Cardiac Glycosides & Congestive Heart Failure
OBJECTIVES
You should be able to:
• Describe the strategies and list the major drug groups used in the treatment of congestive heart failure.
• Describe the probable mechanism of action of digitalis.
• Describe the nature and mechanism of the toxic effects of digitalis on the heart.
• List some positive inotropic drugs that have been investigated as digitalis substitutes.
• Explain the beneficial effects of vasodilators and ACE inhibitors in congestive heart failure.
Learn the definitions that follow
Term |
Definition |
Bigeminy |
An arrhythmia consisting of normal sinus beats coupled with ventricular extrasystoles, ie, "twinned beats" |
Cardenolide |
The basic chemical structure required for cardiac glycoside action, consisting of a steroid nucleus and a lactone ring at the 17 position |
Congestive heart failure |
A condition in which cardiac output is insufficient for the needs of the body. Low-output failure is the more common form and is more responsive to positive inotropic drugs than high-output failure |
End-diastolic fiber length |
The length of the ventricular fibers at the end of diastole; a determinant of the force of the following contraction |
PDE inhibitor |
Phosphodiesterase inhibitor; a drug that inhibits one or more enzymes that degrade cAMP (and other cyclic nucleotides). Example: high concentrations of theophylline |
Premature ventricular beats |
Abnormal beats arising from a cell below the AV node; often from a Purkinje fiber, sometimes from a ventricular fiber |
Sodium pump (Na+/K+ ATPase) |
A transport molecule in the membranes of all vertebrate cells; responsible for the maintenance of normal low intracellular sodium and high intracellular potassium concentrations |
Sodium-calcium exchanger |
A transport molecule in the membrane of many cells (eg, cardiac cells) that pumps one calcium atom against its concentration gradient (outward) in exchange for three sodium ions (moving down their concentration gradient) |
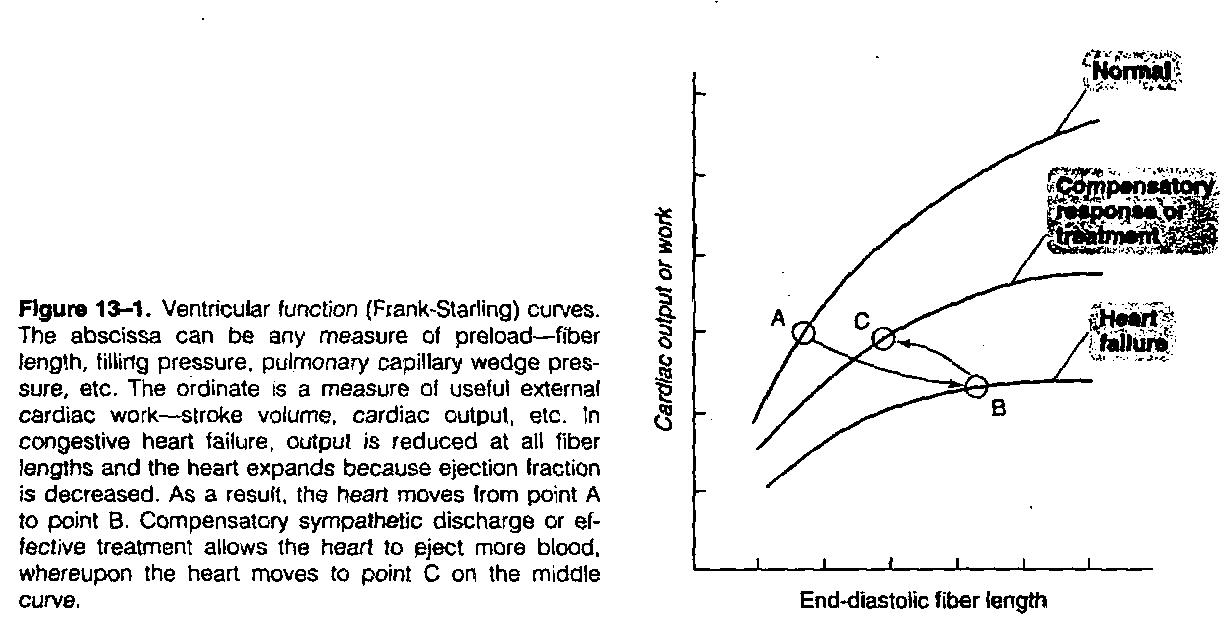
Ventricular function curve |
The curve that relates cardiac output, stroke volume, etc, to filling pressure or end-diastolic fiber length; also known as the Frank-Starting curve |
Ventricular tachycardia |
An arrhythmia consisting entirely or largely of beats originating below the A V node |
Concepts pathophysiology of congestive heart failure & treatment strategies
A. Pathophysiology: The fundamental physiologic defect in congestive heart failure is a decrease in cardiac contractility. The result of the defect is that cardiac output is inadequate for the needs of the body. This is best shown by the ventricular function curve (Frank-Starling curve; Figure 13-1). The homeostatic responses of the body to depressed cardiac output are mediated mainly by the sympathetic nervous system and the renin-angiotensin-aldosterone system. While these compensatory responses may temporarily improve cardiac output, they also increase the load on the heart; the increased load contributes to a further decline in cardiac function. The ventricular function curve reflects some of these deleterious compensatory responses and may also be used to demonstrate the response to drugs. As ventricular ejection decreases, the end-diastolic fiber length increases as shown by the shift from point A to point B in Figure 13-1. Operation at point B is intrinsically less efficient than operation at shorter fiber lengths because of the increase in myocardial oxygen requirement associated with increased fiber stretch (Figure 12-2).
Other compensatory responses include the following: (1) Tachycardia: an early manifestation of increased sympathetic tone. (2) Increased peripheral vascular resistance: another early response, also mediated by increased sympathetic tone. (3) Retention of salt and water by the kidney: an early compensatory response, mediated by the renin-angiotensin-aldosterone system and by increased sympathetic outflow. Increased blood volume results in edema and pulmonary congestion and contributes to the increased end-diastolic fiber length. (4) Cardiomegaly: enlargement of the heart is a slower compensatory response, mediated at least in part by sympathetic discharge. Angiotensin II also plays an important role.
B. Therapeutic Strategies in Congestive Heart Failure: Pharmacologic therapies for congestive heart failure include the removal of retained salt and water with diuretics; direct treatment of the depressed heart with positive inotropic drugs such as digitalis glycosides; reduction of preload or afterload with vasodilators; and reduction of afterload and retained salt and water by angiotensin-converting enzyme inhibitors, In addition, recent evidence suggests that ACE inhibitors also alter the structural changes (remodeling) that often follow myocardial infarction and lead to congestive failure. The use of diuretics is discussed in Chapter 15.