross-contamination of specimens with Mycobacterium tuberculosis: Clinical significance, causes, and prevention. Am J Clin Pathol. 1998;109(3):324–30.
198.Braden CR, Templeton GL, Stead WW, Bates JH, Cave MD, and Valway SE. Retrospective detection of laboratory cross-contam- ination of Mycobacterium tuberculosis cultures with use of DNA fingerprint analysis. Clin Infect Dis. 1997;24(1):35–40.
199.Frieden TR, Woodley CL, Crawford JT, Lew D, and Dooley SM. The molecular epidemiology of tuberculosis in New York City: The importance of nosocomial transmission and laboratory error. Tuber Lung Dis. 1996;77(5):407–13.
200.Jasmer RM et al. A prospective, multicenter study of laboratory cross-contamination of Mycobacterium tuberculosis cultures. Emerg Infect Dis. 2002;8(11):1260–3.
201.Small PM, McClenny NB, Singh SP, Schoolnik GK, Tompkins LS, and Mickelsen PA. Molecular strain typing of Mycobacterium tuberculosis to confirm cross-contamination in the mycobacteriology laboratory and modification of procedures to minimize occurrence of false-positive cultures. J Clin Microbiol. 1993;31(7):1677–82.
202.Ruddy M et al. Estimation of the rate of unrecognized cross-con- tamination with Mycobacterium tuberculosis in London microbiology laboratories. J Clin Microbiol. 2002;40(11):4100–4.
203.Lai CC et al. Molecular evidence of false-positive cultures for Mycobacterium tuberculosis in a Taiwanese hospital with a high incidence of TB. Chest. 2010;137(5):1065–70.
204.Burman WJ, and Reves RR. Review of false-positive cultures for Mycobacterium tuberculosis and recommendations for avoiding unnecessary treatment. Clin Infect Dis. 2000;31(6):1390–5.
205.Northrup JM et al. Estimated costs of false laboratory diagnoses of tuberculosis in three patients. Emerg Infect Dis. 2002;8(11):1264–70.
206.Lee MR et al. Epidemiologic surveillance to detect false-positive
Mycobacterium tuberculosis cultures. Diagn Microbiol Infect Dis. 2012;73(4):343–9.

Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/

6
Tuberculosis Transmission Control
EDWARD A. NARDELL
Introduction |
97 |
Interventions |
103 |
FAST: Find cases Actively, Separate, and Treat effectively based on rapid molecular diagnostic testing |
104 |
Environmental factors |
105 |
Environmental control interventions |
105 |
Respiratory protection, respirators and surgical masks |
108 |
More comprehensive, evidence-based guidelines |
109 |
Treatment of latent TB in healthcare workers |
109 |
References |
109 |
INTRODUCTION
Globally, in high burden settings, recent transmission, including reinfection, accounts for most incident TB clinical cases, compared to reactivation of remote latent infection.1 Ongoing transmission, therefore, especially in congregate settings, is driving the TB epidemic.2 In low-burden settings, however, where transmission is infrequent, reactivation of latent infection is relatively more important, and treatment of latent infection has been a strategy for TB elimination.3 Even under low-burden settings, it is argued, most disease results within a year or so of transmission, and the risk from old infection may be overestimated.1
Importance of the undiagnosed case or undiagnosed drug resistance
This chapter will review current understanding on Mycobacterium tuberculosis (Mtb) transmission and its control, with emphasis on the importance of transmission from persons with unsuspected TB, or unsuspected drug resistance, not on effective therapy.5 Although effective therapy has long been known to rapidly stop transmission, conventional TB infection control efforts tend to focus on known TB patients, most of whom are on effective therapy and not likely to be sources of transmission.6,7 Guidelines and practice need to shift from a focus on known cases started on effective therapy to finding unsuspected cases in congregate settings through screening, followed by rapid molecular diagnosis and drug susceptibility testing, leading to prompt, effective treatment.8 This re-focused, intensified administrative approach to TB transmission control has been packaged as an easy-to-remember
acronym, “F-A-S-T,” Find cases Actively, Separate temporarily, and Treat effectively, based on molecular drug susceptibility testing.8 The acronym emphasizes the need to reduce time from symptom reporting to effective treatment. In crowded congregate settings, however, such as registration areas and ambulatory clinics, effective screening for unsuspected TB may not be feasible. There, administrative measures (triage, appointments) to reduce crowding, and air disinfection through natural ventilation and upper room germicidal lamps are important interventions.9,10 Likewise, respiratory protection for healthcare workers is less important for encounters with known TB patients on effective treatment—where they are most commonly used—and more likely to be effective for encounters with patients at high risk for undiagnosed TB or undiagnosed drug resistance.11 Good examples are caring for patients with undiagnosed respiratory infection in the emergency room, or patients undergoing bronchoscopy for lung infiltrates where TB is prevalent.
