
Revision Sinus Surgery
.pdf
198
20.Marple BF, Fornadley JA, Patel AA, et al. (2007) Keys to successful management of patients with allergic rhinitis: focus on patient confidence, compliance, and satisfaction. Otolaryngol Head Neck Surg 136:S107–S124
21.Morgan WJ, Crain EF, Gruchalla RS, et al. (2004) Results of a home-based environmental intervention among urban children with asthma. N Engl J Med 351:1068–1080
22.Nathan RA (2007) The burden of allergic rhinitis. Allergy Asthma Proc 28:3–9
23.Newman LJ, Platts-Mills TA, Phillips CD, et al. (1994) Chronic sinusitis. Relationship of computed tomographic findings to allergy, asthma, and eosinophilia. JAMA 271:363–367
24.Platts-Mills TA, Vaughan JW, Carter MC, et al. (2000) The role of intervention in established allergy: avoidance of indoor allergens in the treatment of chronic allergic disease. J Allergy Clin Immunol 106:787–804
25.Ramadan HH (1999) Surgical causes of failure in endoscopic sinus surgery. Laryngoscope 109:27–29
26.Ramadan HH, Hinerman RA (2006) Outcome of endoscopic sinus surgery in children with allergic rhinitis. Am J Rhinol 20:438–440
27.Robinson S, Douglas R, Wormald PJ (2006) The relationship between atopy and chronic rhinosinusitis. Am J Rhinol 20:625–628
Li-Xing Man and Berrylin J. Ferguson
28.Schulman, Ronca, and Bucuvalas, Inc (2006) Allergies in America: A Landmark Survey of Nasal Allergy Sufferers. Executive Summary. Available at: http://www.myallergiesi- namerica.com/executive–summary.php. Accessed August 6, 2007. Altana Pharma US, Florham Park, NJ
29.Sheikh A, Hurwitz B, Shehata Y (2007) House dust mite avoidance measures for perennial allergic rhinitis. Cochrane Database Syst Rev:CD001563
30.Sly RM (1999) Changing prevalence of allergic rhinitis and asthma. Ann Allergy Asthma Immunol 82:233–248; quiz 248–252
31.Smith TL, Mendolia-Loffredo S, Loehrl TA, et al. (2005) Predictive factors and outcomes in endoscopic sinus surgery for chronic rhinosinusitis. Laryngoscope 115:2199–2205
32.Sobol SE, Wright ED, Frenkiel S (1998) One-year outcome analysis of functional endoscopic sinus surgery for chronic sinusitis. J Otolaryngology 27:252–257
33.Weiner JM, Abramson MJ, Puy RM (1998) Intranasal corticosteroids versus oral H1 receptor antagonists in allergic rhinitis: systematic review of randomised controlled trials. BMJ 317:1624–1629
34.Wilson AM, O’Byrne PM, Parameswaran K (2004) Leukotriene receptor antagonists for allergic rhinitis: a systematic review and meta-analysis. Am J Med 116:338–344
35.Zacharasiewicz A, Douwes J, Pearce N (2003) What proportion of rhinitis symptoms is attributable to atopy? J Clin Epidemiol 56:385–390
23

Chapter 24 |
24 |
Staging of Disease after Sinus |
|
Surgery Failure |
Valerie J. Lund
Core Messages
■Despite many suggested methods of staging for chronic rhinosinusitis, there are intrinsic difficulties in finding the “perfect” solution.
■Most staging systems have relied on computed tomography (CT) scoring, endoscopic findings, symptom scores or combinations thereof and have concentrated on patients undergoing primary surgery rather than patients with recurrent symptoms awaiting revision surgery.
■Whilst a correlation can be shown between CT and endoscopic findings, the correlation between CT changes and symptoms is generally poor in either circumstance.
■The purpose of staging in inflammation/infection in contrast to malignancy may relate more to demonstration of the disease and as an inclusion criterion for clinical research than as a predictive tool.
Introduction
“Staging: the determination of the particular stage which a progressive disease or condition has reached.”.
Oxford English Dictionary 2003
“A staging system is necessary to have meaningful results”.
Caldwell 1893 [11]
“A judgement on prognosis requires an objective assessment of the anatomical extent of the disease”.
