
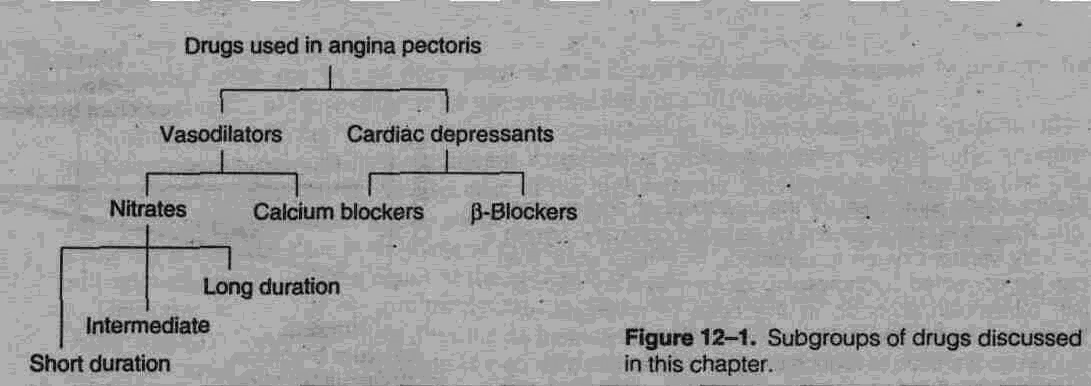
Vasodilators & the Treatment of Angina objectives
You should be able to:
• List the major determinants of cardiac oxygen consumption.
• List the strategies for relief of anginal pain.
• Contrast the therapeutic and adverse effects of nitrates, beta-blockers, and calcium channel blockers when used for angina.
• Explain why a combination of a nitrate with a beta-blocker or a calcium channel blocker may be extremely effective.
• Contrast the effects of medical therapy and surgical therapy of angina.
Learn the definitions that follow.
Table 12-1. Definitions.
|
|
Term
|
Definition
|
Angina of effort, classic angina, atherosclerotic angina |
Angina (crushing, strangling, chest pain) that is precipitated by exertion, ie, increased 02 demand that cannot be met because of irreversible atherosclerotic obstruction of coronary arteries |
Vasospastic angina, variant angina, Prinzmetal's angina |
Angina precipitated by reversible spasm of coronary vessels |
Coronary vasodilator |
Older, incorrect name for drugs useful in angina; drugs that relieve angina of effort do not act primarily through coronary vasodilation; some potent coronary vasodilators are ineffective in angina |
Venodilator |
Drug that selectively dilates veins, eg, nitroglycerin |
"Monday disease" |
Industrial disease caused by chronic exposure to vasodilating concentrations of organic nitrates in the workplace; characterized by headache, dizziness, and tachycardia on Mondays |
Nitrate tolerance |
Loss of effect of a nitrate venodilator when exposure is prolonged |
Unstable angina |
Rapidly progressing increase in frequency and severity of anginal attacks, especially pain at rest; probably heralds imminent myocardial infarction |
Preload |
Filling pressure of the heart; determines end-diastolic fiber length and tension |
Afterload |
Resistance to ejection of stroke volume; determined by arterial blood pressure and arterial stiffness |
Intramyocardial fiber tension |
Force exerted, by myocardial fibers, especially ventricular fibers at any given time; a primary determinant of O2 requirement |
Double product |
The product of heart rate and systolic blood pressure; an estimate of cardiac work |
Myocardial revascularization |
Mechanical intervention to improve 02 delivery to the myocardium by angioplasty or bypass grafting |
Concepts pathophysiology of angina
Determinants of Cardiac Oxygen Requirement: The treatment of coronary insufficiency is based on physiologic factors that control the myocardial oxygen requirement. A major determinant is myocardial fiber tension, ie, the higher the tension, the greater the oxygen requirement (Figure 12-2).
Several variables contribute to fiber tension.
1. Preload: Preload (diastolic filling pressure) is a function of blood volume and venous tone. Because venous tone is mainly controlled by sympathetic outflow, activities that increase sympathetic activity usually increase preload.
