
- •Dedication
- •Preface
- •Acknowledgments
- •Figure Credits
- •Expert Consultants and Reviewers
- •Contents
- •Descriptive Terms for Normal Cells
- •Descriptive Terms for Abnormal Cells and Tissues
- •Epithelium
- •Glands
- •Introduction and Key Concepts for Connective Tissue
- •Cartilage
- •Bone
- •Introduction and Key Concepts for the Nervous System
- •Peripheral Blood Cells
- •Hemopoiesis
- •Introduction and Key Concepts for the Circulatory System
- •The Cardiovascular System
- •Introduction and Key Concepts for the Lymphoid System
- •Cells in the Lymphoid System
- •Introduction and Key Concepts for the Respiratory System
- •Conducting Portion
- •Respiratory Portion
- •Introduction and Key Concepts for the Urinary System
- •Introduction and Key Concepts for the Integumentary System
- •Oral Mucosa
- •Teeth
- •Introduction and Key Concepts for the Digestive Tract
- •Introduction and Key Concepts for the Endocrine System
- •Introduction and Key Concepts for the Male Reproductive System
- •Introduction and Key Concepts for the Female Reproductive System
- •Introduction and Key Concepts for the Eye
- •Introduction and Key Concepts for the Ear
- •Introduction
- •Preservation versus Fixation
- •Fixatives and Methods of Fixation
- •Sectioning and Mounting
- •Staining
- •Index

324 UNIT 3 ■ Organ Systems
Figure 17-11B |
Clinical Correlation: Pheochromocytoma |
Figure 17-12A |
Adrenal Medulla |
Figure 17-12B |
Cells of the Adrenal Medulla |
Pineal Gland |
|
Figure 17-13A |
Overview of the Pineal Gland |
Figure 17-13B |
Pinealocytes and Brain Sand of the Pineal Gland |
Figure 17-13C |
Clinical Correlation: Pineoblastoma |
Endocrine Pancreas |
|
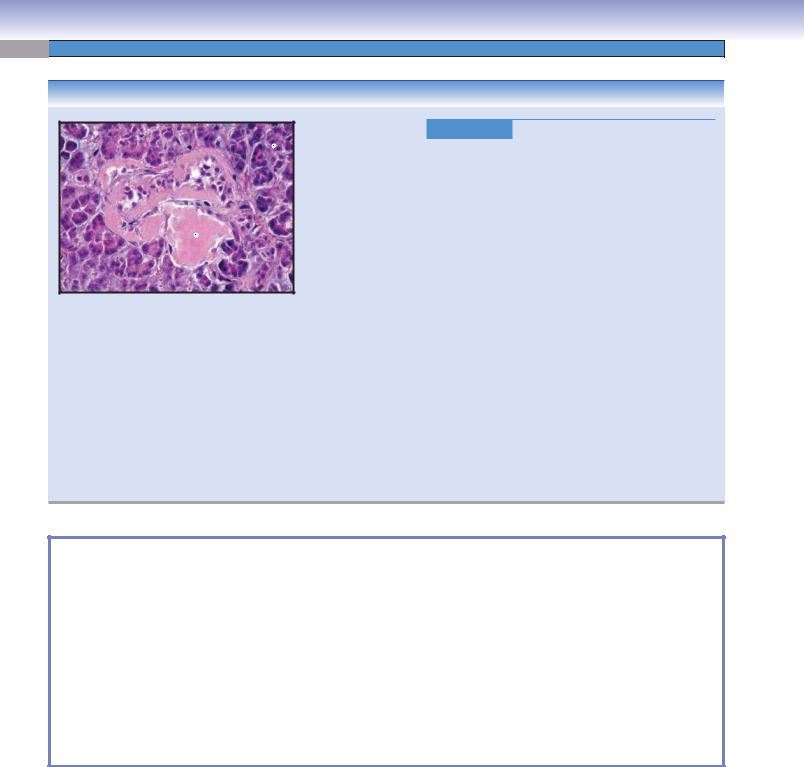
Figure 17-14A,B |
Islets of Langerhans, Endocrine Pancreas |
Figure 17-15A,B |
Pancreatic Islet Cells, Islets of Langerhans |
Figure 17-16 |
Clinical Correlation: Type 2 Diabetes Mellitus |
Synopsis 17-1 |
Pathological Terms for the Endocrine System |
Table 17-1 |
Endocrine Organs |
Introduction and Key Concepts for the Endocrine System
The endocrine system is very closely associated with the nervous system and is much like the nervous system in some ways. The nervous system sends messages related to sensation, thought, and motor control using electrochemical signals (action potentials) that are carried by neurons and axons. The endocrine system sends messages to control and regulate the metabolic activity of the body using chemical signals (hormones) that are released by endocrine secretory cells and carried by the blood circulatory system. The endocrine system includes (1) endocrine glands, such as the pituitary gland, thyroid and parathyroid glands, adrenal glands, and the pineal gland; (2) clusters of endocrine cells located in the organs such as islets of Langerhans in the pancreas; and (3) isolated endocrine cells in certain tissues, such as the enteroendocrine cells in the epithelium of the respiratory and digestive tracts (see Chapters 11, “Respiratory System,” and 15, “Digestive Tract”). The endocrine organs that are discussed in this chapter include the pituitary gland, parathyroid glands, adrenal glands, and the endocrine pancreas (islets of Langerhans). Other endocrine organs, such as the testes and ovaries, are discussed in Chapters 18, “Male Reproductive System,” and 19, “Female Reproductive System.”
Endocrine secretions (hormones) are delivered through the capillary network of the vascular system to the target organs rather than through a series of ducts as in the exocrine system. The timing of hormone release is controlled by the hypothalamus. The hypothalamus acts as a command center, controlling the activity of the pituitary gland. The pituitary gland functions as a master gland, releasing hormones to control other endocrine glands and organs. The organs or tissues that are activated by released hormones are called target organs or tissues. The cells in the target organ/tissue have appropriate
receptors, which are able to recognize and respond to specific hormones (Fig. 17-2).
The hormones can be divided into three classes based on their structure:
1.Steroid hormones are lipid hormones that have the characteristic ring structure of steroids (terpenoid lipids) and are formed from cholesterol. Examples of these hormones include estrogen, testosterone, cortisone, and aldosterone.
2.Peptide hormones are composed of amino acids and are usually produced by the partial hydrolysis of proteins. The majority of hormones of this type are secreted by the pituitary gland (e.g., adrenocorticotropic hormone [ACTH], thyroidstimulating hormone [TSH], follicle-stimulating hormone [FSH], prolactin, and growth hormones) and parathyroid glands (parathyroid hormone [PTH], or parathormone).
3.Amine hormones are derived from the amino acid tyrosine.
Examples include triiodothyronine (T3) and thyroxine (T4) released by the thyroid and sympathomimetic hormones (adrenaline/epinephrine and noradrenaline/norepinephrine) secreted by the adrenal medulla.
Pituitary Gland
The pituitary gland is a neuroendocrine organ located inside the skull and considered a part of the brain (Figs. 17-2 to 17-6B). It consists of two divisions: the adenohypophysis (anterior lobe) and the neurohypophysis (posterior lobe). The pituitary gland produces various types of hormones that act on many target organs, many of which also secrete hormones (Fig. 17-2). Secretion of the pituitary gland is controlled and regulated by releasing hormone and inhibitory hormone secreted by the hypothalamus or by nervous system signals from the hypothalamic nuclei, including the paraventricular nuclei, the supraoptic

