
мошонка, мочевой пузырь уретра
.pdf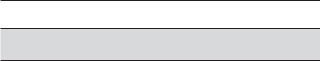
CH A P TER |
Lower Genitourinary |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Scrotum
Bladder
Urethra
Penis
Prostate
For Key Features summary see p. 188
SCROTUM
Sonography is the primary method used to image the scrotum. Patients are usually examined in the supine position. A towel can be draped between the thighs to help support the scrotum. Warm gel should always be used because cold gel can elicit a cremasteric response and the resulting scrotal thickening makes it very difficult to perform a thorough examination.
The normal testes appear as homogeneous ovoid organs that are symmetric bilaterally. The normal testis measures 4 to 5 cm in length, 2 to 3 cm in width, and 2 to 2.5 cm in depth. The normal volume of the testis using the formula for an ellipsoid (length ×width × depth × 0.53) is
15 to 20 mL. Testicular size decreases with age. The seminiferous tubules converge to form the rete testes, which is located at the testicular mediastinum. The mediastinum itself appears as a peripherally located, elongated hyperechoic structure (Fig. 6-1A and B). The rete testes connects to the epididymal head via the efferent ductules. The head of the epididymis is semilunar with rounded edges, and its echogenicity is similar to that of the testis (see Fig. 6-1C). It rests directly on the upper pole of the testis and should be seen in almost all men. It continues inferiorly into the body and tail of the epididymis, which are hypoechoic to the testis (see Fig. 6-1D and E). The body and tail of the epididymis are more difficult to identify than the head, but, with practice, they can usually be seen along the anterolateral or posterior aspect of the testis.
The vascular supply of the testis is shown in Figure 6-2. Unlike other organs, the major arteries of the testis are located peripherally and are called capsular arteries. They supply blood to the testicular parenchyma by means of branches called centripetal arteries. The centripetal arteries enter the testis and travel toward the mediastinum. As they approach the mediastinum, they branch into recurrent rami that curve away from the mediastinum. In approximately 50% of testes, one or more major branches of the testicular artery enter the testis through the mediastinum. These transmediastinal arteries are often large enough to be seen by gray-scale sonography, and a transmediastinal vein often accompanies them. Like other solid parenchymal organs, the testicular arterial waveforms have a low resistance pattern. The veins of the testis drain through the mediastinum as well as through the capsule of the testis. They are more difficult to visualize than the arteries, but with continued improvement in Doppler sensitivity they are being seen with more regularity. Blood flow may or may not be seen in the normal epididymis, but it should not be as vascular as the testis. (See Table 6-1 for a summary of the characteristics of normal testes.)
One of the major roles of sonography is the evaluation of scrotal masses, and the most important determination is whether the mass is inside or outside the testis. The vast majority of extratesticular masses are benign, but intratesticular masses are much more likely to be malignant. In addition to location, it is also important to determine whether the mass is cystic or solid, whether it has detectable internal vascularity on color Doppler imaging, and whether it is palpable (Box 6-1).
The most common scrotal mass is the spermatocele. These are cystic lesions that form in the head of the epididymis and are filled with spermatozoa-containing fluid (Fig. 6-3). Low-level echoes can be seen in the lumen of some spermatoceles, especially when the gain is increased. Septations are occasionally seen with large
152
Lower Genitourinary |
153 |
A B C
D E F
Figure 6-1 Normal scrotal anatomy. A, Transverse view of the testis shows normal homogeneous echogenicity throughout with the exception of the peripherally located hyperechoic mediastinum (arrow). B, Longitudinal view of the testis shows the mediastinum (arrow) as an elongated hyperechoic structure. C, Longitudinal view shows the upper pole of the testis and the head of the epididymis (H). The head of the epididymis and testis have similar echogenicities. D, Longitudinal view shows the body of the epididymis (*) located posterior to the testis. E, Longitudinal view shows the head (H) and body (*) of the epididymis. Note that the body is less echogenic than the head. In this case the body of the epididymis is located anteriorly. F, Transverse view of the right testis shows the hypoechoic epididymal body (*) located along the anterior lateral aspect of the testis.
spermatoceles. Epididymal cysts may also form in the epididymal head as well as the body and tail. They contain serous fluid and are anechoic and indistinguishable from spermatoceles. Both are benign lesions that rarely produce symptoms other than those related to the mass effect. Cystic lesions are extremely common, and at least a small spermatocele can be seen in more than 70% of scans.