TNM: Classification of Malignant Tumours [23]
Throughout medicine considerable effort has been made to quantify and qualify disease processes to facilitate clinical management and research. In rhinology, this has proved remarkably difficult despite several objective
Contents |
|
Introduction . . . . . . . . . . . . . . . . . |
199 |
CRS and NP . . . . . . . . . . . . . . . . . |
199 |
Endoscopy . . . . . . . . . . . . . . . . . . |
203 |
Imaging . . . . . . . . . . . . . . . . . . . |
203 |
Other Methods of Assessment . . . . . . . . . |
. 211 |
Use of Staging in Outcome Research . . . . . . . |
212 |
Staging for Neoplasia . . . . . . . . . . . . . |
. 213 |
Conclusion . . . . . . . . . . . . . . . . . |
. 213 |
tests and investigations, and none more so than in the assessment of patients after surgical treatment. Part of the problem has lain with interand intra-individual variation, partly with the cost, availability and the technical requirements of some of these tests, but above all with the difficulty in correlating results with symptoms. There is clearly a need for a universally accepted method of assessing disease extent that might provide criteria for further therapeutic intervention and allow comparison of results of treatment between centres. However, this presupposes that the purpose of staging is to correlate extent of disease with outcome, using the same premise as that on which the TNM classification is based. Whilst the majority of work in this area has focused on inflammatory conditions such as chronic rhinosinusitis (CRS) and nasal polyposis (NP) where the outcomes are ultimately less finite than in cancer, some mention will also be made of staging in relation to other conditions such as benign and malignant neoplasia where recurrence and revision surgery are frequently required.
CRS and NP
■Rhinosinusitis (including NP) is defined [18] as inflammation of the nose and the paranasal sinuses

200
characterised by two or more of these symptoms, one of which should be either nasal blockage/obstruction/ congestion or nasal discharge (anterior/posterior nasal drip):
1.± Facial pain/pressure.
2.± Reduction or loss of smell. and either
3.Endoscopic signs of:
a.Polyps and/or;
b.Mucopurulent discharge primarily from the middle meatus and/or;
c.Oedema/mucosal obstruction primarily in the middle meatus.
and/or
4.Computed tomography (CT) changes: mucosal changes within the ostiomeatal complex and/or sinuses.
It would therefore seem sensible to use some, if not all of these criteria to stage disease, particularly as virtually all patients will be undergoing symptom assessment, endoscopy and imaging if they have recurrent problems and are being considered for revision surgery.
Subjective assessment of symptoms generally considers the degree and duration of those directly associated with the condition and it has been shown that in a general population of patients with CRS/NP, some of whom had undergone previous surgery, their symptoms could be divided into mild, moderate and severe based on a total severity visual analogue scale (VAS) score (0 10 cm; see below) [39].
Not |
|
Worst thinkable |
|
||
troublesome |
|
troublesome |
|
||
|
10 cm |
|
Subjective assessment of symptoms. A VAS >5 affects patient quality of life:
1.Mild = VAS 0–3
2.Moderate = VAS > 3–7
3.Severe = VAS > 7–10
■To evaluate the total severity, the patient can be asked to indicate on a VAS the answer to the question: “How troublesome are your symptoms of rhinosinusitis?”
24 |
This can be factored into any staging of disease as a |
|
measure of symptom severity (Table 24.1a). |
Other consensus documents have recommended a 0–7 scale [45] where:
1: None to an occasional limited episode. 2–3: Mild-steady symptoms but easily tolerable.
Valerie J. Lund
4–5: Moderately bothersome – symptoms are difficult to tolerate and may interfere with activities of daily living and/or sleep.
6–7: Very severe – symptoms are so bad that they cannot function all of the time.
However, it should be noted that the “normal” population do not score zero, with a mean of 8.8 being found in an ostensibly healthy sample versus a mean of 35.3 (p = 0.0001) in those with CRS [62].
When considering duration of disease, one is reliant on the definition endorsed by various drugs and therapeutic agencies around the world, which were created largely for the purpose of providing inclusion criteria for trials in acute bacterial rhinosinusitis, and which are at best generalisations and at worst, arbitrary.
■Rhinosinusitis classification:
1.Acute
a.< 12 weeks.
b.Complete resolution of symptoms.
2.Chronic
a.> 12 weeks symptoms.
b.Without complete resolution of symptoms.
CRS may also be subject to exacerbations (i.e. acute on chronic). It would be implicit in an individual requiring further surgery that their symptoms had lasted for at least 3 months, and therefore the duration has little utility in staging.
Considerable debate surrounds the relationship between CRS and NP, with many researchers believing that the two are distinct conditions with a different pathophysiology and inflammatory profile, which may have a bearing on staging. However, others prefer to consider NP as part of a spectrum of inflammation that can be generically referred to as CRS. From a practical point of view in the clinical setting, it is probably best to consider the condition as CRS without polyps and CRS with polyps, a distinction that can usually be made on endoscopy.