CHAPTER 17 ■ Endocrine System |
325 |
nuclei, and the arcuate nuclei. The hypothalamus itself receives signals from many areas of the brain, including the amygdala, hippocampus, brainstem tegmentum, and the infralimbic and cingulate cortices. The hypothalamus maintains body homoeostasis by regulating production of the hypothalamic hormones, which, in turn, control the secretion of the pituitary hormones from the pituitary gland.
THE ADENOHYPOPHYSIS, also called the anterior pituitary, is the anterior division of the gland and is derived from the ectoderm of the roof of the developing oral cavity (Rathke pouch). It is composed of glandular tissue. The adenohypophysis can be divided into three regions based on their anatomic positions: the pars distalis, pars tuberalis, and pars intermedia.
1.The pars distalis is the main body of the adenohypophysis, containing blood vessels, a capillary network, and two main types of secretory cells supported by a network of reticular connective tissues. These secretory cells are classified as chromophobes and chromophils. The chromophobes do not effectively take a stain, so they appear clear in the Mallory trichrome stain. These cells are undifferentiated cells but are capable of differentiating into chromophils. The chromophils include basophils and acidophils (Fig. 17-4A).
Basophils appear blue in Mallory stain and include three subtypes of hormone secretory cells: corticotrophs, thyrotrophs, and gonadotrophs. Various hormones are produced by these cells, including ACTH, TSH, FSH, and luteinizing hormone
(LH). These hormones stimulate various target organs including the cortex of the adrenal glands, the thyroid, the testes, and the ovaries (see Fig. 17-2 for details). The secretion of hormones by cells in the adenohypophysis is controlled by hypothalamic releasing hormones and inhibitory hormones. Corticotrophs are stimulated by corticotropin-releasing hormone (CRH) from the hypothalamus. Thyrotrophs are stimulated by thy- rotropin-releasing hormone. Gonadotrophs are stimulated by gonadotropin-releasing hormone.
Acidophils appear red in Mallory stain and contain two subtypes of hormone secretory cells: somatotrophs and mammotrophs. Somatotrophs secrete somatotropin (growth hormone), which stimulates the liver to produce the insulin-like growth factor (IGF-1) that promotes cartilage and bone growth, protein deposition, and cell reproduction. Mammotrophs secrete prolactin, which increases mammary gland size and promotes milk production.
2.The pars tuberalis is the neck of the adenohypophysis; it wraps around the infundibular stalk of the pituitary gland (Fig. 17-3A). It contains a rich capillary network and some low columnar basophilic cells that are commonly arranged in cords.
3.The pars intermedia is located between the pars distalis and pars nervosa (Figs. 17-3A and 17-5A). It contains cuboidal follicular cells and colloid cysts called Rathke cysts, which are lined by follicular cells. Rathke cysts are derived from the ectoderm of the dorsal portion of the Rathke pouch;
these cysts are considered to be the remnants of the Rathke pouch that was present during development. The secretory cells may be involved in producing melanocyte-stimulating hormone (MSH). These cells are usually lightly stained by basophilic dye.
THE NEUROHYPOPHYSIS is derived from the inferior surface of the developing diencephalon. It is considered to be nervous tissue. It can be divided into the infundibular stalk, the median eminence, and the pars nervosa.
1.The infundibular stalk connects the median eminence to the pars nervosa (Fig. 17-3A,B).
2.The median eminence connects the inferior portion of the hypothalamus to the infundibular stalk of the neurohypophysis (Fig. 17-3B). It contains long axons that carry antidiuretic hormone (ADH) and oxytocin hormone produced by nuclei in the hypothalamus. These axons pass through the median eminence and terminate in the pars nervosa. The median eminence also contains short axons and axon terminal endings from the hypothalamus that release neurosecretory hormones (hypothalamic releasing and inhibiting hormones). These hormones are transported through the hypophyseal portal system from the primary capillary plexus to the secondary capillary plexus, thereby regulating the secretion of the secretory cells in the adenohypophysis.
3.The pars nervosa is the main body of the neurohypophysis (Figs. 17-3A and 17-6A,B). It contains a fenestrated capillary plexus, pituicytes (glial cells), and axons and axon terminal endings from neuron cell bodies in the hypothalamus. Pituicytes provide support and nutrition to the axons of the neurons. The enlarged axon terminal endings are filled with neurosecretory granules that are called Herring bodies. The neurosecretory hormones released in the pars nervosa include ADH or vasopressin, oxytocin hormone, and neurophysins.
Thyroid Gland
The thyroid gland has two lobes that are located inferior to the thyroid cartilage and anterior to the trachea. It contains thyroid follicles that produce T3 and T4, which regulate body metabolism (Fig. 17-8A,B). The parafollicular cells located between the follicles are known as clear cells (C cells) and produce calcitonin hormone. This hormone is released in response to high blood calcium and inhibits the activity of the osteoclasts. Calcitonin is involved in calcium and phosphorus metabolism. It decreases blood calcium levels and has opposing effects to the parathormone or PTH.
Parathyroid Glands
There are typically four small parathyroid glands, most commonly lying posterior to the thyroid gland. They consist of chief cells and oxyphil cells (Fig. 17-9A,B). Chief cells are hormoneproducing cells that secrete parathormone, also called PTH. PTH is released in response to low blood calcium levels and indirectly promotes the proliferation and activity of osteoclasts, which remove bone. PTH also inhibits the activity of osteoblasts, which help to build up new bone.

326 |
UNIT 3 ■ |
Organ Systems |
|
|
|
|
|
|
PTH indirectly promotes osteoclasts by stimulating |
Pineal Gland |
|||||
|
osteoblasts |
to produce osteoclast differentiation |
factor, also |
The pineal gland is located inside the skull and lies above the |
|||
|
known as |
RANKL, |
which |
stimulates |
precursors |
(monocytes) |
|
|
superior colliculi of the midbrain. It is considered part of the |
||||||
|
to differentiate and |
fuse to |
become |
multinuclear |
osteoclasts. |
||
|
epithalamus of the brain. It contains pinealocytes, neuroglial |
||||||
|
Increased numbers of osteoclasts cause active bone resorption, |
||||||
|
cells, and calcified structures called brain sand (corpora |
||||||
|
which results in more Ca++ being released into the blood. PTH |
||||||
|
arenacea). The corpora arenacea are derived from the organic |
||||||
|
also affects the distal tubules of the kidney to increase blood cal- |
||||||
|
matter in the pineal gland and are rich in calcium and phos- |
||||||
|
cium levels by enhancing the reabsorption of calcium from distal |
||||||
|
phate. The pineal gland has a rich blood supply. Pinealocytes, |
||||||
|
tubules. |
|
|
|
|
|
|
|
|
|
|
|
|
modified neurons that produce melatonin, are the predominant |
|
|
|
|
|
|
|
|
|
|
Adrenal Glands |
|
|
|
|
cells in the pineal gland. Melatonin is an important hormone |
|
|
|
|
|
|
in the regulation of the day and night cycle called the circadian |
||
|
The adrenal glands lie on the superior tips of the kidneys, in the |
rhythm (Fig. 17-13A,B). |
|||||
|
posterior portion of the abdominal cavity. The adrenal glands can |
|
|||||
|
be divided into the cortex and the medulla (Fig. 17-10A). The cor- |
Endocrine Pancreas (Islets of Langerhans) |
|||||
|
tex has three zones: (moving from external to internal) the zona |
||||||
|
glomerulosa, zona fasciculata, and zona reticularis (Fig. 17-10B). |
There are many islets of Langerhans interspersed in the exocrine |
|||||
|
Cells in the cortex produce various corticosteroid hormones |
portion of the pancreas (Figs. 17-14A to 17-15B). The islets of |
|||||
|
including mineralocorticoids, glucocorticoids, and weak andro- |
Langerhans contain alpha cells, beta cells, delta cells, and pancre- |
|||||
|
gens (see Table 17-1). The medulla contains ganglion neurons and |
atic polypeptide (PP) cells. These hormone secretory cells produce |
|||||
|
chromaffin cells. The chromaffin cells produce adrenaline (epi- |
glucagon, insulin, somatostatin, and PP, important hormones in |
|||||
|
nephrine) and noradrenaline (norepinephrine). These hormones |
regulating blood glucose levels. |
|||||
|
are known as sympathomimetic hormones (Fig. 17-12A,B). |
|
|||||

CHAPTER 17 ■ Endocrine System |
|
|
327 |
|
Hypothalamus |
Pineal |
|
|
|
gland |
|
Fig. 17-3B to |
||
|
|
|||
Pituitary |
|
Pineal |
Fig. 17-6B |
|
|
|
|
||
gland |
|
gland |
Fig. 17-13A,B |
|
|
|
|
||
|
|
|
Fig. 17-8A,B |
|
Thyroid |
|
|
|
|
gland |
Parathyroid |
Fig. 17-9A,B |
||
|
||||
|
gland |
|
|
|
|
(behind thyroid) |
|
|
|
|
|
|
Fig. 17-10A to |
|
Adrenal |
|
|
Fig. 17-12B |
|
|
|
Fig. 17-14A to |
||
gland |
|
|
||
|
Pancreas |
|
Fig. 17-15B |
|
Ovary
Testis 
A B
Figure 17-1. Overview and orientation of detailed endocrine organ illustrations.
The illustration on the left shows the location of the endocrine organs, which include the pituitary gland, pineal gland, thyroid gland, parathyroid glands, adrenal glands, endocrine pancreas (islet of Langerhans), testes (see Chapter 18, “Male Reproductive System”), and ovaries (see Chapter 19, “Female Reproductive System”). The pituitary and pineal glands are neuroendocrine organs; they are located inside the skull and are considered part of the brain. The thyroid gland has two lobes and is located inferior to the thyroid cartilage and anterior to the trachea. There are four parathyroid glands located behind (posterior to) the thyroid gland. The adrenal glands and pancreas are located in the abdominal cavity. The islet of Langerhans is the endocrine portion of the pancreas. The ovaries and testes produce sex-related hormones and also are part of the reproductive system; the details are discussed in Chapters 18 and 19. The illustration on the right shows the orientation of detailed endocrine organ illustrations presented in different figures.
Endocrine Organs with Figure Numbers
Pituitary glands
Figure 17-2
Figure 17-3A
Figure 17-3B
Figure 17-3C
Figure 17-4A
Figure 17-4B
Figure 17-5A
Figure 17-5B
Figure 17-6A
Figure 17-6B
Figure 17-7A–C
Thyroid glands
Figure 17-8A
Figure 17-8B
Figure 17-8C
Parathyroid glands
Figure 17-9A
Figure 17-9B
Figure 17-9C
Adrenal glands
Figure 17-10A
Figure 17-10B
Figure 17-11A
Figure 17-11B
Figure 17-12A
Figure 17-12B
Pineal glands
Figure 17-13A
Figure 17-13B
Figure 17-13C
Endocrine pancreas (islet of Langerhans)
Figure 17-14A
Figure 17-14B
Figure 17-15A
Figure 17-15B
Figure 17-16