2. Afterload: Afterload or arterial blood pressure is one of the systolic determinants of oxygen requirement. Arterial blood pressure depends on peripheral vascular resistance, which is determined by sympathetic outflow to the arteriolar vessels and other factors.
3. Heart rate: Heart rate contributes to time-integrated fiber tension because at fast heart rates, fibers spend more time at systolic tension levels; at faster rates, diastole is abbreviated, and diastole constitutes the time available for coronary flow (coronary blood flow is low or nil during systole). Systolic blood pressure and heart rate may be multiplied to yield the double product, a measure of cardiac work and therefore oxygen requirement. In patients with atherosclerotic angina, effective drugs reduce the double product.
4. Cardiac contractility: Force of cardiac contraction is another systolic factor controlled mainly by sympathetic outflow to the heart. Ejection time for ventricular contraction is inversely related to force of contraction but is also influenced by impedance to outflow. Increased ejection time increases oxygen requirement.
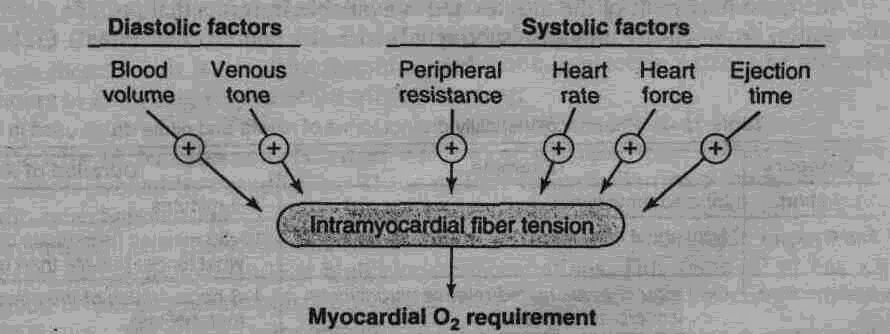
Figure 12-2. Determinants of MVO2, the minute volume of oxygen required by the heart. Both diastolic and systolic factors contribute to the MVO2; most of these factors are directly influenced by sympathetic discharge (venous tone, peripheral resistance, heart rate, and heart force).
B. Types of Angina: There are three forms of angina pectoris.
1. Atherosclerotic angina: Atherosclerotic angina is also known as angina of effort or classic angina. It is associated with atheromatous plaques that partially occlude one or more coronaries. When cardiac work increases (eg, in exercise), the obstruction of flow results in the accumulation of acidic metabolites and ischemic changes stimulate myocardial pain-mediating nerve endings. Atherosclerotic angina constitutes about 90% of angina cases and—depending on the rate of progression of the atheromas—may last for years with little change.
2. Vasospastic angina: Vasospastic angina is also known as variant angina or Prinzmetal's angina. It involves reversible spasm of coronaries, usually at the site of an atherosclerotic plaque. Spasm may occur at any time, even during sleep. Vasospastic angina may deteriorate into unstable angina.
3. Unstable angina: The third type of angina, unstable or crescendo angina, is caused by diminished coronary flow that results from a combination of atherosclerotic plaques, platelet aggregation at fractured plaques, and vasospasm. Unstable angina is thought to be the immediate precursor of a myocardial infarction and is treated as a medical emergency.