■Definition of CRS with/without polyps in individuals who have not had previous surgery:
1.CRS without NP: no visible polyps in the middle meatus, if necessary following administration of decongestant.
2.CRS with nasal polyposis: polyps bilateral, visualised endoscopically in the middle meatus.
This definition accepts that there is a spectrum of disease in CRS that includes polypoid change in the sinuses and/ or middle meatus but excludes those with polypoid disease presenting in the nasal cavity to avoid overlap.

Staging of Disease after Sinus Surgery Failure |
201 |
Table 24.1a The Lund-MacKay scoring system [42]: symptom scores using the visual analogue method. Each category is scored on a scale of 0–10 according to the degree of symptom severity, where 0 = symptoms not present and 10 = greatest possible severity
Symptom |
Pre-surgery After |
After |
After |
After |
After |
|
operation |
3 months |
6 months |
1 year |
2 years |
Nasal blockage or congestion |
|
|
|
|
|
Headache |
|
|
|
|
|
Facial pain |
|
|
|
|
|
Problems of smell |
|
|
|
|
|
Nasal discharge |
|
|
|
|
|
Sneezing |
|
|
|
|
|
Overall |
|
|
|
|
|
Total points |
|
|
|
|
|
|
|
|
|
|
|
Table 24.1 b Lund-MacKay scoring system: endoscopic appearances scores
Characteristic |
Baseline and follow-up |
Polyp left (0,1,2,3)a
Polyp, right (0,1,2,3)a
Oedema, left (0,1,2,)b
Oedema, right (0,1,2,)b
Discharge, left (0,1,2)c
Discharge, right (0,1,2)c
Postoperative scores to be used for outcome assessment only
Scarring, left (0.1,2)d
Scarring, right (0.1,2)d
Crusting, left (0,1,2)e
Crusting, right (0,1,2)e
Total points
a 0 = Absence of polyps; 1 = polyps in middle meatus only; 2 = polyps beyond middle meatus but not blocking the nose completely; 3 = polyps completely obstructing the nose
b Oedema: 0 = absent; 1 = mild; 2 = severe
c Discharge: 0 = no discharge; 1 = clear, thin discharge; 2 = thick, purulent discharge d Scarring: 0 = absent; 1 = mild; 2-severe
e Crusting: 0 = absent; 1 = mild; 2 = severe
202 |
|
Valerie J. Lund |
Table 24.1 c Lund-MacKay scoring system: CT scoring system |
|
|
Sinus systema |
Left |
Right |
Maxillary (0,1,2) |
|
|
Anterior ethmoids (0,1,2) |
|
|
Posterior ethmoids (0,1,2) |
|
|
Sphenoid (0,1,2) |
|
|
Frontal (0,1,2) |
|
|
Ostiomeatal complex (0 or 2 only)* |
|
|
Total points |
|
|
|
|
|
a 0 = no abnormalities; 1 = partial opacification; 2 = total opacification |
|
|
Table 24.1 d Lund-MacKay scoring system: radiological grading of anatomic variants |
|
|
|
|
Anatomic varianta |
Left |
Right |
|
|
Absent frontal sinus |
|
|
|
|
Concha bullosa |
|
|
|
|
Paradoxical middle turbinate |
|
|
|
|
Everted uncinate process |
|
|
|
|
Haller cells |
|
|
|
|
Agger nasi cells |
|
|
|
|
Total points |
|
|
|
|
|
|
|
|
|
a Scoring: 0 = no variant, 1 = variant present |
|
|
|
|
Table 24.1 e Lund-MacKay scoring system: surgery scores |
|
|
|
|
Surgerya |
Left |
Right |
|
|
Uncinectomy |
|
|
|
|
Middle meatal antrostomy |
|
|
|
|
Anterior ethmoidectomy |
|
|
|
|
Posterior ethmoidectomy |
|
|
24 |
|
Sphenoidectomy |
|
|
|
|
Frontal recess surgery |
|
|
|
|
Reduction of the middle turbinate |
|
|
|
|
Total points each side |
|
|
a Score: 0 = no procedure done; 1 = surgery done. The maximum score is 14 (7 each side)

Staging of Disease after Sinus Surgery Failure
Unfortunately the situation is more difficult once surgery has altered the anatomy of the lateral wall. Under these circumstances, it has been proposed that the presence of polyps is defined as bilateral pedunculated lesions as opposed to cobblestoned mucosa > 6 months after surgery on endoscopic examination.
