
нормальная рентгенанатомия легких
.pdf
C H A P T E R 1 ● Normal Chest Radiograph |
23 |
|
|
|
|
|
|
|
A
B
■ FIGURE 1-30 Azygoesophageal recess. A, Detail view from a frontal chest radiograph showing the azygoesophageal recess as a smooth continuous arc (arrowheads) as it extends from the diaphragm to the level of the azygos arch. B, Contrast medium–enhanced CT scan showing the azygos vein and the esophagus forming the medial border of the azygoesophageal (AE) recess.
esophageal tumor or duplication cyst, azygos vein dilation, or subcarinal lymph node enlargement.
The left lateral wall of the trachea is rarely visible on a posteroanterior chest radiograph because of contiguity of the left subclavian artery and mediastinal fat. On a frontal chest radiograph the mediastinal shadow to the left of the trachea above the level of the aortic arch is typically a low-density arcuate opacity (concave laterally) extending from the aortic arch to a point at or just above the medial end of the clavicle (Fig. 1-31). The lateral margin of this density corresponds to the course of the left subclavian artery and may be formed by the artery or, more com-
■ FIGURE 1-31 Normal left mediastinal shadow. A detail view from a frontal chest radiograph shows the outer margin of the left mediastinum above the aortic arch (AA) as an arcuate opacity concave laterally (arrowheads) and extending from the aortic arch to a point just above the medial end of the clavicle. The lateral margin of this opacity corresponds to the course of the left subclavian artery and may be formed by the artery or, more commonly, by adjacent fat. The first convexity of the left aspect of the mediastinum is formed by the posterior portion of the aortic arch. Extending from the aortic arch, the left border of the descending aorta (arrows) can be seen coursing medially down to the level of the diaphragm.
monly, by adjacent fat. The left subclavian artery arises from the aorta behind the left common carotid artery and passes upward lateral to the trachea in contact with the left mediastinal pleura.
The first convexity of the left aspect of the mediastinum is formed by the posterior portion of the aortic arch (Fig. 1-31). Extending from the aortic arch, the left border of the descending aorta can usually be seen coursing medially down to the level of the diaphragm. Contact of the lateral aspect of the descending aorta and the left lung results in the left para-aortic interface. This interface is normally slightly concave laterally or straight. A lateral convexity of the left para-aortic interface may result from tortuosity of the aorta (normally seen in the elderly), an aortic aneurysm, a para-aortic mediastinal mass, or enlarged lymph nodes.
A small triangular or round opacity is seen immediately lateral to the aortic arch on approximately 1% of chest radiographs.38 This opacity, known as the “aortic nipple,” is caused by the left superior intercostal vein as it courses cephalad and forward to enter the left brachiocephalic

24 P A R T O N E ● Normal Chest
A B
■ FIGURE 1-32 Normal and enlarged aortic nipple. A, Detail view from a frontal radiograph showing a small triangular opacity (arrow) immediately lateral to the aortic arch. This opacity, known as the aortic nipple, is caused by the left superior intercostal vein as it courses cephalad and forward to enter the left brachiocephalic vein. B, View from a chest radiograph in a patient with obstruction of the superior vena cava showing marked enlargement of the aortic nipple (arrow) as a result of increased size of the left superior intercostal vein caused by the collateral venous drainage.
vein (Fig. 1-32). In erect normal subjects the aortic nipple may range in size from a small protuberance up to 4.5 mm in diameter. As might be expected, the vein dilates and becomes more prominent when an individual assumes the supine position or performs a Müller maneuver. Dilation also occurs in a variety of disease states that result in increased flow or pressure (or both), particularly obstruction of the left brachiocephalic vein or SVC (Fig. 1-32).
