
2 курс / Нормальная физиология / Учебное_пособие_по_физиологии_крови_Авдеева_Е_В_,_Репалова_Н_В_
.pdf
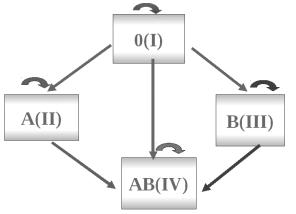
Fig. 53. Mechanism of agglutination.
5. Rhesus system.
In 1940 K. Landsteiner and I. Winner found one more antigen on the erythrocytes of macaque rhesus (fig. 54), they named it rhesus-factor.
Fig. 54. Macaque rhesus.
There are six common types of Rh antigens, each of which is called an Rh factor. These types are designated C, D, E, c, d, and e. A person who has a C antigen does not have the c antigen, but the person missing the C antigen always has the c antigen. The same is true for the D-d and E-e antigens.
There are 2 blood groups in rhesus system: Rh+ – blood has antigen D;
Rh- – blood does not have antigen D (fig. 55).
81

Fig. 55. Blood groups in rhesus system.
6. Rhesus conflict.
Rhesus conflict can occur in 2 cases.
After blood transfusion (after transfusion of Rh+ blood to Rh- recipient) (fig. 56). The first blood transfusion is not dangerous. The maximal titre of antibodies is after 2-4 months. After this period, transfused erythrocytes are derived out of bloodstream. But antirhesus-antibodies are already in the blood of the patient. And after the second transfusion of Rh+ blood agglutination occurs, haemolysis of erythrocytes, which can lead to hemolytic shock and death.
Fig. 56. Rhesus conflict after blood transfusion.
During pregnancy (if an Rh- woman is pregnant with an Rh+ fetus). As usual there are no complications during the first pregnancy. During delivery placental barrier is disturbed and erythrocytes of a fetus get into the blood of a woman. The formation of antirhesus-antibodies (IgG) starts.
During the second Rh-conflict pregnancy, antirhesus-antibodies are passing through placenta in the organism of the fetus and it will cause the destruction of erythrocytes, which will cause the death of the fetus and missbirth. If during the first pregnancy there is fetoplacental insufficiency, small amount of erythrocytes can get
82

into the woman’s organism and cause the production of immunoglobulins. As usual, titre of antibodies increases slowly during several months that is why no serious complications occur. In this case hemolytic anemia of a newborn can take place (fig. 57).
Fig. 57. Rhesus conflict during pregnancy.
Erythroblastosis fetalis (Ch. 35. Guyton, A.C. Textbook of medical physiology).
7. Other systems of blood.
In 1930 for the discovery of blood groups K. Landsteiner was granted with the Nobel Prize. During the ceremony he said that new agglutinogens would be discovered in future and the quantity of blood groups would increase until it reached the number of Earth’s population. And he was right. Even in ABO blood system several variants of every agglutinogen werefound. There are 10 variants of agglutinogen A. The difference between them is that A1 is the most active, and others have less antigenic properties. The blood group of these patients can be mistakenly defined as 1 blood group that can cause complications during transfusion.
Except ABO blood system, the most important are Rh, MNS, P, Luteran, KellChelano, Daffi, Diego, and Kid. Antigens of these blood systems are situated on erythrocytes, independently on ABO system and independently on each other. These systems are important only when there are freguent blood transfusions and during pregnancy, which is incompatible with any of these antigens.
8. Rules of blood transfusion.
1)The blood should have the same group and same rhesus.
2)Blood should be cross-matched to prevent combination of a identical agglutinins of recipient and agglutinogens of a donor (fig. 58).
83
3)According to the rule of dilution, agglutinins of a donor are disregarded in transfusion of small quantities (< 250 ml) of blood.
4)Blood should not be transfused from the same donor more than once.
People with I (O) blood group are thought to be universal donors. Their blood was used to transfuse to the recipients of other groups. Now these blood transfusions are not allowed. Why? Erythrocytes of I group do not have antigens A and B and in fact packed red cells of I group can be transfused to the recipients of other group. But plasma of I blood group includes agglutinins α and β, that’s why it can cause agglutination in blood, which includes agglutinogens A and B (blood with II, III and IV group). This plasma can be injected to the recipients in limited quantities (< 250 ml), so transfused agglutinins will be dissolved and agglutination will not occur.
Persons with group IV blood are known as universal recipients.
Fig. 58. Rule of blood transfusion.
RECOMENDED LABORATORY WORKS
1.Determination of bleeding time by Duke's method.
2.Determination of the prothrombin time according to Abramson and Vainshtein micromethod.
3.Determination of the clot retraction according to Matis method.
4.Determination of the blood groups by standard agglutinating serum.
5.Determination of the blood groups by colyclons.
SUPPLEMENT
1. Determination of bleeding time by Duke's method.
The time required for complete stopping of blood flow from the punctured blood vessels called the bleeding time.
Normally it is 1-3 minutes for a normal human's blood.
Normal clotting time and bleeding time values differ because bleeding time is the time for stopping bleeding by the formation of fibrin network on the surface of
84