328 UNIT 3 ■ Organ Systems
Pituitary Gland
(–)
(–)
Adrenal cortex
Corticosteroids secretion
(salt, sugar, sex)
Thyroid
T3 and T4 secretion (metabolic activity)
ACTH (+) |
|
(corticotrophs) |
|
TSH |
(+) |
|
|
(thyrotrophs) |
|
Testis |
(+) |
|
Secretion by Sertoli cells |
(gonadotrophs) |
|
FSH |
|
|
(spermatogenesis) |
(gonadotrophs) |
|
(follicle growth) |
||
Ovary |
LH |
(+) |
Estrogen |
|
|
secretion |
|
|
Ovary
Progesterone
secretion
(ovulation)
Testis
Secretion of testosterone by Leydig cells
(sex characteristics)
(+) |
(mammotrophs) |
Prolactin |
|
Hypothalamus
Releasing hormones
ADH/vasopressin (+) (from supraoptic nucleus)
Oxytocin (+) (from supraoptic and paraventricular nuclei)
Growth (somatotrophs)somatotrophin hormone/ (+)
Kidney
Water absorption (collecting tubules)
Uterus
Contraction (smooth muscle of myometrium)
Mammary gland
Contraction (myoepithelial cells)
|
Liver |
|
|
Secretion of IGF-1 |
Bone |
|
(somatomedins) |
|
|
(hepatocytes) |
Growth |
|
|
(epiphyseal plate) |
|
|
Muscle |
|
|
Growth |
|
(skeletal muscle) |
|
Mammary gland |
Adipose tissue |
|
Milk secretion |
Utilization for energy |
|
(secretory cells) |
(adipose cells) |
|
Figure 17-2. Overview of hormone regulation by the pituitary gland.
The hormones released by the basophils in the adenohypophysis of the pituitary gland include ACTH, TSH, FSH, and LH. ACTH is synthesized by corticotrophs, which are stimulated by CRH from the hypothalamus. ACTH is synthesized by thyrotrophs, which stimulates the adrenal cortex to produce corticosteroids (glucocorticoids, androgens) and indirectly influences aldosterone. TSH is also synthesized by thyrotrophs; it stimulates production of T3 and T4 by the thyroid. FSH and LH are secreted by gonadotrophs; these hormones promote secondary sex characteristics and stimulate the development of ovarian follicles (ovary) and spermatogonia (testis). The hormones released by acidophils include prolactin and growth hormone. Prolactin is secreted by mammotrophs (lactotrophs) and stimulates the mammary glands to produce milk. The growth hormone (somatotropin) is secreted by somatotrophs; it stimulates the liver to produce IGF-1, also known as somatomedins, which promotes protein deposition, cell reproduction, and cartilage and bone growth and enhances fat utilization for energy by increasing fatty acids in the bloodstream. The hormones released by the neurohypophysis include ADH (or vasopressin) and oxytocin, which are produced by neurons whose cell bodies lie in the hypothalamus. ADH promotes water absorption by collecting tubules and ducts. Oxytocin stimulates contraction of smooth muscle fibers in the myometrium of the uterus.
Pituitary Gland
I.Adenohypophysis (anterior pituitary gland)
A.Pars distalis
1.Chromophobes
2.Chromophils
a.Acidophils: Somatotrophs (secrete growth hormone), mammotrophs/lactotrophs (secrete prolactin)
b.Basophils: Corticotrophs (secrete ACTH), thyrotrophs (secrete TSH), gonadotrophs (secrete FSH and LH)
B.Pars/tuberalis: Gonadotrophs (secrete FSH and LH)
C.Pars intermedia
1.Rathke cysts (colloid-containing cysts)
2.Basophilic cells/melanotrophs (secrete MSH)
II.Neurohypophysis (posterior pituitary gland)
A.Neural (infundibular) stalk
B.Median eminence
C.Pars nervosa
1.Herring bodies (contain neurosecretory granules)
2.Neurohypophyseal hormones: ADH (secreted by neurons whose cell bodies are in the supraoptic nucleus), oxytocin (secreted by neurons whose cell bodies are in both supraoptic and paraventricular nuclei)
Abbreviations
ACTH: Adrenocorticotropic hormone
TSH: Thyroid-stimulating hormone
FSH: Follicle-stimulating hormone
LH: Luteinizing hormone
MSH: Melanocyte-stimulating hormone

CHAPTER 17 ■ Endocrine System |
329 |
|
Optic chiasm |
Optic |
|
chiasm |
Hypothalamus |
|
Pituitary
Pituitary
gland
gland
Pineal
 gland Infundibular stalk
gland Infundibular stalk
Pituitary
gland
A
Figure 17-3A. Overview of the pituitary gland.
The pituitary gland is a small, bean-shaped gland, about 1 cm in diameter, located inferior to the hypothalamus and separated from it by the diaphragma sellae through which the infundibular stalk (infundibulum) passes. The pituitary gland lies within the sella turcica. Various important surrounding structures are visible in the photograph and inset. The pituitary gland is located inferior, and slightly caudal, to the optic chiasm; this is a particularly important anatomical relationship that is applicable to clinical medicine.
A pituitary tumor, as it enlarges, may impinge on the crossing fibers within the optic chiasm, causing visual field deficits. This most commonly results in bitemporal hemianopia, a loss of the temporal visual fields of both eyes. Other visual field deficits can also result from pituitary tumors.
|
Paraventricular |
Hypothalamus |
Arcuate |
Infundibular |
nucleus |
|
nucleus |
stalk |
Supraoptic |
|
Mammillary |
|
|
||
|
nucleus |
|
body |
Hypothalamus |
Median |
|
|
|
eminence |
|
|
Pars |
Optic |
|
|
chiasm |
|
Infundibular |
|
tuberalis |
Pars |
|
|
|
|
stalk |
|
|
tuberalis |
|
Pars |
Pars |
|
|
|
|
|
intermedia |
|
tuberalis |
Basophils |
|
|
|
|
Pars |
Pars |
B distalis |
nervosa |
Acidophils |
Pars |
Pars |
nervosa |
|
|
distalis |
|
Anterior lobe |
Posterior lobe |
Figure 17-3B. Pituitary gland. Mallory trichrome and H&E, 10
The pituitary gland is closely associated with the hypothalamus; it can be divided into two regions based on embryonic origins: the adenohypophysis (anterior pituitary gland) and the neurohypophysis (posterior pituitary gland). The adenohypophysis arises from the ectoderm of the Rathke pouch (roof of the developing oral cavity). It includes the pars distalis, pars tuberalis, and pars intermedia. The neurohypophysis is differentiated from the neural ectoderm of the inferior surface of the developing diencephalon. It includes the median eminence, infundibular stalk, and pars nervosa and contains axons whose cell bodies are located in the hypothalamus.
Capsule
Pars nervosa
Pars distalis
|
Pars |
|
|
Intermedia |
|
C |
||
|
Figure 17-3C. Pituitary gland. Mallory trichrome and H&E, 31
The adenohypophysis (anterior pituitary gland) with its connective tissue capsule is shown on the left of the microphotograph. It stains red-blue because it contains chromophils (acidophils and basophils) and chromophobes. The pars nervosa of the neurohypophysis (posterior pituitary gland) is nervous tissue; it is shown on the right. It contains axons, pituicytes, and capillaries. It stains much lighter than the adenohypophysis. The cell bodies of these axons are located in the supraoptic and paraventricular nuclei of the hypothalamus. These neurons have long axons that extend from the hypothalamus into the neurohypophysis of the pituitary gland. The axons contain neurosecretory granules consisting of two types of hormones: oxytocin (supraoptic and paraventricular nuclei) and ADH (supraoptic nucleus). Enlarged axon terminal endings are known as Herring bodies (Fig. 17-6A,B).

