
Practical Plastic Surgery
.pdf
152 Practical Plastic Surgery
Table 27.1. Continued
Product |
Indications for Use |
Clinical Considerations |
Integra |
For treatment of life-threatening, |
•Provides immediate post-excis- |
|
full-thickness or deep partial- |
ional physiologic wound closure |
|
thickness skin burns where |
•Allows the use of a thin epi- |
|
sufficient autograft is not available |
dermal autograft of 0.005 inch |
|
at the time of excision or not |
•Must remain in place for 21 |
|
desirable due to the physiologic |
days before epidermal auto- |
|
condition of the patient |
grafting; must be protected |
|
|
against shearing forces and |
|
|
mechanical dislodgment |
|
|
•Contraindicated in patients with |
|
|
a known hypersensitivity to |
|
|
bovine collagen or chondroitin |
|
|
materials |
|
|
•Contraindicated in the |
|
|
presence of infection |
Epicel |
For treatment of deep dermal |
•Cultured keratinocytes can be |
(cultured |
or full-thickness wounds where |
grown in 3 weeks |
epitheilial |
sufficient donor sites are |
•Graft take varies from poor |
autografts) |
unavailable. |
to fair |
|
|
•Process is expensive |
|
|
•Grafts extremely fragile and |
|
|
may remain so for months |
|
|
after grafting |
Biobrane is a bilaminar material made of nylon mesh bonded to a thin, semipermeable silicone membrane and used as a temporary skin replacement for superficial partial-thickness burns or skin graft donor sites. It eliminates the need for dressing changes and reduces the length of inpatient treatment.
TransCyte is Biobrane with the addition of neonatal fibroblasts seeded to the collagen-coated nylon mesh. The benefits are similar to Biobrane, but TransCyte is considerably more expensive. Cultured allogeneic keratinocytes are obtained from neonatal foreskin or elective surgical specimens, and are used to cover burn wounds, chronic ulcers and skin graft donor sites. While they do not achieve wound closure, they can survive up to 30 months and produce growth factors that facilitate host
27dermal and epidermal cell proliferation and differentiation, but they are thin, fragile and require meticulous wound care to survive.
Apligraf and Dermagraft are multilaminar materials designed to overcome the fragility of cultured allogeneic keratinocytes. Apligraf is a type I bovine collagen gel with living neonatal allogeneic fibroblasts overlaid by a cornified epidermal layer of neonatal allogeneic keratinocytes, and it is used to treat chronic ulcers, pediatric burns, epidermolysis bullosa and full-thickness wounds from Mohs’ surgery pending definitive repair. Dermagraft is a cryopreserved dermal material made up of neonatal allogeneic fibroblasts on a polymer scaffold, and it stimulates ingrowth of fibrovascular tissue from the wound bed and reepithelialization from the wound edges. It is used to promote healing of chronic lesiongs and to replace lost dermal tissue beneath meshed split-thickness skin grafts on full-thickness wounds.

Skin Grafting and Skin Substitutes |
153 |
Wound Closure
Skin substitutes used for wound closure include Alloderm, Integra and cultured epithelial autografts.
Alloderm is acellular deepithelialized human cadaver dermis, which is used as a dermal graft in full-thickness or deep partial-thickness wounds. A STSG must be placed over Alloderm in a oneor two-stage procedure.
Integra is a bilaminar skin substitute made up of a cross-linked bovine collagen-glycosaminoglycan matrix coated with silicone elastomer barrier on one side. Integra is used in a two-stage procedure, in which a thin split-thickness skin graft is applied in the second stage after the silicone “epidermis” is removed. It is very reliable, with good elasticity and cosmesis, and low risk of infection, but it requires two operations and is expensive.