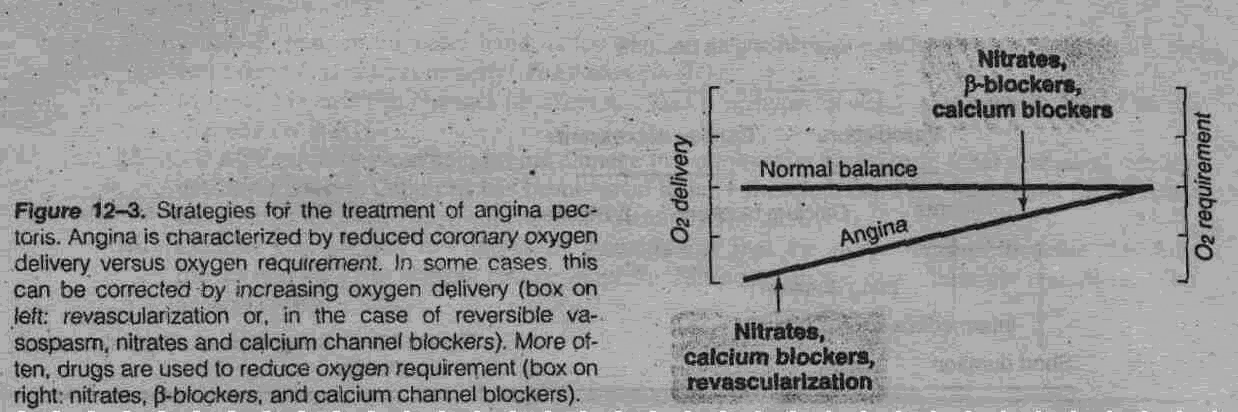
C.Therapeutic Strategies: The defect that causes anginal pain is coronary oxygen delivery inadequate for the myocardial oxygen requirement. This defect can be corrected in two ways: by increasing oxygen delivery or by reducing oxygen requirement (Figure 12-3). Pharmacologic therapies include the nitrates, the calcium channel blockers, and the beta-blockers. All three groups reduce oxygen requirement in atherosclerotic angina; nitrates and calcium channel blockers (but not beta-blockers) can also increase oxygen delivery by reducing vasospasm—but only in the Vasospastic form. Myocardial revascularization corrects coronary obstruction either by bypass grafting or by angioplasty (enlargement of the lumen by means of a special catheter).
NITRATES
Table 12-2. Pharmacokinetically distinct forms of nitrate and nitrite drugs used in angina. |
||
Category |
Example |
Duration of Action |
Very short |
Inhaled amyl nitrite |
3-5 minutes |
Short |
Sublingual nitroglycerin or isosorbide dinitrate |
10-30 minutes (isosorbide dinitrate has a somewhat longer half-life than nitroglycerin) |
Intermediate |
Oral regular or sustained-release nitroglycerin or isosorbide dinitrate |
4-8 hours (much of the effect is due to active metabolites) |
Long |
Transdermal nitroglycerin patch |
8-10 hours (blood levels may persist for 24 hours, but tolerance limits the duration of action) |
A.Classification and Pharmacokinetics: Nitroglycerin (the active ingredient in dynamite) is the most important of the nitrates and is available in forms that provide a range of durations of action from 10-20 minutes (sublingual) to 8-10 hours (transdermal) (Table 12-2). Because treatment of acute attacks and prevention of attacks are both important aspects of therapy, the pharmacokinetics of these different dosage forms are clinically significant. Nitroglycerin (glyceryl trinitrate) is rapidly denitrated in the liver—first to the dinitrate (glyceryl dinitrate), which retains a significant vasodilating effect, and more slowly to the mononitrate, which is much less active. Because of the high enzyme activity in the liver, the first-pass effect for nitroglycerin is large—about 90%. The efficacy of oral (swallowed) nitroglycerin probably results from the high levels of glyceryl dinitrate in the blood. The effects of sublingual nitroglycerin are mainly the result of the unchanged drug. Other nitrates are similar to nitroglycerin in their pharmacokinetics and pharmacodynamics. After nitroglycerin, isosorbide dinitrate is used most extensively; it is available in sublingual and oral forms. Isosorbide dinitrate is rapidly denitrated in the liver to isosorbide mononitrate, which like glyceryl dinitrate is active. Isosorbide mononitrate is available as a separate drug for oral use. Several other nitrates are available for oral use and, like the oral nitroglycerin preparation, have an intermediate duration of action (4-6 hours). Amyl nitrite is a volatile and rapidly acting vasodilator that was used for angina by inhalation but is now rarely prescribed.