330 UNIT 3 ■ Organ Systems
A |
|
|
Figure 17-4A. |
Pars distalis, adenohypophysis (anterior pitu- |
|
|
|
Basophils |
itary gland). Mallory trichrome and H&E, 281 |
||
|
|
The pars distalis, the largest part of the adenohypophysis, contains |
|||
|
|
|
|||
|
|
|
two major types of cells: chromophobes and chromophils. Chro- |
||
|
|
|
mophobes are so named because the cytoplasm does not absorb |
||
|
|
|
chromium salt stains, whereas the cytoplasm of chromophils does |
||
|
|
|
absorb chromium salts. In a Mallory trichrome–stained specimen, |
||
Chromophobes |
|
the chromophils can be divided into acidophils and basophils accord- |
|||
|
ing to the staining (red or blue, respectively) of the granules in the |
||||
|
|
|
|||
|
|
|
cytoplasm. Overall cell composition is about 50% chromophobes, |
||
|
|
|
15% basophils, and 35% acidophils. Acidophilic granules are char- |
||
|
|
|
acteristic of cells that secrete polypeptide hormones, such as growth |
||
Blood |
|
hormone (somatotrophs) or prolactin (mammotrophs), and baso- |
|||
|
philic granules are characteristic of cells that secrete glycoprotein |
||||
vessel |
Acidophils |
||||
hormones such as TSH (thyrotrophs), LH, and FSH (gonadotrophs). |
|||||
|
|
||||
|
|
|
|||
|
|
|
Corticotrophs, which secrete molecules of the proopiomelanocortin |
||
|
|
|
family, also have basophilic granules. In this photomicrograph, chro- |
||
|
|
|
mophobes have pale cytoplasm, basophils have blue-staining gran- |
||
|
|
|
ules in their cytoplasm, and acidophils have red-staining granules. |
||
|
|
|
|
|
|
B
Basophil Acidophil
Chromophobes
Chromophil (possible corticotroph)
Chromophil (possible somatotroph)
Golgi complex
 Chromophobe
Chromophobe
 Chromophil (possible mammotroph)
Chromophil (possible mammotroph)
Figure 17-4B. Cells in the pars distalis, anterior pituitary gland. EM, ×7,700; inset (color) Mallory trichrome and H&E, 423
The five types of hormone-secreting (chromophil) cells in the anterior pituitary are most reliably identified by immunocytochemistry using antibodies against the specific hormone or hormones that each cell type secretes. However, an expert can also identify cell types on the basis of the size, density, and distribution of secretory granules in transmission electron micrographs. This image has an apparent chromophobe and at least three different types of chromophils. Note the differences in the features of the granules in the three chromophils that have been labeled. Note also that the nuclei of the chromophils have nucleoli and substantial euchromatin, features of cells that are actively synthesizing polypeptides. A moderate amount of rough endoplasmic reticulum (RER) and prominent Golgi complexes can also be seen in the chromophils. The rich capillary bed in the adenohypophysis consists of capillaries that are fenestrated, a feature that allows ready movement of both releasing factors and hormones between the blood plasma and the endocrine cells. The relative proportions of the specific cell types vary significantly according to specific location within the anterior lobe.

CHAPTER 17 ■ Endocrine System |
331 |
A |
Follicular cells |
|
Pars |
|
nervosa |
|
Rathke |
|
cysts |
|
Colloid |
|
Blood vessel |
|
Pars |
Blood cells |
distalis |
|
Figure 17-5A. Pars intermedia, anterior pituitary gland.
Mallory trichrome and H&E, 127
The pars intermedia originates from the ectoderm of the Rathke pouch and is part of the adenohypophysis. This bandlike structure lies between the pars distalis and pars nervosa. It is of the same embryonic origin as the pars distalis. The pars intermedia contains colloid cysts called Rathke cysts, which are lined by cuboidal to columnar follicular cells. These cells are associated with the formation of MSH in the fetus. This photomicrograph shows several colloid-filled cysts (Rathke cysts). Most cells in the pars intermedia resemble basophilic cells (melanotrophs). A blood vessel separates the pars intermedia and the pars distalis.
B |
Hypothalamus |
|
|
|
Median |
|
|
eminence |
Median |
|
|
eminence |
|
Branch of |
|
|
|
Primary |
|
internal |
|
carotid artery |
|
capillary |
|
|
|
|
|
plexus |
|
Superior |
Hypophyseal |
|
|
|
hypophyseal |
|
portal veins |
|
|
|
arteries |
|
|
|
|
Hypophyseal |
|
Trabecular |
|
artery |
|
veins |
|
|
|
|
|
|
|
Hypophyseal |
|
|
vein |
Secondary |
|
|
capillary |
|
Inferior hypophyseal |
plexus |
|
artery |
|
Anterior lobe |
Posterior lobe |
Figure 17-5B. Blood supply of the pituitary gland.
The superior hypophyseal arteries, which arise from the internal carotid artery and posterior communicating artery of the circle of Willis, supply the pars tuberalis, the infundibular (neural) stalk, and the median eminence. The darker shaded area indicates the primary capillary plexus, which receives blood from the superior hypophyseal arteries, drains blood into the hypophyseal portal veins supplying the secondary capillary plexus (white shaded area), and, finally, drains into the hypophyseal veins. Both primary and secondary capillary plexuses contain fenestrated capillaries. The portal blood circulation (from primary to secondary capillary plexuses) carries neurosecretory hormones from the median eminence into the pars distalis where they stimulate or inhibit basophils and acidophils to produce hormones. The pars nervosa receives blood mainly from the inferior hypophyseal arteries, which arise from the internal carotid artery. This artery also receives blood from the trabecular artery, which arises from the superior hypophyseal artery. The hormones released by Herring bodies enter the blood circulation through the capillary plexuses of the inferior hypophyseal and trabecular arteries.

332 UNIT 3 ■ Organ Systems
A |
|
|
Figure 17-6A. |
|
Pars nervosa, neurohypophysis (posterior |
|
|
Pituicytes |
pituitary gland). |
Masson trichrome stain, 281 |
|
|
|
|
|
|
|
|
|
|
The neurohypophysis is an outgrowth of the diencephalon |
||
|
|
|
and includes the median eminence, the infundibular stalk, |
||
|
|
|
and the pars nervosa. The median eminence is the termina- |
||
|
Capillary |
|
tion site of short |
axons carrying factors from the arcuate |
|
|
|
nuclei that regulate activity of cells in the adenohypophysis. |
|||
|
|
|
|||
|
|
|
Long axons from the supraoptic and paraventricular nuclei of |
||
|
|
|
the hypothalamus pass through the infundibular stalk and termi- |
||
|
|
|
nate in the pars nervosa (Fig. 17-3A). The pars nervosa contains |
||
|
Herring |
|
unmyelinated axons, axon terminals, pituicytes, and capillaries. |
||
|
bodies |
|
Precursors of hormones (ADH/vasopressin and oxytocin) and |
||
|
|
|
|||
|
|
|
carrier proteins (neurophysins) are synthesized in the cell bodies |
||
Lumen of |
|
of neurons in the two hypothalamic nuclei and are transported |
|||
|
through the axons in the infundibular stalk to the axon terminal |
||||
small vein |
|
||||
|
endings in the pars nervosa, where processing is completed and |
||||
|
|
|
|||
|
|
|
secretion occurs adjacent to fenestrated capillaries. Herring bod- |
||
|
|
|
ies are large dilated axon terminal endings that are filled with |
||
|
|
|
accumulated neurosecretory granules. Pituicytes are glial cells |
||
|
|
|
that provide support and nutrition to the axons of the neurons. |
||
B
Herring |
Pituicyte |
body |
|
Fenestrated capillary
Axon terminals
 Pituicyte
Pituicyte
Figure 17-6B. Pars nervosa, posterior pituitary gland. EM, 30,000; inset (color) Masson trichrome stain, 791
Major components of the posterior lobe can be seen in this electron micrograph. Terminals of hormone secreting neurons are seen as vesicle-filled, membrane-bounded profiles of widely varying shapes and sizes. The largest, most distended profiles appear as Herring bodies in ordinary sections for light microscopy. The vesicles have been transported in unmyelinated axons to this site from the supraoptic and paraventricular nuclei of the hypothalamus, where they were constructed in the cell bodies of the neurons. ADH or oxytocin is released when action potentials are conducted from the hypothalamus in response to neural signals acting on the cell bodies and dendrites in the hypothalamus. The two secreted hormones have only a short distance to diffuse to reach the wall of a fenestrated capillary. There are no neuronal cell bodies in the posterior lobe, so any nuclei seen in the posterior lobe most likely will belong either to endothelial cells of capillaries or to pituicytes, as is the case with the nucleus in this view. Like astrocytes in other parts of the central nervous system, pituicytes have processes that contact nerve processes and the walls of capillaries.