punctured skin; participation of extrinsic and intrinsic mechanisms. But the clotting time is the time for clotting the whole blood, collected in the capillary tube; participation only intrinsic mechanisms. For this reason clotting time is more than the bleeding time, when determining by conventional methods.
For the work it is necessary to have: a sterilized needle, filter paper, cotton, alcohol, and a stop watch.
The succession of the work. A finger of a subject is sterilized with alcohol and pricked with a sterilized needle. Time of pricking is noted. Take the stain of the punctured point on a filter paper on 30 second and keep taking stain of blood in 20 second intervals until the bleeding stops (fig. 59). The time of no stain has come is noted properly; it is the bleeding time of the subject.
Fig. 59. Procedure (Duke's method).
Clinical significance: It plays a significant role
a)to study the haemorrhagic disorders.
b)to study the coagulation defects
c)to have an idea about the platelets count of the patient. Bleeding time is prolonged in few disorders like: vascular lesions, platelet defect, severe liver disease, uremia and anti-coagulant drug administration.
2. Determination of the prothrombin time according to Abramson and Vainshtein micromethod.
For the work it is necessary to have: a water bath, a thermometer, a watch glass, micropipettes, a glass hook, 1.11% solution of calcium chloride, 3% suspension of thromboplastm, blood for analysis, a stop watch.
The succession of the work. Place the watch glass into the water bath (t = 37°C), Place a drop of calcium chloride solution on the watch glass and a drop (without mixing) of suspension of thromboplastin. Place the blood drop on the glass, mix 3 drops, start the stop-watch. Touch the drop with a glass hook every 2 sec. Note the time when the fibrin's filaments (threads) appear.
Norm is 30-40 sec.
85

3.Determination of the clot retraction according to Matis method.
This test is the index quantity and condition of blood plates.
For the work it is necessary to have: a test-tube, a micropipette, castor oil,
blood for analysis.
The succession of the work. Fill a test-tube with castor oil. Place 20 mm3 of blood with a micropipette on the surface of the castor oil. Note the time when the serum appears.
Norm is 20-60 min (average 30 min).
The clot retraction slows down or is absent in thrombopenia, fibrmo-genopenia.
4.Determination of the blood groups by standard agglutinating serum.
For the work it is necessary to have: standard agglutinating serum 1.2 and 3 groups, glasses, smooth white surface (a plate), blood for analysis.
Serum of the
1st I (O ) group contains agglutinins α and β;
2nd II (A) group – agglutimn β;
3rd III (B)group – agglutinin α;
4th IV (AB) group is not used because it is agglutinin-free.
The succession of the work. The glass is placed on white paper. Drop (not mixing) 4 (3) drops of standard serums on the glass. Carry blood drops to the drops of serums by the comers of the other glass (fig. 60).
Reaction of agglutination begins in 1-5 min. Drop becomes transparent, erythrocytes stick together in the presence of agglutination.
Fig. 60. Procedure of blood determination.
A blood group is determined according to reaction of agglutination (fig. 61).
86