Epicel, or cultured epithelial autografts were developed in the 1970s, and have been used for burns, chronic leg ulcers, giant pigmented nevi, epidermolysis bullosa and large areas of skin necrosis. A one square centimeter skin harvest is expected to grow to one square meter in 21 days. Cultured epithelial autografts must be applied on a wound bed with granulation tissue or muscle fascia for proper take. Sheets are fragile, however, and often result in friable, unstable epithelium that spontaneously blisters, breaks down, and contracts long after application. Cultured epithelial autografts are also very sensitive to infection and are only able to tolerate maximum bacterial counts of 100-1000/cm2, compared to 10,000-100,000/cm2 for standard split-thickness skin grafts. Finally, cultured epithelial autografts are extremely expensive.
Pearls and Pitfalls
Over time, the vacuum-assisted closure (VAC) device is gaining a reputation as the ultimate bolster dressing. The VAC bolster dressing consists of a sponge cut in the shape of the graft, and then sealed and placed to 75-125 mmHg continuous suction. Usually, an intervening layer such as Conformant or Adaptik may be placed between the skin graft and VAC to prevent the graft from lifting off the bed when the dressing is removed. We have found that the VAC promotes graft adherence to the recipient bed and removes any accumulating serous fluid or blood. When the VAC is used correctly, STSG take will approach 100%.
Suggested Reading
1.Branham GH, Thomas JR. Skin grafts. Otolaryngol Clin North Am 1990; 27 23(5):889-97.
2.Gallico IIIrd GG. Biologic skin substitutes. Clin Plast Surg 1990; 17(3):519-26.
3.Jones I, Currie L, Martin R. A guide to biological skin substitutes. Br J Plast Surg 2002; 55(3):185-93.
4.Hauben DJ, Baruchin A, Mahler D. On the history of the free skin graft. Ann Plast Surg 1982; 9(3):242-5.
5.Petruzzelli GJ, Johnson JT. Skin grafts. Otolaryngol Clin North Am 1994; 27(1):25-37.
6.Place MJ, Herber SC, Hardesty RA. Basic techniques and principles in plastic surgery (Skin grafting). Grabb and Smith’s Plastic Surgery. 5th ed. Philadelphia: Lippincott-Raven, 1997:17-9.
7.Ratner D. Skin grafting. From here to there. Dermatol Clin 1998; 16(1):75-90.
8.Thornton JF. Skin grafts and skin substitutes. Selected Readings in Plastic Surgery. 2004; 10(1):1-24.
Chapter 28
Burns: Initial Management and Resuscitation
Baubak Safa and Mark Sisco
Epidemiology
Of the 2-3 million thermal injuries that occur in the United States each year, approximately 100,000 require hospital admission to a burn unit. Furthermore, 5,000-6,000 people die as a direct result of thermal injury in this country. Although thermally injured patients require 1-1.5 days in the hospital per percent total body surface area (TBSA) burned, this period only represents a small fraction of the total treatment for these patients which also includes rehabilitation and physical therapy, reconstruction and readaptation.
Burn victims tend to reflect four general populations: The very young, the very old, the very unlucky and the very careless. Indeed, National Burn Information Exchange (NBIE) data indicate that up to 75% of burn injuries result from the victim’s own actions.
Scald burns represent the most common burns in the United States. Fifty percent of these burns occur in children in the kitchen, followed by burns from hot water in the bathroom. The burn depth is directly proportional to the time of exposure of the hot liquid and therefore, this aspect of the history is important in evaluating a burn patient. Many adult scald burns are also caused by automobile radiator injuries.
Heating unit failure is the most common cause of residential fires. The requirement of smoke detectors in new construction buildings has resulted in increased warning time and a decreased chance of death. A key part of the history in patients involved in residential fires is the presence or absence of ignition of their clothing. Full-thickness burns are six times more likely when clothing ignition is present. Furthermore, mortality increases approximately four times when clothing is ignited.
The Burn Wound
There are three zones of burn. The zone of coagulation is the central area and is composed of nonviable tissue. The zone of stasis surrounds the central zone of coagulation. The adequacy of the initial burn resuscitation will affect the extent and outcome of this zone. Typically, blood flow is initially present, but ischemia and hypoperfusion prevail in the subsequent 24 hours, especially with inadequate resuscitation. The zone of hyperemia surrounds the zone of stasis and contains viable tissue.