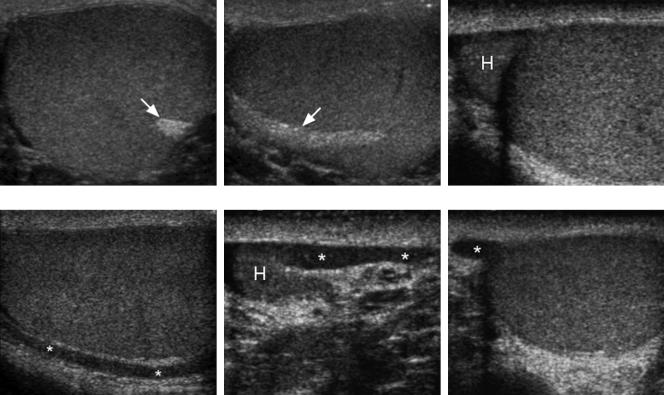
Hydroceles are collections of fluid that form in the potential space of the tunica vaginalis. Most large hydroceles are idiopathic. A variety of conditions, including scrotal inflammatory processes, testicular torsion, and testicular tumors, can cause small to moderate hydroceles. Although variable, hydroceles usually occur in the anterior aspect of the scrotum and displace the testis posteriorly (Fig. 6-4A and B). Crystals can precipitate in hydrocele fluid and produce mobile low-level reflectors
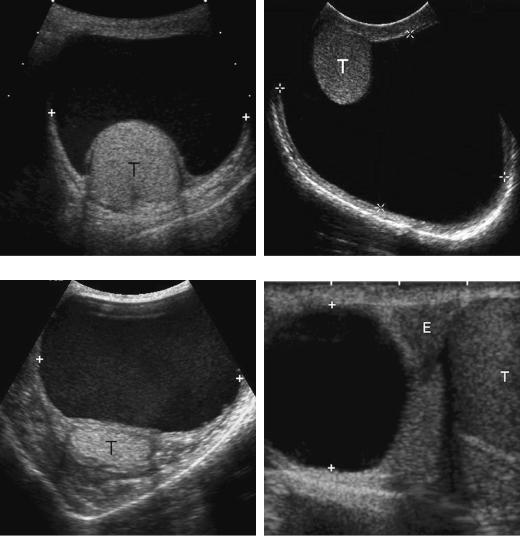
(see Fig. 6-4C). When hydroceles are large and the testis is compressed posteriorly, it can be difficult to obtain high-resolution views of the testes. This can be overcome by positioning the transducer posteriorly to get closer to the testes. Rarely, hydrocele fluid will accumulate in the spermatic cord in an unobliterated portion of the tunica vaginalis. This type of hydrocele will appear superior to the testis and is referred to as a funiculocele or a hydrocele of the cord. It can be distinguished from a spermatocele because it does not arise from the epididymis (see Fig. 6-4D). Pyoceles and hematoceles are hydroceles that are complicated by infection or hemorrhage. They appear as complex collections with internal echoes and septations and often in conjunction with scrotal wall hyperemia (Fig. 6-5). They should be suspected on the basis of combined clinical and sonographic features.