blood group
Fig. 61. Determination of blood groups by standard agglutinating serum.
5. Determination of the blood groups by colyclons.
For the work it is necessary to have: colyclons, glasses, smooth white surface (a plate), blood for analysis.
Colyclons are
anty A – contains agglutinins α;
anty B – agglutimn β;
anty D – agglutinin to Rh.
The succession of the work. The glass is placed on white paper. Drop (not mixing) 4 (3) drops of colyclons on the glass. Carry blood drops to the drops of serums by the comers of the other glass. Reaction of agglutination begins in 1-5 min. Blood group is determined according to reaction of agglutination (fig. 62).
Fig. 62. Determination of blood groups by colyclons.
87
QUESTIONS FOR SELF-CONTROL
1.Explain and enumerate hemostasis and its stages.
2.Enumerate the characteristics of platelets.
3.Characterize all the stages of vascular platelet hemostasis.
4.Elucidate the scheme and explain the processes involved in the extrinsic mechanism of prothrombin activator formation.
5.Intrinsic mechanism of prothrombin activator formation.
6.Characterize the conversion of prothrombin into thrombin.
7.Characterize the conversion of fibrinogen into fibrin.
8.Explain the term: retraction. What is the duration of this process?
9.Explain the term: fibrinolysis.
10.Enumerate the activators of fibrinolysis.
11.Characterize the phases of fibrinolysis.
12.Enumerate anticoagulation mechanisms.
12.What anticoagulants are called primary anticoagulants?
13.What anticoagulants are called secondary anticoagulants?
14.What are the characteristic of antithrombin III, heparin, 2-macroglobulin?
15.Enumerate the anticoagulants for clinical use.
16.What do hypercoagulaemia and hypocoagulaemia mean?
17.Why does hypercoagulation develop upon activation of the sympathetic part of ANS?
18.Why is hypocoagulation always secondary and develops after primary hypercoagulation?
19.Describe how bleeding time is determined.
20.Describe how clotting time is determined.
21.Describe how prothrombin time is determined.
22.What are the main blood group systems? Why?
23.What types of agglutinogens and agglutinins are present in the A-O-B system?
24.What is the origin of agglutinins?
25.What is Rh factor? Who are «Rh-positive» and «Rh-negative» people?
26.Explain the Rh immune response and erythroblastosis fetalis.
27.Enumerate the main principles of blood transfusion.
28.What do direct and reverse agglutination mean?
29.Describe the methods of determining blood groups.
88
|
TESTS FOR SELF-CONTROL |
1. |
WRITE THE MISSING WORD! |
DECOMPOSITION OF FIBRIN CLOT IS CALLED [___].
2. FIND SEVERAL CORRECT ANSWERS!
FACTORS PREVENTING CLOTTING IN THE NORMAL VASCULAR SYSTEM ARE:
1.glycocalix
2.protrombin
3.heparin
4.the smoothness of endothelium
5.thrombomodulin
3. FIND SEVERAL CORRECT ANSWERS!
THE SYSTEM OF BLOOD COAGULATION CONSISTS OF:
1.blood
2.lymph
3.tissues which produce the substances necessary for the hemocoagulation
4.neurohumoral apparatus
5.muscle
4. INDICATE THE CORRESPODENCE!
THE NUMBER OF |
THE NAME OF |
PLASMA FACTOR |
PLASMA FACTOR |
1. factor I |
a. ions of Ca2+ |
2. factor IX |
b. fibrinogen |
3. factor XII |
c. prothrombin |
4. factor IV |
d. Hageman factor |
5. factor VII |
e. proconvertin |
6. factor II |
f. Christmas factor |
5. FIND THE CORRECT ANSWER!
WHAT GROUP OF BLOOD (SYSTEM ABO) WAS PUT IN TO THE STANDARD SERUMS IF AGGLUTINATION TOOK PLACE IN SERUM OF FIRST AND THE SECOND GROUPS?
1.first blood group
2.such combination can not take place (mistake of determination)
3.fourth blood group
4.second blood group
5.third blood group
89

6. WRITE THE MISSING WORD!
[___] OF BLOOD-THE PROCESS OF FORMATION OF FIBRIN CLOT.
7. |
INDICATE THE CORRESPODENCE! |
|
||
|
|
|
|
|
|
|
1 |
|
2 |
|
|
|
|
|
|
|
|
|
|
a.extrinsic pathway
b.intrinsic pathway c. direct pathway
d. indirect pathway
c.primary pathway
8. INDICATE THE CORRESPONDENCE!
GROUP OF ANTICOAGULANTS: |
ANTICOAGULANTS: |
1. primary |
a. factor XI |
2. secondary |
b. factor V |
|
c. heparin |
|
d. alpha2-macroglobulin |
|
e. antithrombin III |
9. FIND THE CORRECT ANSWERS!
PRINSIPLES OF BLOOD TRANSFUSION:
1.blood should be cross-matched
2.rule of dilution (agglutinins of donor is disregarded in transfusion of small quantities of blood)
3.Egorov's rule
4.blood should be incross-matched
5.Zweig rule
90