■Any mucosal disease without overt polyps should be regarded as CRS.
It should be remembered that other conditions may occur concomitantly with CRS/NP and may significantly alter the prognosis, and thus the validity of staging systems, for example cystic fibrosis, gross immunodeficiency (congenital or acquired), congenital mucociliary problems (e.g. primary ciliary dyskinesia), non-invasive and invasive fungal disease, systemic vasculitis and granulomatous diseases, cocaine abuse and neoplasia.
Endoscopy
This may be performed with or without decongestion and some form of local anaesthesia. Schemes have proposed semi-quantitative scores [41] for polyps, oedema, discharge, crusting and scarring, such as that shown in Table 24.1b, which are designed to provide a baseline score and can be repeated at regular intervals following therapeutic interventions (e.g. at 3, 6, 9 and 12 months). The most important factor is the ease with which a particular staging system can be taught, performed and reproduced, and this particular one has a high inter-rater concordance [1] and can be used in the presence of recurrent disease and both prior and following revision surgery. In the system shown, which has been widely adopted, polyps are scored on a scale of 0–3. However, there are at least three other systems ranging from 0–2, 0–4 and 0–7 (Tables 24.2 and 24.3) [30, 38, 42]. Johansson showed good correlation between a 0 3 scoring system and their own system in which they estimated the percentage projection of polyps from the lateral wall and the percentage of the nasal cavity volume occupied by polyps. However, they did not find a correlation between the size of polyps and symptoms.
Imaging
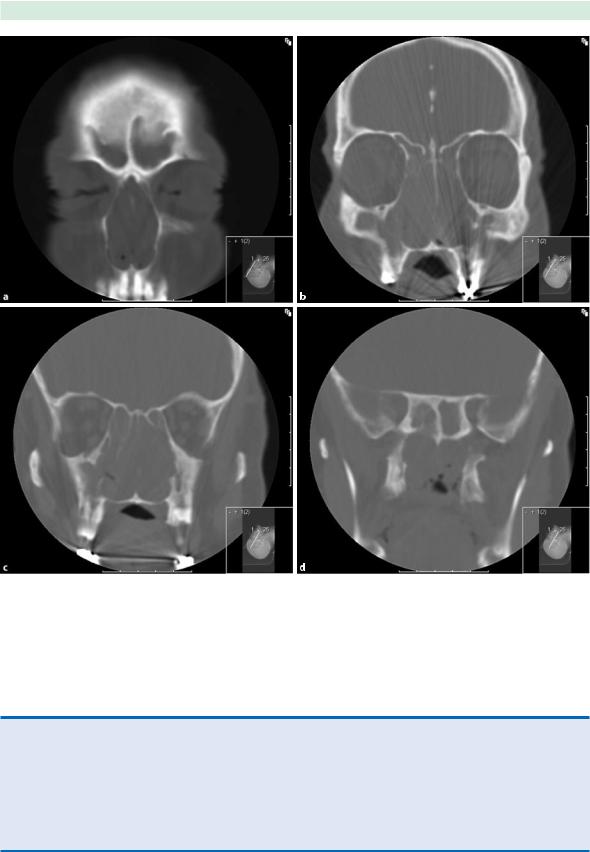
It is widely accepted that plain sinus x-rays play no part in the diagnosis and thus staging of sinus disease, and we have come to rely on CT scanning as the modality of choice in inflammation and infection (Figs. 24.1 and 24.2). It is therefore not surprising that this has proved the mainstay of staging despite the many protocols and
203
interest in reducing radiation exposure. All were originally designed with the evaluation of primary chronic disease in mind but can be adapted to the presence of recurrence. However, there are no published scoring systems for acute bacterial rhinosinusitis. At least nine systems have been published (Tables 24.1 and 24.4–24.11), some of which formulate a number of stages, usually 0–4 (e.g. Kennedy [34]), whereas others produce a score (e.g. the Lund-MacKay system [42]). This latter system has probably gained the greatest currency, largely due to its simplicity and reproducibility. However, few have specifically addressed the issue of the patient undergoing revision surgery.
The Lund-MacKay system relies on a score of 0–2 dependent upon the absence, partial or complete opacification of each sinus system and of the ostiomeatal complex, deriving a maximum score of 12 per side (Table 24.1c). It can be used following surgery, but the extent of surgical disruption will affect its application. Nonetheless, the presence of mucosal thickening and opacification of extant sinuses may still be scored. Previous surgery, such as Caldwell-Luc, may lead to permanently thickened mucosa, although this may be fibrotic rather than evidence of ongoing inflammation. However, this does not preclude the application of a numerical score in a patient whose symptoms have warranted a scan.