154 ULTRASOUND: THE REQUISITES
A B C
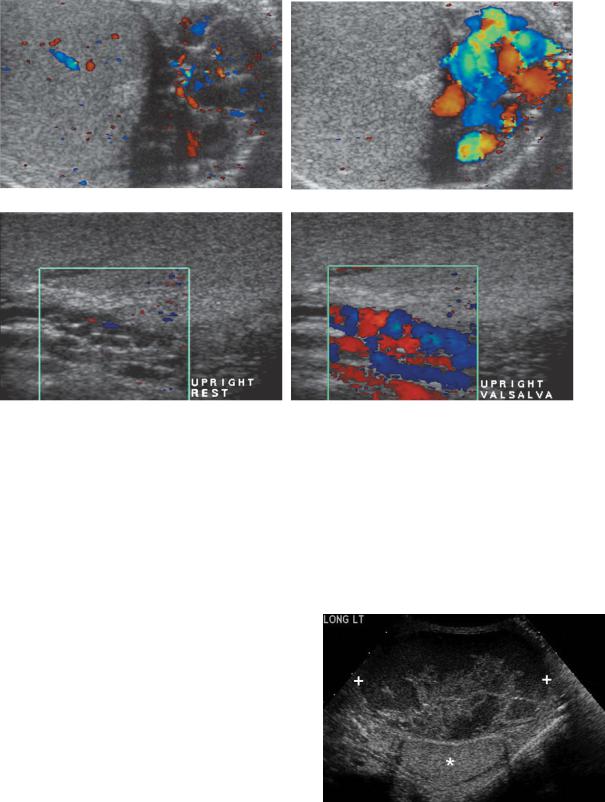
Figure 6-2 Testicular vascular anatomy. A, Transverse color Doppler view shows a peripherally located capsular artery (black arrows) supplying several centripetal arteries (white arrowheads). Several recurrent rami (white arrows) are seen arising from the centripetal arteries. M, mediastinum. B, Transverse color Doppler view of a different patient shows a large transmediastinal artery (*) passing through the mediastinum (M) and traveling to the opposite side of the testis. An adjacent transmediastinal vein (black arrowhead) is also seen. A centripetal artery (white arrowhead), recurrent ramus (white arrow), and a capsular artery (black arrow) are also seen. C, Grayscale view of a different patient shows a transmediastinal artery (*) as well as vein (arrowhead) and their relationship to the mediastinum (M).
Table 6-1 Characteristics of a Normal Testis
Characteristic |
Appearance |
|
|
Echogenicity |
Medium level (except echogenic mediastinum) |
Texture |
Homogeneous |
Surface |
Smooth |
Vascularity |
Largest vessels on surface |
Size |
15-20 mL (average 4-5 × 2-3 × 2-3 cm) |
|
|
Box 6-1 Appearance of Scrotal Lesion
versus Chance of Neoplasm
FACTORS THAT DECREASE |
FACTORS THAT INCREASE |
CHANCE OF NEOPLASM |
CHANCE OF NEOPLASM |
Extratesticular |
Intratesticular |
Nonpalpable |
Palpable |
Simple cystic appearance |
Solid or complex cystic |
No detectable vascularity |
Detectable internal |
|
vascularity |
A B C
Figure 6-3 Spermatoceles in different patients. A, Longitudinal view of the epididymal head shows a small spermatocele (cursors). B, Longitudinal view shows a moderate-sized spermatocele (cursors). C, Longitudinal view shows a large spermatocele (cursors) that makes it difficult to visualize the adjacent epididymal head.
Lower Genitourinary |
155 |
A B
C D
Figure 6-4 Hydroceles in different patients. A, Transverse view shows a large anechoic hydrocele (cursors) surrounding the testis (T). B, Transverse view shows a large hydrocele (cursors) surrounding the testis (T). This case is unusual because the testis is located anteriorly. C, Transverse view shows a hydrocele (cursors) with diffuse low-level echoes. The testis (T) is seen posteriorly. D, Longitudinal view shows a cystic lesion (cursors) in the scrotum located superior to the epididymal head (E). This is the expected location and appearance of a hydrocele of the spermatic cord.
Varicoceles are dilated peritesticular veins that form as the result of incompetent valves in the spermatic veins. The left spermatic vein drains into the left renal vein and the right spermatic vein drains into the inferior vena cava. Because the superior mesenteric artery compresses the left renal vein, the pressure on the left side is higher than that on the right, and this presumably explains why 85% of the varioceles are on the left. Most of the remaining 15% are bilateral. It is so unusual to have an isolated right-sided varicocele that compression of the right spermatic vein by retroperitoneal masses, or situs inversus should be considered whenever one is detected.