CHAPTER 17 ■ Endocrine System |
333 |
CLINICAL CORRELATIONS
Normal
Prolactinoma—H&E
A
Acidophils
 Tumor cells
Tumor cells
Interstitial |
Pleomorphic |
blood |
nucleus |
Normal
Prolactinoma—immunocytochemistry
B
Prolactin-producing
cells
Tumor cells
Figure 17-7A,B. Pituitary Adenoma. A:
H&E, (left) 213; (right) 154. B: Immunocytochemistry, (left) 213; (right) 154
Pituitary adenomas are benign tumors of the anterior pituitary gland. Clinically, they can be divided into nonsecreting and secreting forms. Historically, adenomas were classified by their staining properties, the degree to which they took up the stains hematoxylin and eosin. They were classified as basophilic, acidophilic, or chromophobic adenomas. With modern immunocytochemical techniques, however, tumor cells can be classified by the type of hormone they produce. Some cells do not mark with any antibody, and their tumors are called null-cell adenomas. Pituitary tumors may compress the hypothalamus, cranial nerves, or the optic chiasm. A bitemporal hemianopia is commonly seen in patients suffering from compression of the optic nerve. Mutations are believed to play a role in the development of the tumors. Pathologically, the tumors are composed of uniform, polygonal cells arrayed in sheets or cords. They lack a reticular network of supporting connective tissue and show monomorphism. Treatment includes drug therapy and surgery, depending on the type and the size of the tumors. A: The prolactinoma lacks acidophils and has tumor cells with pleomorphic nuclei (variable size nuclei). The normal tissue of the pars distalis of the pituitary gland shows individual or clusters of acidophils interspersed among basophils and chromophobes (right). B: The cell membranes of prolactin-producing tumor cells have been stained brown using an immunocytochemical reaction. The majority of the cells in this sample are tumor cells. By contrast, in the normal tissue sample shown on the right, only a small number of prolactin-producing cells are stained.
|
|
|
|
|
|
|
|
|
Figure 17-7C. |
Pituitary Adenoma in Magnetic Resonance |
|
|
C |
|
Imaging. |
|
|
|
|
|
Pituitary tumors, called adenomas, can be classified accord- |
||
|
|
|
ing to their size, secretory status, histology, and general |
||
|
|
|
clinical picture of the patient. Regarding size, they can be |
||
|
|
|
microadenomas, which are less than 1 cm in size (about 50% |
||
|
|
|
of all tumors at diagnosis) and may be difficult to remove, |
||
|
|
|
and macroadenomas, which are greater than 1.0 cm in |
||
|
|
Tumor |
diameter, and may cause deficits related to hormone imbal- |
||
|
|
ance or compression of adjacent structures. Classification |
|||
|
|
|
by secretory status may reflect, for example, excess cortisol |
||
|
|
|
(Cushing disease) or prolactin (prolactinoma) or the over- |
||
|
|
|
production of growth hormone (gigantism or acromegaly). |
||
|
|
|
The MRI may reflect damage to the hypothalamus; the optic |
||
|
|
|
chiasm, nerve, or tracts; or increased intracranial pressure. |
||
|
|
|
Histologic classification relies on demonstrating particular |
||
|
|
|
abnormal cell types in biopsy samples. |
||
|
|
|
|
|
|

334 UNIT 3 ■ Organ Systems
Thyroid Gland
A
Connective
 tissue septum
tissue septum
Follicle
 Septum
Septum
Colloid
Figure 17-8A. Thyroid follicles, thyroid gland. H&E, 70
The thyroid gland is derived from the developing endoderm of the foramen cecum of the tongue; it has two lobes and is one of the largest endocrine glands. Connective tissue septa divide the thyroid gland into lobules. Each lobule consists of numerous thyroid follicles. The thyroid follicles are the main functional components of the gland; they synthesize and release T3 and T4. Each follicle is filled with colloid, which is a gelatinous substance containing the stored form of T3 and T4. The follicular cells are usually simple cuboidal cells but may change to simple squamous (inactive) or columnar cells (active) depending on their states of secretion (Fig. 17-8B).
The thyroid hormones play an important role in regulating the basal metabolic activity of the body. Iodine is required for formation of thyroxine; iodine deficiency can lead to the development of thyroid goiters (nodules).
B
Colloid |
|
|
Follicular |
Parafollicular |
(cuboidal) |
cells |
cells |
Follicular (squamous) cells
Figure 17-8B. Parafollicular cells, thyroid gland. H&E, 702
Another type of endocrine cell located between the follicules of the thyroid gland is called a parafollicular cell. These cells are also called clear cells or C cells and are commonly located within the interstitial connective tissue septa. Parafollicular cells produce calcitonin, which inhibits osteoclasts from resorbing bone tissue, thereby decreasing blood calcium levels. High blood calcium levels stimulate parafollicular cells to secrete calcitonin. Parafollicular cells are relatively large cells with round nuclei and pale cytoplasm. They can be found scattered beneath the follicular cells or in small groups in the interstitial connective tissue between the follicles, as shown here.
Graves disease is an example of hyperthyroidism in which excessive amounts of thyroid hormones are secreted by follicular cells (see Fig. 3-5C). In hypothyroidism, thyroid glands produce abnormally low levels of thyroid hormones, such as in Hashimoto thyroiditis.
CLINICAL CORRELATION
C |
Thyroid |
follicle |
Lymphocytes |
in germinal |
center |
Hurthle cell |
change |
Figure 17-8C. Hashimoto Thyroiditis. H&E, 55
Hashimoto thyroiditis is a chronic autoimmune disease, characterized by enlargement of the thyroid gland (goiter) and gradual failure of thyroid function. Hashimoto thyroiditis is the most common cause of hypothyroidism in the United States and primarily affects women. Autoantibodies against thyroid antigens, genetic susceptibility, and environmental factors are believed to play a role in the development of the disease. The signs and symptoms related to hypothyroidism include fatigue, increased sensitivity to cold, pale skin, constipation, muscle pain and weakness, and weight gain. Histologically, infiltrating lymphocytes form lymphoid follicles (lymphatic nodules) with germinal centers within the thyroid parenchyma. Some thyroid follicle cells show Hurthle cell change with abundant eosinophilic cytoplasm. Thyroid hormone replacement therapy is the treatment for the disease. Surgery may be indicated if enlargement of the thyroid gland causes compression of the airway.

CHAPTER 17 ■ Endocrine System |
335 |
Parathyroid Glands
|
Blood |
Septa |
Figure 17-9A. |
Overview of the parathyroid glands. H&E, 37 |
|
|
vessel |
The four small parathyroid glands typically lie on the posterior |
|||
|
|
|
|
||
|
|
|
|
surface of the thyroid gland (Fig. 17-1) and are separated from |
|
|
|
|
|
the thyroid gland by a connective tissue capsule. Connective tissue |
|
|
|
|
|
septa with blood vessels divide each parathyroid gland into many |
|
|
|
|
|
incomplete lobules. The parathyroid glands are derived from the |
|
|
|
|
|
endoderm of pharyngeal pouch 3 (the inferior parathyroid glands) |
|
|
|
|
|
and pouch 4 (the superior parathyroid glands). There are two |
|
|
|
|
|
types of cells in the parathyroid glands: chief cells and oxyphil |
|
|
|
|
|
cells (Fig. 17-9B). Adipocytes are commonly found in the parathy- |
|
|
|
|
|
roid glands in older individuals. |
|
|
Capsule |
|
|
|
|
|
|
|
Blood |
||
|
A |
|
vessels |
||
|
|
|
|
|
|
|
|
|
|
|
|
Chief |
Connective |
cells |
tissue |
|
septum |
|
Blood |
|
vessels |
|
Chief |
Capillary |
|
cells |
|
B |
Oxyphil |
Oxyphil cells |
cells |
Figure 17-9B. Chief cells and oxyphil cells of the parathyroid glands. H&E, 139; inset 296
The chief cells are smaller and more numerous than the oxyphil cells. They are distributed throughout the glands and are the principal cells in the parathyroid glands. Each chief cell has a large round nucleus with a small amount of clear cytoplasm. These chief cells produce PTH, also called parathormone, which is secreted in response to low blood calcium levels. PTH indirectly promotes osteoclast proliferation and increases their activity of absorption of bone tissue to increase blood calcium levels. The oxyphil cells are large cells with acidophilic (pink) cytoplasm as shown here. Each cell has a small nucleus and a large amount of cytoplasm containing numerous mitochondria. The oxyphil cells are often arranged in clusters; individual cells can also be found scattered among the chief cells. The oxyphil cells appear at puberty, and their numbers increase with age. Their functions are unclear.
CLINICAL CORRELATION
C
Adenoma composed of chief cells
Normal parathyroid gland with adipose tissue
Adipocytes
Figure 17-9C. Parathyroid Adenoma. H&E, 96
Parathyroid adenomas are benign neoplasms of the parathyroid gland representing the most common cause of primary hyperparathyroidism, in which autonomous overproduction of parathyroid hormone occurs. The increased parathyroid hormone results in elevated blood calcium (hypercalcemia), which may cause constipation, kidney stones, neuropsychiatric issues, and bone diseases such as osteitis fibrosa cystica. The majority of cases are asymptomatic, discovered incidentally when hypercalcemia is detected on routine blood tests. Most cases are sporadic, but some cases may be related to inherited conditions like multiple endocrine neoplasia (MEN1 and MEN2). Parathyroid adenomas are usually solitary, whereas parathyroid hyperplasia tends to affect all four glands. Grossly, these adenomas are well circumscribed with a red-to-brown cut surface. Histologically, an adenoma is enveloped with a capsule, is usually composed of monomorphic chief cells, and tends to compress the surrounding normal parathyroid tissue. Definitive treatment is surgical removal of the parathyroid gland containing the adenoma.