The opacity seen immediately below the level of the aortic arch and above the left main bronchus is the main pulmonary artery. At this level the main pulmonary artery appears as an oval or elliptical opacity medial to the left pulmonary artery. From the level of the aortic arch to the level of the left pulmonary artery the lateral border of the mediastinum is normally concave laterally or straight. The space between the arch of the aorta and the left pulmonary artery is known as the aortopulmonary window (Fig. 1-33). It is occupied largely by mediastinal fat; its medial boundary is the ductus ligament, and its lateral boundary is the mediastinal and visceral pleura over the left lung, which creates the aortopulmonary window interface (Fig. 1-34). Convexity of the aortopulmonary window interface may result from lymph node enlargement, a mediastinal tumor, or an aortic aneurysm. Because the left recurrent laryngeal nerve courses in the aortopulmonary window, pathologic processes in this region may be associated with left vocal cord palsy and hoarseness.
The outer contour of the mediastinum below the level of the left main bronchus is caused by the heart. The upper aspect, corresponding to the region of the left
atrium and left atrial appendage, is normally straight or concave, and the lower aspect, corresponding to the left ventricle, is normally convex (see Fig. 1-33).
The anterior mediastinum has its narrowest point below the level of the great vessels and aortic arch, and the posterior mediastinum has its narrowest point above the level of the aortic arch. The lungs at these levels may occasionally appear to abut each other on a frontal radiograph and result in linear shadows known as the anterior and posterior junction line, respectively.
The anterior junction line is formed by contact of the right and left lungs with the adjacent anterior mediastinum in the retrosternal space. It consists of four layers of pleura (two layers of visceral pleura covering the lungs and two layers of mediastinal pleura) and a variable quantity of intervening mediastinal fat. On a posteroanterior chest radiograph this line is typically oriented obliquely from upper right to lower left behind the sternum (Fig. 1-35). The anterior junction line is seen in approximately 20% of cases. It may be displaced ipsilaterally in patients with atelectasis.
The right and left upper lobes contact the mediastinum behind the esophagus anterior to the third through fifth vertebral bodies, where they form a pleural apposition that along with any intervening mediastinal tissue creates the posterior junction line (Fig. 1-35). On a posteroanterior radiograph, the posterior junction line usually projects through the air column of the trachea; it may be straight or slightly convex to the left. When intervening mediastinal tissue is abundant or a narrowed retroesopha-
C H A P T E R 1 ● Normal Chest Radiograph |
25 |
|
|
|
|
|
|
|
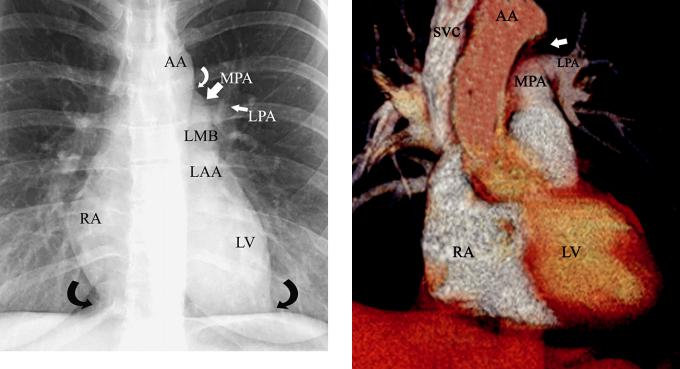
■ FIGURE 1-33 Normal mediastinum and heart. A detail view from a frontal radiograph shows the aortic arch (AA). The opacity seen immediately below the level of the aortic arch and above the left main bronchus is the main pulmonary artery (MPA). At this level the main pulmonary artery appears as an oval or elliptical opacity medial to the
left pulmonary artery (LPA). From the level of the aortic arch to the level of the pulmonary artery, the lateral border of the mediastinum is normally concave laterally or straight (white curved arrow). The space between the arch of the aorta and the pulmonary artery is known as
the aortopulmonary window. The main and left pulmonary arteries are located immediately above the level of the left main (LMB) and left upper lobe bronchi. The lateral border immediately below the left main bronchus is formed by the left atrial appendage (LAA) and is usually slightly concave or straight. The remaining left border of the heart is formed by the left ventricle (LV). The right border of the heart is formed by the right atrium (RA). The cardiophrenic angles or sulci (black curved arrows) are located at the junction of the cardiopericardial silhouette and the diaphragm. Variable amounts of fat (pericardial fat) are normally present in this region.
geal space precludes lung apposition, the posterior junction line can appear as a distinct stripe.