Although the yield is very low, a sonographic survey of the upper abdomen should be performed whenever an isolated right-sided varicocele or an unusually large and asymmetric right-sided varicocele is detected.
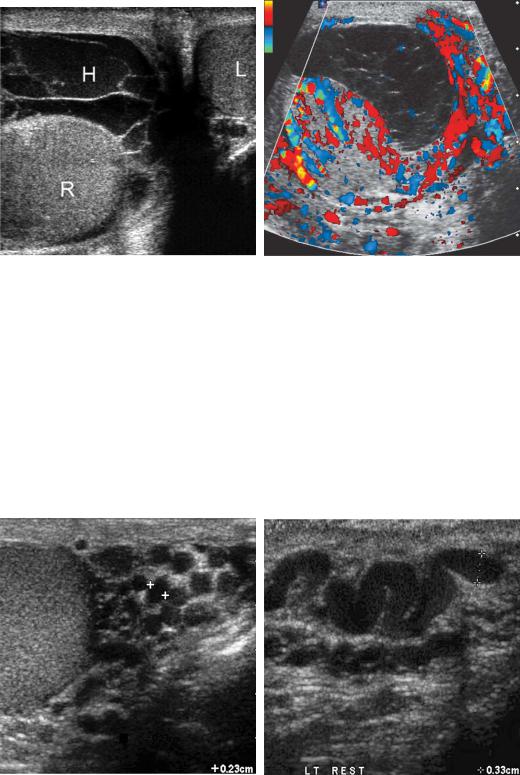
Varicoceles generally do not cause pain or discomfort until they become large. However, even small nonpalpable varicoceles can potentially cause infertility. Therefore, a search for varicoceles is important in the evaluation of an infertile couple. Gray-scale sonography depicts varicoceles as numerous, dilated, tortuous, tubular channels in the peritesticular tissues (Fig. 6-6). They are usually located lateral, posterior and/or superior to the testis.
156 ULTRASOUND: THE REQUISITES
A B
Figure 6-5 Complicated hydroceles in different patients. A, Transverse view of the scrotum shows a complex multi-septated hydrocele (H) containing low-level echoes. The right (R) and left (L) testes are also seen. This was a post-traumatic hematocele. B, Color Doppler view of the scrotum in a different patient with epididymitis shows a multi-septated collection in the scrotal sac with peripheral hyperemia. This is consistent with a pyocele.
Rarely, varicoceles will involve intratesticular veins. The upper limit of normal for the caliber of scrotal veins is 2 mm. At rest, blood flow in varicoceles is occasionally visible on gray-scale sonography, but it is usually too slow to be detected with color Doppler imaging. However, when the patient performs a Valsalva maneuver,
the incompetent valves in the spermatic vein allow rapid retrograde blood flow into the pampiniform plexus, and this is detectable on color Doppler imaging (Fig. 6-7). In most patients this Valsalva-induced flow augmentation is readily detectable when the patient is supine. If the examination is normal with the patient supine, then the
A B
Figure 6-6 Varicoceles in different patients. A, Transverse view of the left testis shows multiple cystic-appearing spaces (cursors) lateral to the testis. During real-time scanning these could be shown to communicate with each other and are consistent with peritesticular veins. They all measure slightly greater than 2 mm in diameter (cursors). B, Longitudinal view of the left scrotum shows a tortuous vein lateral to the left testis (cursors). At rest, this vein measured 3.3 mm in diameter.