336 UNIT 3 ■ Organ Systems
Adrenal Glands (Suprarenal Glands)
Fig. 17-10B
A
Cortex 
Medulla 
Cortex |
Medulla |
Capsule 
Zona reticularis 
Zona fasciculata 
Zona glomerulosa 
Figure 17-10A. Overview of the adrenal glands. H&E, 7
An adrenal gland covers the apical region of each kidney. It is also called the suprarenal gland (Fig. 17-1A). Each adrenal gland is covered by a connective tissue capsule and has a cortex and a medulla. The cortex of the adrenal gland is derived from the mesoderm and can be divided into three zones: the zona glomerulosa, zona fasciculata, and zona reticularis. Hormone-producing cells in the cortex secrete several types of hormones: mineralocorticoids, glucocorticoids, and weak androgens. The medulla of the adrenal gland is derived from the neural crest and contains cell bodies of sympathetic ganglion neurons and their axons as well as chromaffin cells, which synthesize and release adrenaline
(epinephrine) and noradrenaline (norepinephrine) (Fig. 17-12A,B).
B
Zona glomerulosa |
1 |
Capsule |
1 |
2 |
|
|
|
2 |
Capillaries |
|
|
Zona fasciculata |
|
|
Capillary |
Cortex |
|
Zona fasciculata |
|
|
|
||
Zona glomerulosa |
|
|
|
Zona reticularis |
3 |
Zona reticularis |
4 |
|
|
||
3 |
|
|
|
Zona reticularis |
|
|
|
4 |
|
|
|
Medulla |
Capillary |
|
Capillary |
|
Medulla |
||
|
|
|
Figure 17-10B. Cortex of the adrenal gland. H&E, left 41, left (insets) 466; right (4 panels) 163
The cortex of the adrenal gland contains many glandular cells. These cells are arranged in cords, which are formed by hormone secretory cells. The capillaries run parallel to these cords. (1) The zona glomerulosa lies beneath the connective capsule and consists of secretory cells that contain lipid droplets (vacuoles) and a pale-staining cytoplasm. These cells are arranged in round or ovoid clusters (like glomeruli); they secrete mineralocorticoids, mainly aldosterone, which control the electrolyte balance by acting on the distal tubules of the kidney to increase Na+ and decrease K+ absorption. (2) The zona fasciculata contains hormone-secreting cells that secrete glucocorticoids (mainly cortisol and corticosterone). The glucocorticoids stimulate glycogen synthesis in the liver; increase carbohydrate, fat, and protein metabolism; and suppress the immune response by slowing down immune cell (lymphocyte) circulation. ACTH stimulates the production of glucocorticoids. The cells in the zona fasciculata contain many lipid droplets, which make the cytoplasm appear light and vacuolated. These cells are arranged in long cords in which cell nuclei are packed close to one another with their pale-stained cytoplasm facing the capillaries.
(3) The zona reticularis is adjacent to the medulla. Its secretory cells contain only a few lipid droplets, and their cytoplasm is stained dark and acidophilic in appearance. The cells are arranged in anastomosing cords, which are intermixed with by surrounding capillaries. These secretory cells secrete androgens (mainly dehydroepiandrosterone), which can be converted into testosterone or estrogen. ACTH also stimulates the secretion of the adrenal androgens. (4) The junction between the zona reticularis and the medulla is shown here. There are many blood vessels separating the zona reticularis of the cortex and the medulla. The cells in the medulla are stained lighter than the cells in the zona reticularis. The left insets show a high power view of hormone secreting cells in the zona glomerulosa, zona fasciculata, and zona reticularis of the adrenal gland cortex. The right panels show regions of the adrenal gland that are indicated by the dashed boxes.

CHAPTER 17 ■ Endocrine System |
337 |
A
Secretory cells in zona reticularis
Rough
endoplasmic reticulum
Smooth
endoplasmic reticulum
Nucleolus
Mitochondrion with tubular cristae
Lipid droplets
Figure 17-11A. Adrenal cortical cells, adrenal cortex. EM, 11,500; inset (color) H&E, 680
Cells of the adrenal cortex have features common to all cells that synthesize and secrete steroid hormones. The three most prominent components of the cytoplasm are an abundance of smooth endoplasmic reticulum (SER), mitochondria that have peculiar tubular cristae, and lipid droplets. Cholesterol, the precursor of steroid hormones, is stored as esters in the lipid droplets. Enzymes necessary for synthesis of steroid hormones are located in the SER and in the inner mitochondrial membrane, so hormone production is a cooperative function of these two organelles. Although proteins are not secreted by these cells, protein synthesis is required to maintain structure and function. This is reflected by the prominent nucleolus and by the patches of RER.
CLINICAL CORRELATION
B
Adjacent normal  adrenal cortex
adrenal cortex
Pheochromocytoma
 with zellballen
with zellballen
Figure 17-11B. Pheochromocytoma. H&E, ×96 Pheochromocytomas are neoplasms of the adrenal medulla characterized by the production of catecholamines, such as epinephrine and norepinephrine, which cause significant hypertension, often episodic, in affected patients. Most pheochromocytomas are sporadic, but about 10% are associated with familial syndromes such as MEN (types 2A and 2B), and von Hippel-Lindau. Some pheochromocytomas are bilateral, and although most occur in adults, about 10% occur in children. Grossly, most of these tumors are well circumscribed and range in size from a few grams to kilograms. Microscopically, pheochromocytomas can have a diverse appearance, from spindle cells to large, bizarre cells. The cells are often arranged in nests, or cell packets called zellballen. Histologic features alone do not reliably separate benign tumors from malignant ones; therefore, the demonstration of metastases is necessary to ascertain malignancy. Definitive treatment is surgical removal of the tumor.

338 UNIT 3 ■ Organ Systems
A |
|
Figure 17-12A. |
Adrenal medulla. H&E, 140; inset (left) |
|
Blood cells |
340; inset (right) 158 |
|
|
|
|
|
|
in the vein |
|
|
Cell bodies of ganglion neurons
Chromaffin
cells
Nerve fibers
The adrenal medulla is derived from the neural crest; its embryonic origin is different from that of the adrenal cortex. The cells in the adrenal medulla include chromaffin cells and ganglion neurons. Large blood vessels (veins) are found in the medulla; these vessels drain blood out of the adrenal gland. Chromaffin cells are irregularly shaped neuroendocrine cells and are the predominant cells in the adrenal medulla. These cells have round nuclei with pale-staining cytoplasm as shown here. They have numerous plasma secretory granules that stain intensively with chromium salts; therefore, they are called chromaffin cells. These cells secrete the sympathomimetic hormones adrenaline (epinephrine) and noradrenaline (norepinephrine) in response to stress. The sympathetic ganglion neurons have large cell bodies that are surrounded by supporting cells as shown in the left inset. The adrenal medulla is innervated by sympathetic preganglionic nerves.
B
of Lumen fenestratedcapillary
Chromaffin cells
Nucleus of chromaffin cell
Nucleolus
Rough
endoplasmic reticulum
Norepinephrine
granule
Figure 17-12B. Cells of the adrenal medulla. EM, 5,700; inset (color) H&E, 1,632
Cells of the adrenal medulla synthesize and secrete adrenaline (epinephrine) and noradrenaline (norepinephrine), with adrenaline being the main product. These catecholamines are both synthesized from the amino acid tyrosine through a series of reactions that occur in the cytosol and within the granules in the cytoplasm. The generation of the granules, along with the enzymes, packaging proteins, and membrane proteins, involves the RER and Golgi complex, so these cells have equipment similar to a proteinsynthesizing cell, although their product is not a protein. The granules vary greatly in size and appearance, a reflection partly of the current state of activity (synthesis, storage) and partly of the catecholamine (epinephrine, norepinephrine) stored in the granule. The granules that store norepinephrine (noradrenaline) are the large electron-lucent profiles containing a small electron-dense particle at the edge of the cavity. Like the cells of the cortex, the cells of the adrenal medulla are closely associated with the walls of fenestrated capillaries. However, the edge of the vessel in the upper left corner of this view does not show the fenestrations.