Burn depth, along with the extent of the burn (TBSA) and age of the patient, are primary determinants of mortality following thermal injury. The depth of injury is also a major determinant of a patient’s long term function and appearance. The varying depth of a burn as well as the changing perfusion of the zone of stasis render the precise determination of burn depth difficult in the first 24 to 48 hours. Therefore, the most accurate method of determining the depth of burn is clinical assessment based on experience.
Practical Plastic Surgery, edited by Zol B. Kryger and Mark Sisco. ©2007 Landes Bioscience.

Burns: Initial Management and Resuscitation |
155 |
Burn Classification
Superficial Burns (First Degree)
Superficial burns are easily diagnosed. The typical superficial burn is a bad sunburn with erythema and mild edema. The area involved is tender and warm to the touch and there is rapid capillary refill. Topical antimicrobial therapy is unnecessary and all layers of the epidermis and dermis are intact. Healing should occur within five to seven days and some superficial epidermolysis may be seen. These burns are not included in the assessment of the TBSA of a burn victim.
Partial-Thickness Burns (Second Degree)
Partial-thickness burns may involve a wide spectrum of dermal injury and present a diagnostic dilemma. Superficial partial-thickness burns involving the uppermost layers of the dermis may only be slightly more serious than a superficial burn. A deep partial-thickness burn, however, may behave in a similar fashion to a full-thickness burn and require excision and grafting. The formation of blisters is the hallmark of partial-thickness burns and implies some integrity of deeper dermal layers. Other signs of dermal viability include blanching with pressure and capillary refill. These signs may be absent in deep partial-thickness burns, and there may be a red-and-white reticulated appearance after blister debridement. In general, if complete reepithelialization is not expected within three weeks, or if the resulting wound will lead to contractures or a less-than-ideal cosmetic appearance, excision and skin grafting is performed.
Full-Thickness Burns (Third Degree)
Full-thickness burns have an easily recognizable appearance and may extend into fat, fascia, muscle and even bone. There is complete destruction of all epidermal and dermal elements and the wounds are insensate. The patient, therefore, has little or no discomfort. The burn wound is leathery, waxy, or translucent and thrombosed vessels may be visible beneath the skin. All full-thickness burns need surgical excision and skin grafting.
Burn Triage
The American Burn Association has defined the criteria used in triaging burns to be admitted and treated in a specialized burn unit:
•Partialand full-thickness burns >10% TBSA in patients under 10 or over 50 years of age
•Partialand full-thickness burns > 20% TBSA in other age groups
• Full-thickness burns >5% TBSA in any age group |
28 |
•Partialand full-thickness burns involving the face, hands, feet, genitalia, perineum, or major joints
•Electric burns, including lightning injury
•Chemical burns with serious threat of functional or cosmetic impairment
•Inhalation injuries
•Any burn patient with concomitant trauma
•Lesser burns in patients with preexisting medical problems that could complicate management
•Combined mechanical and thermal injury in which the burn wound poses the greater risk
•Any case in which abuse or neglect is suspected

156 |
Practical Plastic Surgery |
On admission and initial evaluation, the burn victim is treated as any trauma patient and is evaluated for the “ABCs” (Airway, Breathing and Circulation). Large-bore peripheral IVs are placed in unburned skin. In patients who will likely need invasive hemodynamic monitoring, a central venous catheter, pulmonary arterial or Swan-Ganz catheter, or a peripheral arterial catheter may be used.
One should have a low threshold for endotracheal intubation especially if inhalational injury is suspected. Facial burns, for example, can lead to severe edema rendering later intubation extremely difficult or impossible thereby necessitating a surgical airway. Once airway, ventilation and systemic perfusion have been established, the next priority is diagnosis and treatment of concomitant life-threatening injuries. The patient’s tetanus status should also be obtained and updated if necessary.
If inhalational injury is suspected, early intubation is necessary to prevent respiratory distress, especially if the patient is being transferred to a burn center. The physician must maintain a high degree of suspicion for the presence of inhalational injury. If it is suspected, arterial blood gases and carboxyhemoglobin (CHgb) levels should be obtained. If CHgb levels are elevated (>10%), 100 percent oxygen must be administered.