Lateral Chest Radiograph
The trachea can be readily seen on a lateral radiograph as it descends in a straight course obliquely caudally and posteriorly (Fig. 1-36). Forward bowing may occur as a result of aortic unfolding or posterior indentation by an enlarged esophagus, an abnormal vessel, or a mediastinal mass. The anterior wall of the trachea is seldom visible because it is obscured by the mediastinum, but the posterior wall can usually be seen because it abuts the lung.
The posterior wall together with adjacent fat forms the posterior tracheal stripe or band. This stripe generally measures less than 4 mm in diameter. Measurement of this stripe, however, is seldom helpful because the esophagus may be interposed between the posterior trachea and lung and result in a stripe thickness of 1 cm or greater. A focal opacity in the region of the posterior tracheal stripe or an
■ FIGURE 1-34 Normal mediastinum and heart. A volume-rendering image from a CT scan shows the superior vena cava (SVC) and right atrium (RA) forming the right lateral margin of the mediastinum, left ventricle (LV), ascending aorta and aortic arch (AA), and main (MPA) and left (LPA) pulmonary arteries. The aortopulmonary window (arrow) is situated between the aortic arch and the proximal left pulmonary artery.
increase in thickness on serial radiographs should raise the possibility of esophageal carcinoma.
The region posterior to the tracheal stripe and anterior to the spine above the level of the aortic arch is known as the retrotracheal triangle (Fig. 1-36). This triangle is relatively lucent and contains the esophagus, lymph nodes, and posterior segments of the upper lobes. Increased opacity in the retrotracheal triangle may be due to an esophageal tumor, a thyroid mass, lymph node enlargement, an aberrant subclavian artery, an aneurysm, or a foregut duplication cyst.
The shadow anterior to the trachea above the level of the aortic arch includes the head and neck vessels. The brachiocephalic artery may be recognized as it arises anterior to the tracheal air column. The aortic arch and descending aorta can usually be seen on a lateral radiograph, but the ascending aorta is difficult to identify unless it is unfolded, enlarged, or calcified.
The left pulmonary artery is seen in virtually all cases as it courses over the left main and upper lobe bronchi and descends behind the bronchi to form an arch roughly parallel to the aortic arch. The proximity of the descending left pulmonary artery to the anterolateral aspect of the descending aorta may result in focal obscuration of the margins of these vessels. Obscuration of the left pulmonary artery at any other level should raise the possibility of an adjacent abnormality in the aortopulmonary window, left hilum, or left lung.

26 P A R T O N E ● Normal Chest
B
A C
■ FIGURE 1-35 Anterior and posterior junction lines. A, Detail view of a chest radiograph showing the anterior junction line (arrowheads) extending from the level of the aortic arch inferiorly and obliquely to the left and posterior junction line (arrows) above the level of the aortic arch. B, CT scan at the level of the bronchus intermedius showing contact of the right and left lungs (arrows) in the retrosternal space. This contact results in the anterior junction line seen on the radiograph. C, CT scan in the region of the thoracic inlet showing contact of the right and left lungs (arrows) posterior to the esophagus, which results in the posterior junction line.
KEY POINTS: HILA AND
MEDIASTINUM
■Left hilum normally 1 to 2 cm higher than the right
■Normal diameter of the vascular pedicle: <7 cm
■Normal right paratracheal stripe: 1 to 4 mm
■Normal diameter of the azygos vein in the upright position: <10 mm
■Normal diameter of the azygos vein in the supine position: <15 mm
Heart
On a frontal radiograph of a normal chest, the position of the heart in relation to the midline of the thorax depends largely on the patient’s build (see Fig. 1-33). Assuming radiographic exposure with the lungs fully inflated, the heart shadow is almost exactly midline in position in asthenic individuals, only projecting slightly more to the left; in individuals of stockier build, it lies a little more to the left of midline.