B. Mechanism of Action: Denitration of the nitrates within smooth muscle cells releases nitric oxide (NO), which stimulates guanylyl cyclase, causes an increase of the second messenger cGMP, and leads to smooth muscle relaxation, probably by dephosphorylation of myosin light chain phosphate. Note that this mechanism is identical to that of nitroprusside (Chapter 11).
C. Organ System Effects:
1. Cardiovascular: Smooth muscle relaxation leads to peripheral venodilation, which results in reduced cardiac size and cardiac output through reduced preload. Reduced after-load—from arteriolar dilation—may contribute to an increase in ejection and a further decrease in cardiac size. Some studies suggest that of the vascular beds, the veins are the most sensitive, arteries less so, and arterioles least sensitive. Venodilation leads to decreased diastolic heart size and fiber tension. Arteriolar dilation leads to reduced peripheral resistance and blood pressure. These changes contribute to an overall reduction in myocardial fiber tension, oxygen consumption, and the double product. Thus, the primary mechanism of therapeutic benefit in atherosclerotic angina is reduction of the oxygen requirement; an increase in coronary flow in ischemic areas is less likely. In vasospastic angina, on the other hand, a reversal of coronary spasm and increased flow can be demonstrated. A significant reflex tachycardia is predictable when nitroglycerin reduces the blood pressure.
2. Other organs: Nitrates relax the smooth muscle of the bronchi, gastrointestinal tract, and genitourinary tract, but these effects are too small to be clinically useful. Intravenous nitroglycerin (sometimes used in unstable angina) reduces platelet aggregation. There are no significant effects on other tissues.
D. Clinical Uses: As previously noted, nitroglycerin is available in several formulations (Table 12-2). The standard form for treatment of acute anginal pain is the sublingual tablet, which has a duration of action of 10-20 minutes. Oral (swallowed) normal-release nitroglycerin has a duration of 4-6 hours. Sustained-release oral forms have a somewhat longer duration (Table 12-2). Transdermal formulations (ointment or patch) can maintain blood levels for up to 24 hours. Tolerance develops after about 8 hours, however, with markedly diminishing effectiveness thereafter. It is therefore recommended that nitroglycerin patches be removed after 10-12 hours to allow recovery of sensitivity to the drug.
E. Toxicity of Nitrates and Nitrites: The most common toxic effects of nitrates are the responses evoked by vasodilation. These include tachycardia (from the baroreceptor reflex), orthostatic hypotension (a direct extension of the venodilator effect), and throbbing headache from meningeal artery vasodilation. Nitrites are of greater toxicologic importance because they cause methemoglobinemia at high blood concentrations. This same effect has a potential antidotal action in cyanide poisoning (see below). The nitrates do not cause methemoglobinemia. In the past, the nitrates were responsible for several occupational diseases in munitions plants in which workplace contamination by these volatile chemicals was severe. The most common of these diseases was "Monday disease," or the alternating development of tolerance (during the work week) and loss of tolerance (over the weekend) for the vasodilating action, resulting in headache, tachycardia, and dizziness every Monday.
F. Nitrites in the Treatment of Cyanide Poisoning: Cyanide ion rapidly complexes with the iron in cytochrome oxidase, resulting in a block of oxidative metabolism and cell death. Fortunately, the iron in methemoglobin has a higher affinity for cyanide than does the iron in cytochrome oxidase. Nitrites convert the ferrous iron in hemoglobin to the ferric form, yielding methemoglobin. Therefore, cyanide poisoning can be treated by (1) immediate exposure to amyl nitrite, followed by (2) intravenous administration of sodium nitrite, which rapidly increases the methemoglobin level to the degree necessary to remove a significant amount of cyanide from cytochrome oxidase. This is followed by (3) intravenous sodium thiosulfate, which converts cyan-methemoglobin resulting from step 2 to thiocyanate and methemoglobin. Thiocyanate is much less toxic than cyanide and is excreted by the kidney. (It should be noted that excessive methemoglobinemia is fatal, since methemoglobin is a very poor oxygen carrier.)