Burn Resuscitation
Burn Shock
Burn shock develops from hypovolemia and cellular breakdown. This type of shock is characterized by decreased cardiac output and plasma volume, increased extracellular fluid and edema and oliguria.
Fluid Resuscitation
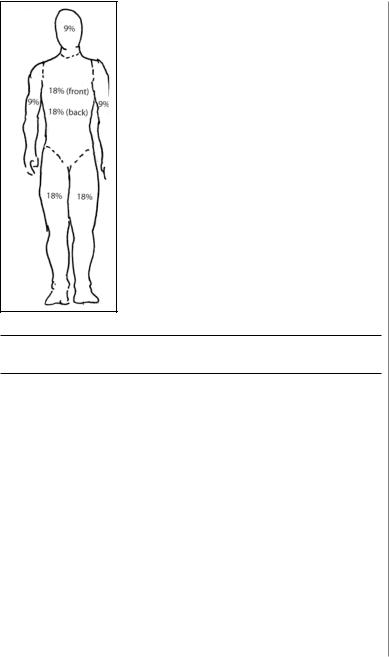
The volume of fluid needed for resuscitation depends on both the area and the depth of burn. The “rule of nines” is a simple and relatively accurate method of estimating TBSA burned in adults (Fig. 28.1). The goal of fluid replacement is to restore and maintain adequate tissue perfusion and oxygenation, prevent organ ischemia, save as much of the zone of stasis as possible, and minimize the iatrogenic contribution to edema. Various fluid replacement protocols have been described in caring for the burn patient. It is important to keep in mind that these formulas are merely a starting point and that precise monitoring of the patient’s status should be used to fine-tune fluid replacement. Urine output remains an excellent guideline for the adequacy of fluid replacement. An output of 30-50 ml/hour for adults and greater than 1.0 ml/kg/hour for children is used as a guideline for adequate fluid resuscitation. Central venous
28pressure and Swan-Ganz monitoring can also be used to fine-tune resuscitation, especially in elderly patients with preexisting cardiopulmonary pathology.
In pediatric burn patients, the Lund and Bowder chart or the Berkow formula are used for establishing the extent of burn injury (Table 28.1).
The Parkland Formula is the most widely used method for calculating resuscitation volume. It is simple, safe and inexpensive. This formula calls for 4 mL/kg/% TBSA of Lactated Ringer’s solution over the first 24 hours of injury. Half of this volume is given over the first eight hours and half over the next 16 hours after injury. It is important to keep in mind that the volume calculated is to be given from the time of injury and not from the time of initial evaluation of the patient.
Parkland Formula
[0.5 (4 mL kg % TBSA)] / 8 hr = mL/hr (first eight hours) [0.5 (4 mL kg % TBSA)] / 16 hr = mL/hr (next sixteen hours)
Burns: Initial Management and Resuscitation |
157 |
Figure 28.1. “Rule of Nines” for estimating percent
TBSA in adults.