In normal individuals, the transverse diameter of the heart measured on standard posteroanterior radiographs is generally in the range of 11.5 to 15.5 cm; it is less than 11.5 cm in approximately 5% and only rarely exceeds 15.5 cm (in heavy subjects of stocky build).22 A commonly used measurement to assess overall heart size is the ratio of the widest cardiac diameter to the widest inside thoracic diameter, known as the cardiothoracic ratio. A cardiothoracic ratio greater than 50% on a posteroanterior radiograph with the patient upright has a specificity of approximately 80% for the detection of left ventricular dilation but a sensitivity of only 50%.22 The cardiothoracic ratio is not helpful in detecting left atrial or right ventricular enlargement because neither of these chambers is reflected in the transverse dimension.
Cardiac size and contour of the heart are influenced by five main factors:
1.Cardiac cycle: the diameter is largest at end diastole and smallest at peak systole. The change in heart width between systole and diastole is usually less than 1 cm.
2.Height of the diaphragm, which in turn is influenced by the degree of pulmonary inflation. The lower the position of the diaphragm, the longer and narrower the cardiovascular silhouette.

■ FIGURE 1-36 Trachea and retrotracheal triangle. A lateral radiograph shows the trachea as it descends in a straight course obliquely caudally and slightly posteriorly. The posterior wall together with adjacent fat forms the posterior tracheal stripe (arrow). The region posterior to the tracheal stripe and anterior to the spine above the level of the aortic arch is known as the retrotracheal triangle (arrowheads).
3.Intrathoracic pressure, which influences not only cardiac size but also the appearance of the pulmonary vascular pattern.
4.Body position: assuming equality of all other factors, the heart is broader when a subject is recumbent than when erect.
5.Posteroanterior versus anteroposterior radiograph: the heart is magnified more and appears larger on radiographs performed with anteroposterior projection of the x-ray beam.
The right border of the heart on a frontal radiograph is formed by the right atrium as it abuts the right middle lobe (see Fig. 1-34). Adjacent to the diaphragm, the inferior vena cava may be seen as it enters the right atrium.
The right ventricle is not visible on a frontal radiograph. The left heart border immediately below the level of the left bronchus is formed by the left atrial appendage and adjacent epicardial fat. The remainder of the left heart border is formed by the left ventricle.
The heart border immediately below the level of the left bronchus is typically concave or straight (see Fig.
C H A P T E R 1 ● Normal Chest Radiograph |
27 |
1-33). A focal convexity at this level is most suggestive of enlargement of the left atrial appendage, a finding seen most commonly in mitral heart disease. Enlargement of the left atrium may elevate the left main bronchus and cause splaying of the tracheal carina. Enlargement of the left ventricle results in an increased cardiothoracic ratio and elongation of the long axis of the left ventricle.
The junction of the right and left heart borders with the anterior hemidiaphragms results in the right and left cardiophrenic angles or recesses (Fig. 1-33). These recesses contain fat (pericardial fat pad) and lymph nodes and are usually concave laterally. Their density is slightly less than that of the heart, thus allowing identification through them of the approximate position of the cardiac borders (Fig. 1-37). These pleuropericardial fat shadows should not be misinterpreted as cardiac enlargement or as mediastinal or diaphragmatic masses. A focal convexity of the cardiophrenic angle may result from the accumulation of fat (prominent pericardial fat pad), a pericardial cyst, enlarged pericardiophrenic lymph nodes, or a Morgagni hernia (Fig. 1-37).
On a lateral view the anterior border of the heart is formed by the right ventricle. Normally, the right ventricle contacts only the lower half of the sternum (Figs. 1-38 and 1-39). The earliest sign of right ventricular enlargement on the radiograph is an increased area of contact between the heart and the sternum. The posterior heart border is formed in its upper third by the left atrium and in its lower two thirds by the left ventricle. In some patients the inferior vena cava may be seen entering the posterior border of the right atrium (Fig. 1-38). Left atrial enlargement results in posterior bulging of the upper heart shadow, whereas left ventricular enlargement results in posterior bulging of the lower two thirds of the heart shadow.