Airborne spread
TB pathogenesis begins through person-to-person transmission, almost exclusively by the airborne route, a relatively unusual transmission route among human pathogens, shared primarily with some respiratory viruses.12 Airborne Mtb infection requires host susceptibility to the extremely small dose of Mtb, carried as droplet nuclei (the 1–5 µm dried residua of larger droplets) able to traverse the structural barriers of the upper respiratory track to reach the peripheral lung where pulmonary alveolar macrophages (PAMs) reside.13 PAMs are both a first line of innate immunity and, paradoxically, the target cell for initial Mtb replication. To accomplish this, Mtb has evolved specific mechanisms for blocking PAM
97

98 Tuberculosis Transmission Control
intracellular killing. Airborne transport is probably facilitated by Mtb’s uniquely thick, hydrophobic cell wall, able to protect this preferentially intracellular pathogen from the stresses of aerosolization, dehydration in room air, transport, and rehydration in the humid respiratory track of a new host.14 Barer has described a “fat and lazy” spore-like phenotype that may be preparatory to aerosolization.15 Exactly what microbial gene-expression signatures are necessary to facilitate airborne transport remain largely unknown, but may be important to elucidate. For example, the rapid impact of effective treatment on transmission, discussed later in this chapter, well before sputum smear and culture conversion, might be due to pharmacologic interference with specific microbial adaptive mechanisms.16
Particles small enough to be inhaled deep into the lung settle very slowly in still air and can remain suspended indefinitely in occupied rooms where air is rarely stagnant due to body heat, air infiltration, and other factors.17 The 1–5 µm size of infectious droplet nuclei is defined not by organism size (0.5 × 1.0 µm), per se, but by the size of the entire particle containing one, or at most several (estimated 2–3) Mtb organisms, but also dried solute, mucous, and cellular debris found in respiratory lining liquid.18 High airflow in the relatively narrow upper airways and trachea, generated by cough and other forced respiratory maneuvers, shears off relatively large droplets that evaporate rapidly into droplet nuclei once expelled, depending on fluid viscoelasticity and ambient humidity.17 Thinner lung lining fluid may be easier to aerosolize than viscous sputum. Quiet breathing can also generate droplet nuclei as alveoli pop open with inhalation, but the contribution of this mechanism to TB transmission is unknown.19 A hallmark of chronic TB disease is lung cavitation, the result of caseation necrosis of a granuloma and erosion into an airway. With cavities containing an estimated 108 Mtb organisms, expectorated sputum may contain tens of thousands of detectable Mtb organisms per cubic millilitre in various states of viability and infectiousness. Aerosolization by cough and other respiratory maneuvers into room air results in a variety of respiratory droplets and droplet nuclei—the majority of which, it is believed, contain damaged, dead, or dying organisms, including microbial fragments of DNA from Mtb, other microorganisms, and respiratory lining cells. Molecular testing of ambient air samples in an unventilated small chamber occupied by an infectious TB patient reveal orders of magnitude more Mtb DNA copies than the estimated numbers of viable, infectious droplet nuclei that actually reach the alveolus and result in sustained infection.20,21 Thus, there is a steep cascade from large numbers of particles generated, many of which are dead or dying, to fewer and fewer particles that reach the distal lung and remain both viable and infectious—and succeed in causing a sustained infection.20
Unable to define the exact number of infectious droplet nuclei that must be inhaled to result in infection in a host, Wells applied the word “quanta,” a general term referring to the smallest amount of almost anything—in this case, the smallest infectious dose. For an individual infection, the lowest infectious dose (or quanta) of Mtb, cannot be less than one intact, viable, infectious Mtb organism, but nor can it be more than can be associated with a single airborne infectious droplet nucleus. Unlike multifocal pointsource histoplasmosis infection, for example, initial (primary)