Table 28.1. The Berkow formula for calculating percent TBSA in children and adolescents
Site |
Age (years): |
<1 |
1-4 |
5-9 |
10-14 |
15+ |
|
|
|
Head |
|
19 |
17 |
13 |
11 |
9 |
|
|
|
Neck |
|
2 |
2 |
2 |
2 |
2 |
|
|
|
Trunk (anterior) |
13 |
13 |
13 |
13 |
13 |
|
|
||
Trunk (posterior) |
13 |
13 |
13 |
13 |
13 |
|
|
||
Buttocks |
|
5 |
5 |
5 |
5 |
5 |
|
|
|
Genitalia |
|
1 |
1 |
1 |
1 |
1 |
|
|
|
Right upper arm |
4 |
4 |
4 |
4 |
4 |
|
|
||
28 |
|||||||||
Right forearm |
|
3 |
3 |
3 |
3 |
3 |
|
||
|
|
|
|||||||
Right hand |
|
2.5 |
2.5 |
2.5 |
2.5 |
2.5 |
|
|
|
Left upper arm |
4 |
4 |
4 |
4 |
4 |
|
|
||
Left forearm |
|
3 |
3 |
3 |
3 |
3 |
|
|
|
Left hand |
|
2.5 |
2.5 |
2.5 |
2.5 |
2.5 |
|
|
|
Right thigh |
|
5.5 |
6.5 |
8 |
8.5 |
9 |
|
|
|
Right leg |
|
5 |
5 |
5.5 |
6 |
6.5 |
|
|
|
Right foot |
|
3.5 |
3.5 |
3.5 |
3.5 |
3.5 |
|
|
|
Left thigh |
|
5.5 |
6.5 |
8 |
8.5 |
9 |
|
|
|
Left leg |
|
5 |
5 |
5.5 |
6 |
6.5 |
|
|
|
Left foot |
|
3.5 |
3.5 |
3.5 |
3.5 |
3.5 |
|
|
|
|
|
|
|
|
|
|
|
|
|

158 |
Practical Plastic Surgery |
Colloid Therapy
The timing of colloid therapy remains highly controversial. Plasma proteins counteract the outward hydrostatic force in the capillaries by generating an inward oncotic force. Massive interstitial edema occurs in many burn patients after the leaking of plasma fluid into and around the burned tissue. Albumin is the most commonly used colloid infusion. Although the precise amount of protein needed is not known, experience has shown that infusions at a constant rate seem superior to bolus administration. It is important to note that protein administration does not decrease burn edema but does limit edema in nonburned tissues and maintains intravascular volume better than crystalloid infusion. The exact protocol for administration of protein infusions varies widely between burn centers. In our burn unit, crystalloid is given in the first 8 hours, and protein infusions are initiated 8-12 hours after injury.
Other nonprotein colloid solutions available include dextran and hetastarch. Dextrans are colloids consisting of glucose molecules polymerized to form high-molecular-weight polysaccharides. Dextran has an osmotic effect and consequently increases urine output. When using dextran, therefore, urine output cannot be used to judge the adequacy of resuscitation. Hetastarch is an alternative to dextran and has volume expanding properties similar to a 6% protein solution. Furthermore, hetastarch has been used successfully as colloid administered during the second 24 hours of burn resuscitation.
Escharotomy
Thick, leathery eschar from a circumferential burn to the upper and lower extremities or trunk can be lifeor limb-threatening. A circumferential eschar on the extremities can cause severe constriction resulting in compartment syndrome, ischemia and necrosis. This phenomenon is worsened by massive capillary leak and edema caused by a deep partialor full-thickness burn. In a similar fashion, constricting eschar in the region of the trunk may cause decreased chest wall excursion and an inability to adequately ventilate the patient due to high peak inspiratory pressures.
In the extremities, peripheral perfusion can be easily assessed using a Doppler apparatus. Alternatively, transcutaneous oxygen saturation can be used to assess peripheral oxygenation. Typically, an oxygen saturation of less than 95 percent correlates with a need for emergent escharotomy. The need for chest escharotomies can be assessed by noting increased peak inspiratory pressures on a ventilator or more simply, limited chest excursion on physical examination.