Diaphragm
The diaphragm is a musculotendinous structure that separates the thoracic and abdominal cavities. Its costal muscle fibers arise anteriorly from the xiphoid process and around the convexity of the thorax from ribs 7 to 12; posteriorly, the crural fibers arise from the lateral margins of the first, second, and third lumbar vertebrae on the right side and from the first and second lumbar vertebrae on the left. These fibers converge toward the central tendon and are inserted into it nearly perpendicular to its margin.
On a chest radiograph the upper surface of the domeshaped diaphragm is normally visualized as it forms an interface with the lung; the soft tissues of the abdomen obscure its inferior surface. In approximately 95% of normal adults, the level of the cupola of the right hemidiaphragm is projected in a plane ranging from the anterior end of the fifth rib to the sixth anterior interspace; in about 5%, it is projected at or below the level of the seventh rib.54 In approximately 90% of adults, the plane of the right diaphragmatic dome is about half an interspace higher than the left; both are at the same height, or the left is higher than the right in approximately 10% of normal subjects (Fig. 1-40).48 On a left lateral view of the chest the right hemidiaphragm is seen along its entire length, whereas the anterior portion of the left hemidiaphragm is obscured by the heart (Fig. 1-40).

A B
D
C
F
E
■ FIGURE 1-37 Pericardial fat pads and mediastinal lipomatosis. A, Posteroanterior chest radiograph showing the left pericardial fat pad (arrows). B, A CT image in the same patient as in A demonstrates the left and right pericardial fat pads. C, A posteroanterior chest radiograph in another patient shows the right pericardial fat pad (arrow). D, A CT image in the same patient as in C demonstrates the right pericardial fat pad (arrow).
E, An anteroposterior chest radiograph in a patient undergoing long-term corticosteroid therapy shows widening of the mediastinum and apparent enlargement of the cardiopericardial silhouette. F, A coronal reformatted image from a multidetector CT scan in the same patient as in
E demonstrates extensive mediastinal lipomatosis and increased size of the cardiophrenic fat pads. The heart size is within normal limits.

C H A P T E R 1 ● Normal Chest Radiograph |
29 |
|
|
|
|
|
|
|
■ FIGURE 1-38 Normal cardiac anatomy on a lateral radiograph. A lateral radiograph shows the anterior border of the heart formed by the right ventricle (RV), which contacts less than the lower half of the
sternum. The lower two thirds of the posterior heart border are formed by the left ventricle (LV) and the upper third by the left atrium. The faint opacity (arrow) seen in the posterior cardiophrenic angle represents the inferior vena cava (IVC) as it drains into the right atrium. The ascending aorta, aortic arch, and proximal descending aorta are well seen in this elderly patient. The aorta is not as well seen in normal young adults.
■ FIGURE 1-39 Lateral view of the right ventricle (RV) and main pulmonary artery (MPA). A sagittal reformatted image from a CT scan shows the right ventricle, pulmonary outflow tract, and main pulmonary artery forming the anterior contour of the heart. AA, aortic arch; LPA, left pulmonary artery.
Chest Wall
On a frontal radiograph of the thorax, the soft tissues, including the skin, subcutaneous fat, and muscles, are usually distinguishable over the shoulders and along the thoracic wall. In the absence of pulmonary or pleural disease, deformity of the spine, or congenital anomalies of the ribs themselves, the rib cage should be symmetric.
The ribs are oriented obliquely; their anterior portions are slanted downward and their posterior portions are slanted upward (Fig. 1-41). The intercostal arteries, veins, and nerves are situated in the inferior inner surface of the ribs. The upper and lower borders of the ribs are normally sharply defined, except in the middle and lower thoracic regions; here, the thin flanges created by the vascular sulci on the inferior aspects of the ribs posteriorly are viewed en face, thereby resulting in a less distinct inferior margin. On a lateral view, the ribs farther from the radiographic cassette are magnified more than those adjacent to the film (the big rib sign); on a left lateral radiograph, the right ribs appear bigger than the left ribs. By convention, a lateral chest radiograph is taken with the left side against the radiographic cassette. Therefore, the right ribs, being
A
B
■ FIGURE 1-40 Normal diaphragm. A, Detail view from a frontal radiograph showing the upper surface of the dome-shaped right and left hemidiaphragms. The right hemidiaphragm is normally 1 to 3 cm above the level of the left hemidiaphragm. B, Detail view from a lateral radiograph showing the entire length of the right hemidiaphragm (straight arrows). The anterior portion of the left hemidiaphragm (curved arrows) is obscured by the heart.