CHAPTER 17 ■ Endocrine System |
339 |
Pineal Gland
A
Capsule
Pineal
 gland
gland
Posterior commissure Superior
colliculus
Brain Septum sand
Figure 17-13A. Overview of the pineal gland. H&E, 5
The pineal gland is a pinecone-shaped neuroendocrine gland about 8 mm in length that produces melatonin and is covered by a capsule of pia mater. The pineal gland is part of the epithalamus (a diencephalic structure) that extends caudally from its attachment immediately superior to the posterior commissure into the superior (quadrigeminal) cistern. It is superior to the colliculi of the midbrain. Secretion of melatonin is stimulated by darkness and inhibited by light. The level of this hormone increases during sleep. Connective septa divide the pineal into poorly defined lobules. This gland contains pinealocytes, neuroglial cells, and blood vessels. Calcified concretions called brain sand (also called corpora arenacea) may also be present in the pineal gland, especially in older patients.
The calcifications (brain sand) within the pineal gland increase with age. These calcifications appear white in computed tomography scan and magnetic resonance imaging and are commonly used as a natural landmark by radiologists and neurologists.
B |
Pinealocytes |
|
Pinealocytes |
Capillary
Neuroglial
cells
Neuroglial
cells Capillary
Brain sand
Brain
sand
Figure 17-13B. Pinealocytes and brain sand of the pineal gland.
H&E, 140; insets 363
The pineal gland is composed of two types of cells: pinealocytes and neuroglial cells. The pinealocytes are modified neurons, which have round or ovoid nuclei with pale-stained cytoplasm containing granules filled with melatonin. The pinealocytes synthesize melatonin, which is important in the regulation of the circadian rhythms (day and night cycles). The pinealocytes are larger than the neuroglial cells and have a long cytoplasmic process that extends to the capillaries; their secretory granules are released into the capillaries. The neuroglial cells are supportive cells with small, dark nuclei. They are also called pineal astrocytes and are commonly found near the capillaries. The particles of brain sand assume various sizes as shown here; their function is not known. Other functions of the pineal gland may relate to promoting sleep and sexual development; enhancing mood and slowing the aging process; and, possibly, inhibiting the growth of some tumors.
CLINICAL CORRELATION
 C
C
Tumor
Nucleus of tumor cell
Synaptophysin in tumor cell cytoplasm
Figure 17-13C. Pineoblastoma. Immunohistochemical preparation for synaptophysin, 198
Pineoblastoma is an aggressive malignant tumor in children, which arises in the pineal gland. Because it commonly consists of cellular sheets that lack an architectural pattern, it is described as a small blue cell tumor. The term embryonal is also used to emphasize the rudimentary developmental stage of the tumor, although in some tumors the cells begin to show differentiation into neurons, or glial cells, or even rods and cones. The earliest stages of such specialization may be detectable before any architectural alteration. Synaptophysin is a protein associated with synapses. An antibody to this marker protein, conjugated to the enzyme peroxidase, creates a colored metabolite wherever synaptophysin appears in cell cytoplasm or membranes. In the image on the left, a brown compound marks the tumor cells that contain synaptophysin. Tumor treatments can be individually formulated based on the different cellular components.

340 UNIT 3 ■ Organ Systems
Endocrine Pancreas
A
Connective Islets of tissue
Langerhans
Exocrine secretory cells
Small |
Septum |
Interlobular |
artery |
duct |
Figure 17-14A. Islets of Langerhans, endocrine pancreas. H&E,
39
The pancreas has endocrine and exocrine components. The endocrine component consists of the islets of Langerhans, which are clusters of endocrine cells within a capillary network. There are numerous palestaining islets of Langerhans scattered throughout the pancreas, and each of them is surrounded by an eosinophilic exocrine component of the pancreas as shown here. A connective tissue septum divides the pancreas into lobules. Two interlobular ducts, surrounded by the connective tissue, belong to the exocrine pancreas, from which they carry secretions. The endocrine pancreas does not have ducts; the hormones (insulin and glucagon) secreted by the islets of Langerhans are released into the capillaries and from there into the blood circulation. Insulin and glucagons play important roles in regulating blood glucose levels. Insulin stimulates glucose entry in many cells, thereby regulating carbohydrate metabolism and lowering blood glucose levels. Glucagon enhances the synthesis and release of glucose from the liver into the blood, thus increasing blood glucose levels.
B
Exocrine
gland Exocrine
secretory cells
Capillaries
Islet of
Langerhans
Islet of
Langerhans
Exocrine
gland Endocrine  secretory cells
secretory cells
Figure 17-14B. Islets of Langerhans, endocrine pancreas. H&E, 462
There are four types of endocrine cells in the islets of Langerhans: alpha cells, beta cells, delta cells, and PP cells. It is difficult to distinguish among them in H&E stain. However, the beta cells are usually distributed throughout the islets; the other three types of cells are commonly found at the periphery of the islets. Alpha cells secrete glucagon, beta cells secrete insulin, delta cells secrete somatostatin and gastrin, and PP cells secrete pancreatic polypeptide. Secretion of insulin occurs in response to high blood glucose levels; secretion of glucagon occurs in response to lower blood glucose levels.

CHAPTER 17 ■ Endocrine System |
341 |
A
Insulin-producing
(beta) cells
Exocrine
secretory Capillaries cells
Figure 17-15A. Pancreatic islet cells, islets of Langerhans.
Immunocytochemistry stain, 189
This is an example of an islet of Langerhans prepared with a special immunocytochemistry stain for insulin. Cells with brown color are insulin-producing cells and are the predominant cells in the islets of Langerhans. Insulinproducing cells, also called beta cells, are distributed throughout the pancreatic islets. The background counterstain is hematoxylin, which makes the endocrine pancreatic cells appear light blue with darker blue–stained nuclei.
Type 1 diabetes mellitus is the most common type of diabetes in childhood and adolescence (65% of total cases). It is characterized by insulin deficiency and sudden onset of severe hyperglycemia, diabetic ketoacidosis, and death if patients are left without insulin treatment. Symptoms also include polyuria, polydipsia, lethargy, and weight loss. The major cause of the disease is autoimmune destruction of the insulin-secreting beta cells in the islets of Langerhans by T cells and humoral mediators (tumor necrosis factor, interleukin-1, nitric oxide). Treatment options depend largely on patient and physician preferences and include baseline doses of insulin plus adjustable premeal doses of short-acting insulin or rapid-acting insulin analogs.
B
Secretory granules in beta cell
Endocrine secretory cell
Rough endoplasmic reticulum
Golgi complex
Secretory granules in alpha cell
Erythrocyte in lumen of fenestrated capillary
Figure 17-15B. Pancreatic islet cells, islets of Langerhans. EM, 13,000; inset (color) H&E, 1,632
Pancreatic islet cells, like other types of endocrine cells, are closely associated with fenestrated or sinusoidal capillaries. The granules of each of the four main types of cells have slightly different characteristic appearances in electron micrographs. Profiles of two different cells are visible in this view. The cell adjacent to the wall of the capillary appears to be an alpha (glucagon-secreting) cell with small-to-medium granules that have an electron-dense core with a very narrow electron-lucent surround. The profile in the upper left appears to belong to a beta (insulin-secreting) cell with larger granules, a less dense core, and a wide lucent area surrounding the core. The nuclei of the cells are not present in this view, but note that the cytoplasm of the alpha cell exhibits typical features of a polypeptide synthesizing and secreting cell: Both RER and a large Golgi complex are readily apparent.
342 UNIT 3 ■ Organ Systems
CLINICAL CORRELATION
Exocrine
 pancreas
pancreas
Amyloid  replacing
replacing
islet of Langerhans
Figure 17-16. Type 2 Diabetes Mellitus. H&E, 195 Type 2 diabetes mellitus is characterized by hyperglycemia with normal or elevated insulin levels, in contrast to type 1 diabetes in which hyperglycemia is associated with little or no insulin production. In type 2 diabetes, insulin is present, but insulin-sensitive tissues, such as skeletal muscle and adipose tissues, manifest resistance to the action of insulin. Defects in beta cell function also contribute to the disease process. Type 2 diabetes generally has an insidious onset and typically affects adults. Risk factors include genetic factors and a strong association with obesity. Approximately 85% of type 2 diabetes is associated with obesity. Clinically, patients present primarily with polyuria and polydipsia due to the hyperglycemia. Chronic hyperglycemia leads to accelerated atherosclerosis and small vessel damage, which affects the eyes (retinopathy), kidneys (nephropathy), and nerves (neuropathy). Early in the disease, the islets of Langerhans become hyperplastic in order to produce more insulin. Later in the disease, the islets become atrophic with amyloid deposition. Treatment includes diet modification and exercise to induce weight loss and the use of oral hypoglycemic medications. Some patients may require insulin late in the disease process because of progressive loss of beta cells.
SYNOPSIS 17 - 1 Pathological Terms for the Endocrine System
■Bitemporal hemianopia: A visual field deficit characterized by loss of both temporal visual fields, most often due to compression of the optic chiasm by a pituitary tumor or cyst (Fig. 17-7A,B).
■Goiter: A general term for enlargement of the thyroid gland; common causes include benign multinodular goiter, diffuse toxic goiter, and thyroiditis (Fig. 17-8C).
■Osteitis fibrosa cystica: A cystic bone lesion seen in patients with hyperparathyroidism due to increased osteoclast activity and bone resorption caused by elevated parathyroid hormone (Fig. 17-9C).
■Polydipsia: Term describing patients with excessive thirst, commonly seen in diabetes mellitus when hyperglycemia causes osmotic fluid diuresis with resultant dehydration and thirst (Fig. 17-16).
■Polyuria: Term describing excessive urination, commonly seen in diabetes mellitus when hyperglycemia produces osmotic fluid diuresis with resultant dehydration and secondary polydipsia (Fig. 17-16).
■Amyloid: Extracellular glycoproteins characterized physically by fibrillar ultrastructures and chemically by response to special staining reactions (Fig. 17-16).