Lower Genitourinary |
157 |
A B
C D
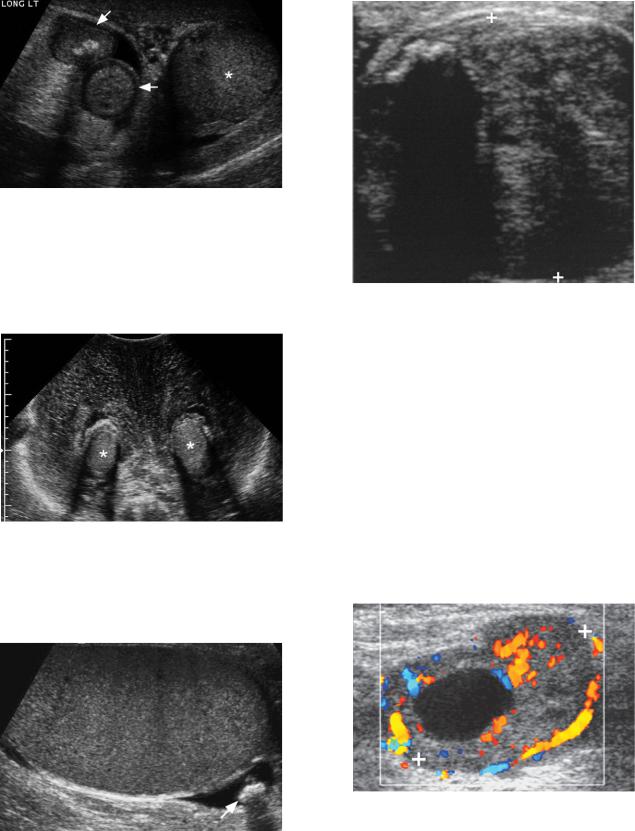
Figure 6-7 Varicoceles in different patients. A and B, Transverse color Doppler views of the left scrotum at rest (A) and during Valsalva maneuver (B) show dilated peritesticular veins with little detectable flow at rest but readily detectable augmented venous flow during Valsalva maneuver. C and D, Longitudinal views in the upright position at rest (C) and during Valsalva maneuver (D) show minimally dilated veins posterior to the testis that have augmented venous flow during Valsalva maneuver.
study should be repeated with the patient upright because the increased hydrostatic pressure may accentuate the varicocele’s appearance. Short-duration Valsalva augmented peritesticular venous flow can occasionally be seen in normal men. The diagnosis of a varicocele should be made when the Valsalva-augmented flow is persistent (greater than 1 second) or the veins are dilated on gray-scale sonography.
Spermatoceles, hydroceles, and varicoceles account for the majority of extratesticular scrotal masses, and this explains why most extratesticular masses are benign. Other non-neoplastic peritesticular masses include exuberant scars, sperm cell granulomas, chronic hematomas (Fig. 6-8), hernias (Fig. 6-9), scrotal wall edema (Fig. 6-10), and scrotoliths (Fig. 6-11). Extratesticular tumors occur but are rare. The most common is the adenomatoid tumor. It is a benign lesion that arises
Figure 6-8 Scrotal hematoma. Longitudinal view of the left scrotum shows the testis posteriorly (*). A large complex fluid collection (cursors) with internal membranes and solid-appearing components is identified. This patient had undergone a hernia repair, and this is a typical appearance of an evolving hematoma.
158 ULTRASOUND: THE REQUISITES
Figure 6-9 Hernia. Longitudinal view of the left scrotum shows the testis inferiorly (*) and a hernia sac containing loops of small bowel (arrows) superiorly. The typical target appearance of the small bowel is apparent, and peristalsis could be seen on real-time examination.
Figure 6-12 Leiomyosarcoma. Longitudinal view in the region of the spermatic cord shows a heterogeneous solid mass (cursors) with an area of shadowing calcification superiorly. Because of its size and appearance this was resected and shown to be a leiomyosarcoma.
Figure 6-10 Severe scrotal edema. Transverse view of the scrotum shows the right and left testis (*) surrounded by markedly thickened scrotal wall bilaterally.
from the epididymis or the tunica vaginalis and varies in its ultrasound appearance. Benign and malignant soft tissue tumors (lipomas/liposarcomas, leiomyomas/ leiomyosarcomas) can arise in the scrotum (Fig. 6-12) and metastases can also develop in the scrotum (Fig. 6-13). Neoplasms should be suspected when large solid or complex masses are seen in the peritesticular region.
Intratesticular cysts are much less common than spermatoceles. Nonetheless, reports indicate that they can
Figure 6-11 Scrotolith. Longitudinal view shows a small shadowing scrotolith (arrow) in the inferior aspect of the scrotum posterior to the testis.