TB infection in humans (and naturally infected experimental animals) is rarely more than a single lung focus—usually in better ventilated dependent (lower) regions of lungs. This strongly implies a single infectious droplet nucleus. By definition, the clinical foci of infection recognized by x-ray or at autopsy likely represent only the successful host−pathogen interactions from the pathogen perspective, leading to persistent infection manifest by detectable adaptive inflammatory responses. Unknown are the number of host−pathogen interactions that occurred where the host (i.e., macrophage) wins the initial encounter, resulting in complete microbial clearance, leaving little or no measurable evidence (by current methods) of infection or an innate immune response, much less any evidence of any aborted adaptive immune responses.22,23
Understanding that inhaling particles is probabilistic, Wells introduced Poisson’s law of small chances and defined a “quanta” of TB infection on a population basis—the average dose necessary to infect 63% of a population—the remaining exposed susceptible hosts escaping infection by chance. The estimated source strength from human outbreaks and human-to-guinea-pig experiments (see subsection “Source factors” and Figure 6.8), ranges from 1.25 infectious quanta per hour (qph), to 13 qph for an infectious office worker, to 60 qph for a case of laryngeal TB, and approximately 250 qph for a bronchoscopy-related TB case.24–26
Room air concentrations of infectious quanta vary with dilution of in-room volume, and from ventilation and die-off over time, but estimates from Riley’s classic 2-year human-to-guinea- pig transmission study are as low as 1 infectious quanta in 11,000 ft3 (311 m3) of air.27,28 These low levels of contagion, however, were sufficient to explain the rate at which student nurses became infected on hospital TB wards in the pre-chemotherapy era.29 The more infectious a particular airborne pathogen for a particular host, the less role chance plays, for example, initial measles exposure almost always results in human infection.
Measuring infectiousness
TB is routinely diagnosed in sputum by smear microscopy, culture, and by molecular detection of Mtb. Smear microscopy will detect about half of the organisms that will grow in sputum culture—and the newest molecular methods detect about the same as does liquid culture. However, it has not been possible to grow Mtb sampled from ambient room air on selective media due to overwhelming numbers of fast-growing competing environmental organisms. As noted previously, while molecular methods can detect nucleic acids, their viability and infectivity remain unknown. Coughing into a sterilized air-sampling cylinder, directly onto agar surfaces or into liquid media (cough aerosol sampling system, CASS), incorporating the host’s ability to cough and generate aerosol, has allowed source strength quantification that has been shown to correlate better with household Mtb spread than does sputum smear or culture alone.30 Because it is technically challenging, CASS remains a research tool. In low burden settings, accurate estimates of infectiousness of a source case requires testing human contacts for infection by tuberculin skin testing or IGRA. Under high-burden settings, however, pre-existing tuberculin hypersensitivity from vaccination or previous mycobacterial infection limits the utility of contact tracing.
Книга в списке рекомендаций к покупке и прочтению сайта https://meduniver.com/
Introduction 99
Because of far fewer variables, for research purposes, the gold standard method for measuring human infectiousness remains quantitative animal studies, where hundreds of highly vulnerable guinea pigs breath the exhaust air from an experimental TB ward and are tested monthly for new infection.22,26,31
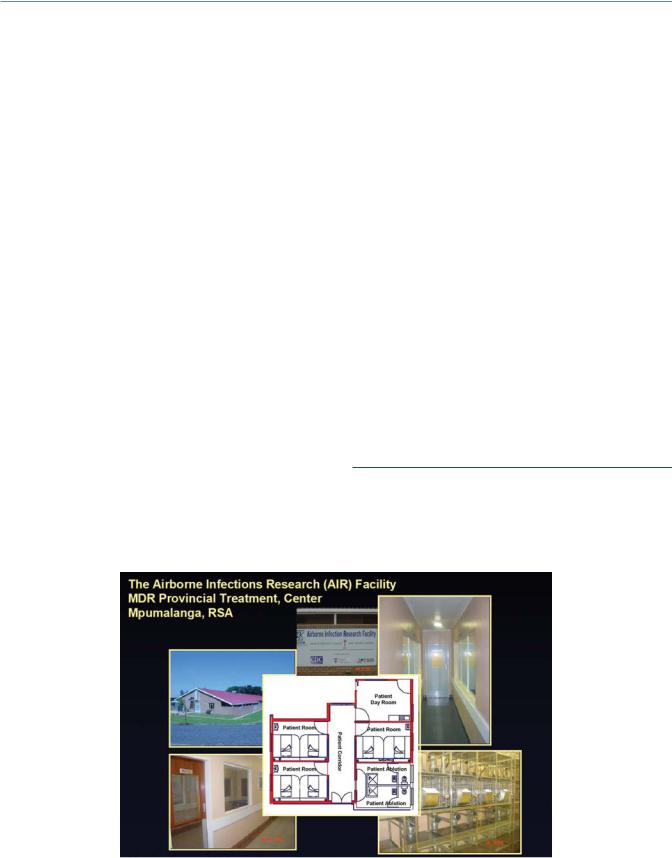