CHAPTER 17 ■ Endocrine System |
343 |
TABLE 17 - 1 |
Endocrine Organs |
|
|
||
Gland Name |
Hormone |
Hormone Produced |
Target Tissues and |
Main Functions |
|
|
|
producing Cells |
|
Organs |
|
|
|
|
|
|
|
Pituitary Glands |
|
|
|
|
|
|
|
|
|
|
|
Adenohypophysis |
|
Acidophils: |
Growth hormone |
Liver (primary); bone, |
Stimulate body growth |
(anterior pituitary) |
|
Somatotrophs |
Somatotropin |
muscle, and adipose tissue |
|
|
|
|
|
(secondary) |
|
|
|
Mammotrophs |
Prolactin |
Mammary gland |
Stimulate mammary glands to produce |
|
|
|
|
|
milk |
|
|
Basophils: |
ACTH and |
Adrenal cortex |
Stimulate secretion of glucocorticoids and |
|
|
Corticotrophs |
corticotropin |
|
androgens |
|
|
Thyrotrophs |
TSH |
Thyroid gland |
T3 and T4 |
|
|
Gonadotrophs |
FSH |
Ovaries |
Stimulate oocytes to develop and promote |
|
|
|
|
|
|
|
|
|
|
|
estrogen secretion |
|
|
|
LH |
Testes |
Stimulate testes to produce sperm |
Neurohypophysis |
|
Neurosecretory |
Vasopressin/ADH |
Collecting tubules of |
Promote collecting tubules’ permeability |
(posterior pituitary) |
|
cells from |
|
kidney; smooth muscle in |
to water |
|
|
hypothalamus |
|
arterioles |
|
|
|
|
Oxytocin |
Uterus, mammary gland |
Stimulate contraction of uterus and |
|
|
|
|
|
mammary gland |
Thyroid Gland |
|
|
|
|
|
|
|
|
|
|
|
|
|
Follicular cells |
T3 and T4 |
Most tissues of body |
Increase metabolic rate; influence body |
|
|
|
|
|
growth and development |
|
|
Parafollicular cells |
Calcitonin |
Bone |
Inhibit osteoclasts’ absorption activity and |
|
|
|
|
|
reduce blood calcium level |
Parathyroid Gland |
|
|
|
|
|
|
|
|
|
|
|
|
|
Chief cells |
PTH |
Bone; small intestine; |
Increase osteoclasts’ absorption activity and |
|
|
|
|
kidney |
increase blood calcium level |
Adrenal Gland |
|
|
|
|
|
|
|
|
|
|
|
Adrenal cortex |
|
Secretory cells in |
Mineralocorticoids |
Renal tubules of the |
Influence salt and water balance by |
|
|
zona glomerulosa |
(aldosterone) |
kidney |
promoting renal tubule reabsorption of |
|
|
|
|
|
Na+ and water and secretion of K+ |
|
|
Secretory cells in |
Glucocorticoids (cortisol |
Liver; immune cells (such |
Involved in carbohydrate metabolism |
|
|
zona fasciculata |
or hydrocortisone; |
as T and B lymphocytes |
and stimulation of gluconeogenesis in |
|
|
|
corticosterone) |
and macrophages); muscle |
the liver; immunosuppressive; reduces |
|
|
|
|
and adipose tissue |
muscle and adipose tissue uptake of |
|
|
|
|
|
glucose |
|
|
Secretory cells in |
Weak androgens |
Testes; uterine and |
As weak androgens, can be converted to |
|
|
zona reticularis |
(dehydroepiandrosterone, |
mammary glands; other |
either testosterone or estrogen; contribute |
|
|
|
androstenedione) |
tissue, such as bone, hair, |
to sex characteristics and reproduction |
|
|
|
|
etc. |
|
Adrenal medulla |
|
Chromaffin cells: |
|
|
Increase heart rate and cardiac output; |
|
|
Adrenaline |
Adrenaline (epinephrine) |
Heart; blood vessel; liver |
constrict blood vessels in organs and |
|
|
secreting cells |
|
and adipocytes |
increase blood flow to heart and to |
|
|
|
|
|
skeletal muscle |
|
|
Noradrenaline |
Noradrenaline |
|
Increase release of glucose and fatty acids |
|
|
secreting cells |
(norepinephrine) |
|
into blood; dilate pupils, and prepare body |
|
|
|
|
|
for action. |
|
|
|
|
|
|
Pineal Gland |
|
|
|
|
|
|
|
|
|
|
|
|
|
Pinealocytes |
Melatonin |
Hypothalamus |
Regulate circadian rhythms; promote sleep |
|
|
|
Serotonin |
|
and control sexual activity; enhance mood |
|
|
|
|
|
and slow the aging process |
Endocrine Pancreas |
|
|
|
|
|
|
|
|
|
|
|
|
|
Alpha |
Glucagon |
Liver; gastric glands; |
Regulate blood glucose levels; stimulate |
|
|
Beta, |
Insulin |
exocrine pancreas |
gastric gland secretion; inhibit exocrine |
|
|
Delta |
Somatostatin |
|
pancreatic secretion |
|
|
PP cells |
Pancreatic polypeptide |
|
|
|
|
|
|
|
|
ACTH, adenocorticotropic hormone; TSH, thyroid-stimulating hormone; FSH, follicle-stimulating hormone; LH, luteinizing hormone; ADH, antidiuretic hormone; T3, triiodothyrodine; T4, thyroxine; PTH, parathyroid hormone; PP cells, pancreatic polypeptide cells.

18 Male Reproductive
System
Introduction and Key Concepts for the Male Reproductive System
Figure 18-1 |
Overview of the Male Reproductive System |
Figure 18-2 |
Orientation of Detailed Male Reproductive System Illustrations |
Testis |
|
Figure 18-3A |
Overview of the Testis |
Figure 18-3B,C |
Seminiferous Tubules of the Testis |
Figure 18-4A |
Cells in the Seminiferous Tubules |
Figure 18-4B |
Seminiferous Epithelium |
Figure 18-5 |
Seminiferous Epithelium, Early Spermatid |
Figure 18-6A |
Sertoli Cells, Seminiferous Tubules |
Figure 18-6B |
Sertoli Cell and Primary Spermatocyte, Seminiferous Epithelium |
Figure 18-7 |
Interstitial Cells of Leydig |
Synopsis 18-1 |
Functions of Sertoli Cells |
Synopsis 18-2 |
Functions of Testosterone |
Figure 18-8 |
Hormone Regulation Involving the Testicular Cells |
|
(Interstitial Cells of Leydig and Sertoli Cells) |
Figure 18-9 |
Overview of Readily Identifiable Spermatogenic Cells in the Seminiferous Epithelium |
Figure 18-10 |
Overview of Spermatogenesis and the Stages of the Seminiferous Epithelium |
Figure 18-11A |
Stage I Seminiferous Epithelium |
Figure 18-11B |
Stage II Seminiferous Epithelium |
Figure 18-12A |
Stage III Seminiferous Epithelium |
Figure 18-12B |
Stage IV Seminiferous Epithelium |
Figure 18-13A |
Stage V Seminiferous Epithelium |
Figure 18-13B |
Stage VI Seminiferous Epithelium |
Intratesticular Genital Ducts |
|
Figure 18-14A |
Intratesticular Genital Ducts |
Figure 18-14B |
Tubuli Recti |
344