Figure 6-13 Scrotal metastasis. Longitudinal color Doppler view in the left supratesticular region shows a solid mass (cursors) with an internal cystic region and readily detectable internal and peripheral blood flow. Further evaluation in this patient showed peritoneal nodules and a supraclavicular node. The patient was subsequently shown to have metastatic bronchogenic carcinoma.
Lower Genitourinary |
159 |
A B
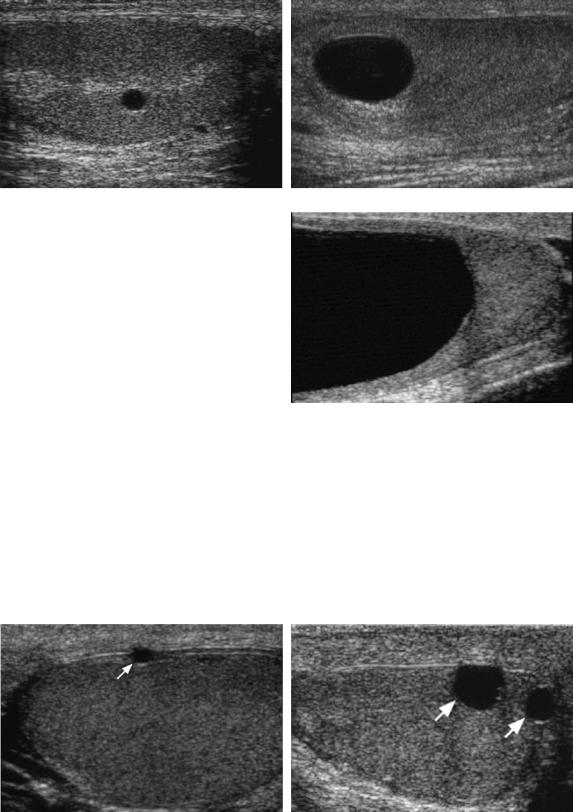
Figure 6-14 Testicular cysts in different patients. A, Longitudinal view shows a small testicular cyst adjacent to the mediastinum. B, Longitudinal view shows a moderate-size testicular cyst. C, Longitudinal view shows a large testicular cyst. Despite its size, this cyst was not palpable as a distinct lesion in the testis.
C
be found in as many as 10% of testicular sonograms (Fig. 6-14). They are most common in elderly patients and are often located near the mediastinum of the testis. Even when they are large they are usually not palpable. If they appear as simple cysts on sonography, they can be ignored. However, a cystic tumor such as a teratoma should be considered if they are multiseptated, contain intraluminal internal echogenicity, exhibit solid
components, have a thick wall, or have detectable internal vascularity. Unlike simple cysts, complex cystic tumors are usually palpable.
A variant of simple testicular cysts that are very firm and easily palpable are cysts of the tunica albuginea. Despite their firmness, if they satisfy the sonographic criteria for a simple cyst, they can also be ignored (Fig. 6-15). Typically they are solitary and very small, but
A B
Figure 6-15 Tunica albuginea cysts in different patients. A, Longitudinal view of the testis shows a typically small, peripherally located cyst (arrow). B, Oblique view shows two peripherally located cysts (arrows) that are slightly larger than typical for tunica albuginea cysts.
160 ULTRASOUND: THE REQUISITES
Box 6-2 Testicular Neoplasms
Germ cell tumors
Seminoma
Embryonal cell
Teratoma
Choriocarcinoma
Yolk sac
Mixed germ cell
Stromal tumors
Leydig cell tumor
Sertoli cell tumor
Lymphoma/leukemia
Metastases
Epidermoid cyst
they may be larger and multiple. Because they arise within the tunica albuginea, they are always located at the periphery of the testis.
Tubular ectasia of the rete testis can also produce tiny cystic-appearing changes in the mediastinum. This is usually bilateral, although it can be quite asymmetric and in a minority of cases can be unilateral. It is often
A
associated with spermatoceles and with intratesticular cysts. Like testicular cysts, it is not palpable. Sonographically it has the appearance of multiple small cystic or tubular spaces that replace and enlarge the mediastinum (Fig. 6-16). This is a very characteristic appearance and should not be mistaken for a testicular tumor and does not require any further evaluation or follow-up.