30 P A R T O N E ● Normal Chest
A
■ FIGURE 1-41 Chest wall. A, Frontal view showing the oblique orientation of the ribs. The anterior portions are slanted downward and the posterior portions are slanted upward. The costal cartilages (not shown) connect the anterior ribs to the sternum. The sternum has three components: manubrium (M), body (B), and xiphoid process (X). C, clavicle. B, Lateral view demonstrating the orientation of the ribs and the position of the manubrium (M) and body (B) of the sternum and the inferior aspect of the clavicles (C) at the level of the sternoclavicular joints.
further away, are magnified and appear bigger than the left ribs.
Calcification of the rib cartilage is common and probably never of pathologic significance. The first rib cartilage is usually the first to calcify, often shortly after the age of
20. Fairly consistent differences in the pattern of costal calcification are observed in the two sexes, particularly in older individuals.55 In men, the upper and lower borders of cartilage calcify first, with calcification extending in continuity with the end of the rib; calcification of the central area follows. By contrast, calcification in women tends to occur first in a central location, in the form of a solid tongue or as two parallel lines extending into the cartilage from the end of the rib.55
In approximately 0.5% of the population, unilateral or bilateral cervical ribs can be seen arising from the seventh cervical vertebra (Fig. 1-42).56 Such ribs occur more commonly in females than in males and are generally asymptomatic incidental findings. Occasionally, they may result in thoracic outlet syndrome (pain and weakness in the C8 nerve root distribution, variation in pulse intensity in the two arms when the affected extremity is in certain positions). Other supernumerary ribs are rare.
Sometimes the inferior aspect of the clavicle has an irregular notch or indentation 2 to 3 cm from the sternal
B
articulation; its size and shape vary from a superficial saucer-shaped defect to a deep notch 2 cm wide by 1.0 to 1.5 cm deep.57 These rhomboid fossae give rise to the costoclavicular or rhomboid ligaments, which radiate downward to bind the clavicles to the first rib. The fossae are seen in about 10% of clavicles studied anatomically but are rarely detected radiologically.57
The sternum forms the anterior midline portion of the thoracic cage (see Fig. 1-41). It is made up of the manubrium, which articulates with the clavicles; the body; and the xiphoid process. The most common congenital abnormality of the sternum is a depression of the sternum known as pectus excavatum, or “funnel chest” (Fig. 1-43). When marked, pectus excavatum results in a reduction in the prevertebral space, thereby causing leftward displacement and axial rotation of the heart, and a reduction in the space occupied by the left lung.58 Posteroanterior radiographs depict the parasternal soft tissues of the anterior chest wall as an area of increased density in the inferomedial portion of the right hemithorax, displacement of the heart to the left, and obscuration of the right heart border on frontal radiographs (the latter mimics right middle lobe disease) (Fig. 1-43). Another finding is exaggerated inferior angulation of the anterior ribs. The degree of sternal depression is easily appreciated on a

C H A P T E R 1 ● Normal Chest Radiograph |
31 |
■ FIGURE 1-42 Bilateral cervical ribs. A detail view from a frontal chest radiograph shows bilateral cervical ribs arising from the seventh cervical vertebra (arrows). The patient was a 21-year-old woman with thoracic outlet syndrome.
A
■ FIGURE 1-43 Pectus excavatum. A, Posteroanterior chest radiograph demonstrating displacement of the heart to the left and obscuration of the right heart border. B, Lateral chest radiograph showing abnormal
depression of the sternum (arrows), known as pectus excavatum, or B “funnel chest.”

32 P A R T O N E ● Normal Chest
lateral radiograph. Pectus excavatum seldom leads to symptoms but is associated with a greater prevalence of congenital heart disease.