It should be noted that incidental abnormalities are found on scanning in up to one-fifth of the “normal” population [40]. Mean Lund-MacKay scores of 4.26 in adults [2] and 2.81 in children aged 1–18 years [25] have been reported. In addition, for ethical reasons a CT scan is generally only performed post-operatively when there are persistent problems, and therefore CT staging or scoring is best regarded as an inclusion criterion for studies rather than as an outcome assessment.
This system also allows for a radiological grading of anatomic variants (Table 24.1d), some of which may still be present post-surgery and provides a method of scoring extent of the operation itself (Table 24.1e), which again may be of use in the revision case.
The Lund-MacKay system has been validated in several studies [50] and shown to have a high interand in- tra-rater reproducibility. As a consequence it was adopted by the Rhinosinusitis Task Force Committee of the American Academy of Otolaryngology Head and Neck Surgery in 1996 [53] as well as several subsequent consensus documents and guidelines [16, 18]. CT and endoscopic scores correlate well in CRS both with and without polyps [24, 56, 60], but as previously indicated, the correlation between CT findings and symptom scores has generally been shown to be poor and is not a good indicator of outcome [9, 10, 26, 59]. However, Wabnitz and colleagues did find a correlation between a total VAS based on the sum of five sinonasal symptoms and CT score, although

204 |
Valerie J. Lund |
24
Fig. 24.1 a Coronal CT Scan – Chronic rhinosinusitis, previous endoscopic sinus surgery, b L&M Score, c R maxillary sinus 1, L maxillary sinus 1, d Posterior ethmoids R-1, L-1, e Sphenoid R-0, L-0
Staging of Disease after Sinus Surgery Failure |
205 |
Fig. 24.2 a Coronal CTScan – Chronic rhinosinusitis with nasal polyps, b Anterior ethmoids R-2, L-2, c Posterior ethmoids R-2, L-2, d Sphenoid R-2, L-2
Table 24.2 Lildholt et al. [38]: semi-quantitative scoring of nasal polyps
0None
1Cobblestoned
2Pedunculated polyps only visible endoscopically
3Pedunculated polyps not protruding below the middle turbinate (equivalent to the back of the inferior turbinate when the middle turbinate has been resected)
4Pedunculated polyps below the middle turbinate

206 |
Valerie J. Lund |
Fig 24.3 a Coronal CT scans: Chronic rhinosinusitis with previous nasal polyposis, one previous endoscopic operation, b Anterior ethmoid cavities R-2, L-2, c Posterior ethmoidal cavities R-1, L-1, d Sphenoid R-0, L-0
24

Staging of Disease after Sinus Surgery Failure |
207 |
Table 24.3 Johansson et al. [30]: semi-quantitative scoring of nasal polyps
4As before
5Polyps medial to the middle turbinate
6Polyps medial and lateral to the middle turbinate
7Nasal cavity completely filled with polyps
Table 24.4 The staging system of Friedman et al. [19]
Stage 0 |
Normal |
Stage I |
Single-focus disease (involving a single focus or sinus unit) |
Stage II |
Multifocal disease (includes bilateral or multiple areas of disease that are not conflu- |
|
ent or are diffuse throughout the ethmoid labyrinth, bilateral middle-meatal polyps) |
Stage III |
Diffuse disease (extensive bilateral involvement of multiple sinuses) without bony changes |
Stage IV |
Diffuse disease associated with bony changes |
|
|
Table 24.5 The staging system of Kennedy [34]
Stage 0 |
Normal |
Stage I |
Anatomic abnormalities |
|
All unilateral sinus disease |
|
Bilateral disease limited to ethmoid sinuses |
Stage II |
Bilateral ethmoid disease with involvement of one dependent sinus |
Stage III |
Bilateral ethmoid disease with involvement of two or more dependent sinuses on each side |
Stage IV |
Diffuse sinonasal polyposis |
|
|
Table 24.6 The staging system of Levine and May [37]
Stage 0 |
Normal |
Stage I |
Disease limited to the ostiomeatal complex |
Stage II |
Incomplete opacification of one or more major sinuses (frontal, maxillary, sphenoid) |
Stage III |
Complete opacification of one or more major sinuses, but not all |
Stage IV |
Total opacification of all sinuses |
|
|