Although human-to-animal transmission experiments go back to the late nineteenth century, the first quantitative human- to-guinea-pig (H-GP) transmission study, envisioned by Wells and conducted by Riley in the late 1950s and the early 1960s, proved beyond doubt that Mtb was routinely spread via the air, that patients varied greatly from one another in infectiousness, and that effective treatment had an immediate and profound impact on transmission.26 More recently, Escombe conducted similar studies in Peru, focused on an HIV co-infected patient population, and proved the effectiveness of upper room germicidal UV (GUV) air disinfection (see Figure 6.1 and subsection “Upper room GUV”).32 In South Africa, Nardell, Stoltz, and colleagues have used the same model for more than 14 years (Figure 6.1)—major findings include the rapid impact of effective treatment, and new regimens, on transmission of multi-drug resistant (MDR)/extensively drug-resistant (XDR)-TB, the effectiveness of surgical masks on patients, the effectiveness of upper room GUV air disinfection (with dosing specifications), the ineffectiveness of selected room air cleaning (filtration) devices, and importantly, new insights into the early events of infection in the guinea-pig model, demonstrating frequent transient infections, with spontaneous clearance, as well as reinfection. These findings are discussed further, below.6,22,33,34
TB primary infection (and reinfection), as noted above, follows inhalation of viable and infectious Mtb-containing droplet nuclei small enough (1–5 µm) to reach and impact surfaces in the peripheral lung patrolled by alveolar macrophages.13 Macrophage recognition and phagocytosis of Mtb triggers a series of host innate and metabolic defense mechanisms aimed at killing the microbe at
that stage, and initiating specific adaptive immunity, should it be necessary. But phagocytosis of Mtb also triggers a series of microbial virulence factors intended to evade host defenses (see subsections “Infection: Transient and sustained” and “Host factors”) and, indeed, to allow the organisms to replicate rather than die within and, ultimately, outside of host cells.13 Stimulation of intracellular macrophage signaling also impacts the cytokine environment thereby modifying the strength of adaptive immunity, leading to Mtb survival and tolerance (granuloma formation, necrosis, latency) over time. Thus, the early innate host responses to Mtb are essential for preventing sustained TB infection as well as for developing effective adaptive immunity should infection persist.23,35
Development of active (clinical) TB, therefore, represents a failure of host defenses at several levels, but critically, failure of the earliest response to prevent sustained infection from relatively rare, individual Mtb-containing droplet nuclei. Given the natural variability in host innate immunity and microbial virulence, a spectrum of host−pathogen outcomes is inevitable, but poorly documented for TB. Not well described in the literature, transient TB infection occurs—the best documented example of which— albeit not usually resolved at the earliest stage of infection due to an extremely large microbial dose—is BCG vaccination, where despite clear evidence of local response to live bacteria at the injection site, measurable systemic hypersensitivity is almost always transient (months to many years) following complete clearance of this attenuated strain.36
Infection: Transient and sustained
Despite a clear understanding that initial TB infection entails innate immune responses to one or, at most, several viable Mtb organisms able to reach the alveoli in a single focus, most experimental laboratory aerosol challenge models employ brief (10–20 min) exposures to 10–50 CFUs of cultured organisms to assure infection
Figure 6.1 The AIR Facility, Mpumalanga, South Africa, has been a collaboration of several US and South African institutions, with funding from NIOSH, USAID, NIH, and the Bill and Melinda Gates Foundation. Clockwise from the photo of the signage, the images show the two identical guinea-pig exposure chambers, the cages in one exposure chamber, one of three patient 2-bed rooms, and the outside of the facility. In the center is a schematic of the patient suite. Air is sampled from the three patient rooms, the corridor, and the patient day room.