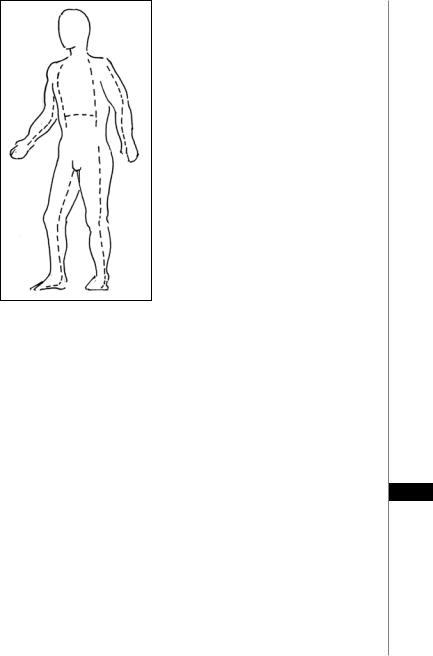
If chest wall excursion is limited, escharotomies should be performed bilaterally
28in the anterior axillary lines using either an electrocautery device or a scalpel. These escharotomies may be joined with a chevron-shaped incision over the costal margin if needed. Extremity escharotomies are done in the mid-lateral lines of the affected limb. The location of the ulnar nerve in the upper extremity (posterior to the medial epicondyle) and the common peroneal nerve in the lower extremity (posterior to the fibular head) should be noted and extreme care should be taken to avoid injury to these structures. Finger escharotomies are done on the mid-lateral lines as well. Such a release is performed on the ulnar aspects of the index, middle and ring fingers and on the radial aspect of the thumb and small finger to avoid an incision over the “working surface” of these digits. Escharotomies may also be performed over the thenar and hypothenar muscles if necessary. In deep hand burns, escharotomies are performed over the dorsum of the hand, and the interosseous compartment fasciotomies are performed through the same incisions. Typically two longitudinal
Burns: Initial Management and Resuscitation |
159 |
Figure 28.2. The commonly used escharotomy sites.
incisions (over the second and fourth metacarpals) are sufficient for release of all compartments. Figure 28.2 illustrates the commonly used escharotomy sites.
Escharotomies should be performed through the entire length of an eschar, from normal to normal skin since even a small area of remaining circumferential constriction can lead to peripheral ischemia. Typically, an obvious release of the underlying soft tissue indicates an adequate incision. Inadequate fluid resuscitation or the need for compartment fasciotomies should be suspected in patients in whom sufficient release of a constricting eschar fails to lead to a return of peripheral perfusion.
Rarely, aggressive fluid resuscitation may lead to a massive accumulation of intraor retroperitoneal fluid. This phenomenon has been observed, for example, in patients with previous intra-abdominal pathology such as chronic pancreatitis. In such patients, one should have a high index of suspicion for the development of abdominal compartment syndrome (ACS). Elevated peak inspiratory, bladder and central venous
pressures as well decreased urine output are suggestive and if diagnosed, immediate 28 abdominal myofascial release should be performed. The development of abdominal compartment syndrome portends a very poor prognosis in the burn patient.
Burn Wound Care
After initial resuscitation of the burn patient, debridement and wound care is commenced in the burn unit. This is typically done in a heated hydrotherapy room with access to warm water to minimize heat loss. At this time, any loose skin and blisters are debrided and topical agents are applied. Effective debridement of burn eschar increases penetration of topical agents, improves time-to-healing for partial-thickness burns, and may allow faster skin graft coverage of full-thickness burns. Administration of appropriate analgesia, oral or intravenous, is extremely important during the debridement process. A variety of topical antibiotics are available for application to burn wounds.

160 |
Practical Plastic Surgery |
Xeroform/Bacitracin
A combination of xeroform and bacitracin is commonly used for superficial par- tial-thickness burns. This application has the advantage of being relatively inexpensive and widely available and is applied on a daily basis until reepithelialization has occurred.
Silver Sulfadiazine
Silver sulfadiazine is the most widely used topical agent for deep partial-thickness burns or partial-thickness burns of indeterminate depth as well as full-thickness burns. It can be applied either daily or twice daily. In vitro studies have shown silver sulfadiazine to be active against gram-positive and gram-negative bacteria, and Candida albicans. Minimal pain is associated with its application and in fact, many patients find it soothing when applied to partial-thickness burns. The formation of a pseudoeschar is one detriment of silver sulfadiazine and may render determination of burn depth difficult. Other downsides of its use include leukopenia and the possibility of induction of resistant organisms such as Pseudomonas aeruginosa or Enterobacteriaceae.
Silver Nitrate
Silver nitrate has significant antimicrobial properties and is nontoxic in its most commonly used formulation. It is important to keep in mind, however, that gram-negative bacteria and some gram-positive bacteria may reduce silver nitrate to silver nitrite which can lead to methemoglobinemia in rare cases. It is active against gram positive and some gram negative bacteria, such as Pseudomonas aeruginosa, and is now commonly incorporated into commercially available wound care products.