The primary reason for scanning a patient with a scrotal mass is to determine if the mass is a testicular tumor. Germ cell tumors of the testis are the most common neoplasm in young adult men. They usually present as a nontender palpable mass. Approximately 10% will present with pain, and an even smaller percentage will present with symptoms related to metastatic disease. The most common germ cell tumors are pure seminomas and mixed germ cell tumors. Seminomas typically are homogeneous and hypoechoic (Fig. 6-17) until they become large, at which point they may become heterogeneous. Calcifications and cystic changes are rare in seminomas. They are highly sensitive to irradiation and carry a good prognosis. Mixed germ cell tumors include various combinations of seminoma, teratoma, embryonal cell carcinoma, and choriocarcinoma. They are usually heterogeneous and often have calcification and cystic elements (Fig. 6-18). The
B
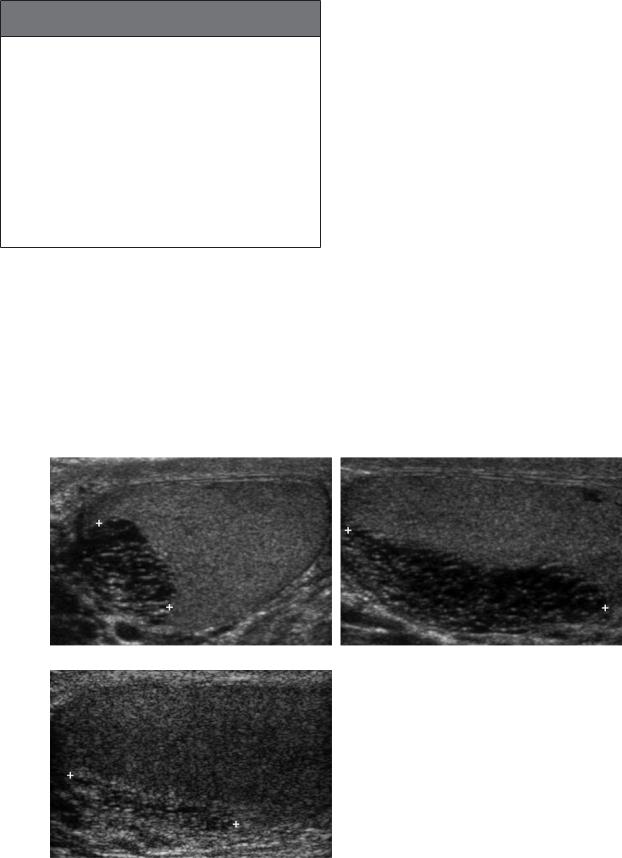
Figure 6-16 Tubular ectasia of the rete testes. Transverse (A) and longitudinal (B) views of the testis show marked enlargement and cystic replacement of the mediastinum (cursors). The elongated nature on the longitudinal view is very characteristic. C, Longitudinal view of a different patient shows less advanced tubular ectasia (cursors).
C

Lower Genitourinary |
161 |
A B
Figure 6-17 Seminoma in different patients. A, Longitudinal view of the testis shows a homogeneous hypoechoic solid mass (cursors) typical of a seminoma. B, Longitudinal view shows another typical-appearing seminoma (cursors). C, Longitudinal view shows a large lesion (cursors) almost entirely replacing the testis. Several small areas of central calcification are present. Calcification is very unusual in seminomas.
C
A B
Figure 6-18 Nonseminomatous testicular tumors in different patients. A, Longitudinal view of the testis shows two hypoechoic solid lesions. The smaller more anterior lesion is more heterogeneous. This was pathologically proven to represent a teratocarcinoma (combination of teratoma and embryonal cell carcinoma). B, Longitudinal view shows a heterogeneous but predominately hyperechoic mass with small internal cystic elements and a hypoechoic halo (cursors). Microlithiasis is also seen in the remainder of the testis. This represented a mixed germ cell tumor. C, Transverse view of the testis shows a heterogeneous isoechoic mass with a peripheral halo and multiple small internal cystic components (cursors). This was a yolk sack tumor.
C