A less common congenital abnormality is abnormal protrusion of the sternum, known as pectus carinatum, or “pigeon breast” (Fig. 1-44). Although it can occur in isolation, pigeon breast is seen with increased frequency in patients with cyanotic congenital heart disease.58
The sternum is difficult to assess on a frontal view and best seen on lateral or oblique views. Retrosternal lung allows identification of a stripe between the posterior cortex of the sternal body and the lung. This retrosternal stripe is composed primarily of fat and ranges from 1 to 3 mm in thickness. Indentation of the lung by parasternal structures, particularly costal cartilage, may result in a lobulated contour posterior to the parasternal stripe. A focal convexity or lobulation that is not at the level of a costal cartilage is suggestive of an abnormality, most commonly enlarged internal mammary lymph nodes.
On an optimal chest radiograph, exposure factors should be such that the thoracic spine and intervertebral discs are faintly visible, with the spinous processes being in the midline. The thoracic spine is normally straight on a frontal radiograph and slightly concave anteriorly (dorsal kyphosis) on a lateral radiograph. Contact between the lower lobes and the paravertebral soft tissues results in paravertebral interfaces or stripes that are commonly visible on a frontal radiograph, particularly in the lower part of the chest. A left paravertebral stripe is generally longer and better seen than a right paravertebral stripe. Paravertebral stripes are usually thin and parallel to the spine. The left stripe is typically seen halfway between the lateral margin of the descending aorta and the spine. Displacement of the paravertebral stripe may occur with a vertebral abnormality (osteophyte, fracture, infection, neoplasm), paravertebral masses (hematoma, neurogenic tumor, paravertebral abscess), or lymph node enlargement.
■ FIGURE 1-44 Pectus carinatum. A lateral chest radiograph shows abnormal protrusion of the sternum (arrows), known as pectus carinatum, or “pigeon breast.”
S U G G E S T E D R E A D I N G S
Cole TJ, Henry DA, Jolles H, Proto AV. Normal and abnormal vascular structures that simulate neoplasms on chest radiographs: clues to the diagnosis. RadioGraphics 1995; 15:867-891.
Hayashi K, Aziz A, Ashizawa K, et al. Radiographic and CT appearances of the major fissures. RadioGraphics 2001; 21:861-874.
Jeung MY, Gangi A, Gasser B, et al. Imaging of chest wall disorders. RadioGraphics 1999; 19:617-637.
MacMahon H. Digital chest radiography: practical issues. J Thorac Imaging 2003; 18:138-147.
Müller NL, Webb WR. Radiographic imaging of the pulmonary hila. Invest Radiol 1985; 20:661-671.
Proto AV. Mediastinal anatomy: emphasis on conventional images with anatomic and computed tomographic correlations. J Thorac Imaging 1987; 2:1-48.
Proto AV, Speckman JM. The left lateral radiograph of the chest. Part 1. Med Radiogr Photogr 1979; 55:29-74.
Proto AV, Speckman JM. The left lateral radiograph of the chest. Med Radiogr Photogr 1980; 56:38-64.
Schaefer-Prokop C, Uffmann M, Eisenhuber E, Prokop M. Digital radiography of the chest: detector techniques and performance parameters. J Thorac Imaging 2003; 18:124-137.
Verschakelen J, Bellon E, Deprez T. Digital chest radiography: quality assurance. J Thorac Imaging 2003; 18:169-177.
R E F E R E N C E S
1.American College of Radiology. Practice guidelines for the performance of adult and pediatric chest radiography. 2001.
2.Hasegawa BH, Naimuddin S, Dobbins JT 3rd, et al. Digital beam attenuator technique for compensated chest radiography. Radiology 1986; 159:537-543.
3.Plewes DB, Vogelstein E. A scanning system for chest radiography with regional exposure control: practical implementation. Med Phys 1983; 10:655-663.
4.MacMahon H, Vyborny C. Technical advances in chest radiography. AJR Am J Roentgenol 1994; 163:1049-1059.