Mafenide (Sulfamylon)
Mafenide has a broad antibacterial spectrum and has the best eschar penetration of any available agent. Due to its efficient penetration of cartilage, it is used over cartilaginous areas such as the nose or the ear. It is usually applied twice daily and due to its action as a carbonic anhydrase inhibitor may cause a metabolic acidosis if applied to large surface areas. Of the silver containing products, Sulfamylon is the most painful to the patient.
Inhalation Injury
Currently, inhalation injury is a more common acute cause of death from a burn injury than the surface burns themselves. The mechanisms of injury may involve carbon monoxide inhalation, thermal injury to the upper airway and digestive tract,
28 and inhalation of the products of combustion.
Carbon Monoxide Poisoning
Carbon monoxide (CO) is a tasteless, odorless gas. It preferentially binds to hemoglobin and displaces oxygen from the hemoglobin molecule thereby impairing tissue oxygenation. The major deleterious effects of carbon monoxide result from its displacement of oxygen. It is estimated that it has more than 200 times the affinity for hemoglobin than oxygen.
Thermal Injury to the Upper Airway
The most common cause of direct thermal injury to the upper airway is inhalation of steam. This is because steam has 4000 times the heat-carrying capacity of air. Edema of the face and perioral tissues can result in narrowing of the airway and increased

Burns: Initial Management and Resuscitation |
161 |
work of breathing. In addition to direct thermal injury to the airway, edema of the airway often parallels the generalized edema in a burn patient. Therefore, airway protection should always be kept in mind in a patient with severe generalized burn edema.
Inhalation of Products of Combustion
Inhalation of aldehydes, ketones and organic acids, all products of combustion, is the most significant component of inhalation injury. All of the above chemicals cause significant chemical injury to the respiratory tract and mimic aspiration of acidic gastric contents. Increased capillary permeability and alveolar injury may lead to pulmonary edema and ultimately adult respiratory distress syndrome (ARDS). Secondary pneumonias may develop after plugging of the lower airways with sloughed bronchial mucosa. Patients with secondary pneumonias after inhalation injury have a poor prognosis.
Diagnosis
A history of a flame burn in an enclosed space, singed nasal hairs and facial or oropharyngeal burns, and the presence of carbonaceous sputum should raise suspicion of an inhalation injury. CHgb levels should be obtained in all patients with such findings. Levels above 10% are significant and denote inhalation injury and levels above 50% are associated with a high likelihood of death. A patient with documented inhalation injury should be immediately placed on 100% oxygen therapy which reduces the washout time of carbon monoxide. Fiberoptic bronchoscopy of the upper respiratory tract is the gold standard for diagnosis and may show edema of the vocal cords and charring, sloughing, or edema of the hypopharyngeal and upper tracheal mucosa
Management
The management of inhalation injury is primarily supportive care. Endotracheal intubation should be performed liberally due to the potentially disastrous consequences of a delay in diagnosis. If carbon monoxide poisoning is present, 100% oxygen is administered. Furthermore, the airway can be cleared of mucosal plugs and airway debris by aggressive pulmonary toilet and bronchoscopy.
Nutrition
Proper nutrition in the burn patient is of the utmost importance. A major burn results in a hypermetabolic state that is even more profound than that found in the stress response to trauma and sepsis. Enteral nutrition should be used whenever possible, and therefore a feeding tube should be inserted immediately in patients 28 with major burns. This is important in light of the fact that delayed placement of a post-pyloric feeding tube is often extremely difficult. It is also important to keep in mind that large burns are also associated with a transient ileus. The precise calcula-
tions in basal energy expenditures and caloric requirements are beyond the scope of this text, but the inclusion of a nutritionist as part of the multi-disciplinary approach to the management of the burn patient is extremely important. Finally, ulcer prophylaxis should also be considered in all patients with large burns.
Pearls and Pitfalls
•If not treated rapidly and adequately, the central area of the burn, the zone of coagulation, can progress and enlarge. This occurs because the surrounding zone
