
fascia-neck
.pdf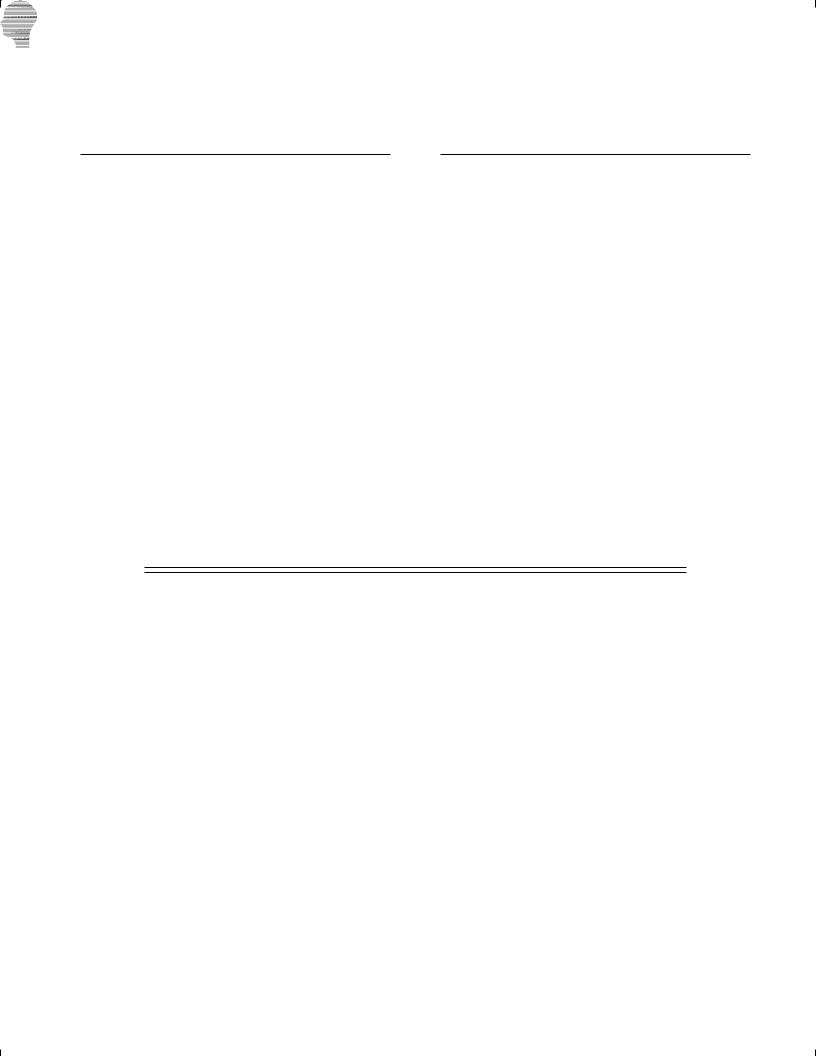
34
Fascia and Spaces of the Neck
Peter M. Som and Hugh D. Curtin
INTRODUCTION
THE FASCIAE
The Superficial Fascia
The Deep Cervical Fascia
The Superficial Layer of the Deep Cervical
Fascia
The Deep Layer of the Deep Cervical Fascia
Sibson’s Fascia
The Middle Layer of the Deep Cervical Fascia
in the Infrahyoid Neck
The Middle Layer of the Deep Cervical Fascia
in the Suprahyoid Neck
THE CAROTID SHEATH
THE FASCIAL SPACES
The Visceral Compartment and Its Spaces
The Pretracheal Space
The Retrovisceral Space The Danger Space
The Prevertebral Space The Carotid Sheath
The Space of the Body of the Mandible The Space of the Submandibular Gland The Space of the Parotid Gland
The Submandibular Space The Masticator Space
The Parapharyngeal Space The Peritonsillar Space The ‘‘Paravertebral Space’’
The ‘‘Posterior Triangle (Cervical) Space’’ SUMMARY AND CONCLUSION
INTRODUCTION
The importance of the fasciae of the neck is their ability to define spaces that may limit to some degree the spread of most infections and some tumors. However, these fasciae vary in thickness and composition, and they have been described in numerous forms by a variety of authors. In fact, the literature is filled with such varying descriptions of the anatomy of the cervical fasciae and spaces that there is confusion due to unclear statements and contradictory reports. As a sign of this frustration, Malgaigne in 1838 was prompted to note that ‘‘the cervical fasciae appear in a new form under the pen of each author who attempts to describe them.’’1–3
Part of the problem is that there is no consistent definition of what constitutes fascia. Fascia has been variously described in the literature as a collection of fat and fibrous tissue that seems to equate with a ‘‘fat layer’’; a thin but firm, well-defined layer of fibrous tissue such as an aponeurosis; and a localized thickening or condensation of fibroadipose tissue within a larger, more diffuse area of such tissue. This problem prompted Hollinshead to write: ‘‘If the reader will recall that there is no generally accepted definition as to how dense connective tissue must be before
it can be regarded as forming a fascia, and that fascial spaces are simply areas of relatively loose connective tissues, the reasons for many of the discrepancies in various descriptions will be obvious.’’4
Another part of the problem relates to the varied descriptions of the anatomic boundaries of the fasciae. However, when one considers that the fasciae may split to surround muscles, vessels, and nerves and then merge with other fascial layers, it becomes apparent that any description is somewhat arbitrary.2, 4 In addition, many of the smaller muscles have their own surrounding fascia, or epimysium, which is not necessarily considered to arise from any of the classic fascial layers.
The interest in the fasciae and spaces of the neck stems from early anatomic investigations performed by surgeons who were seeking ways to predict the spread of infection.5 They believed correctly that knowledge of such routes of spread would allow them to approach and drain abscesses more effectively. However, interest in this subject waned with the introduction of the antibiotic era and the advent of medical control of many of these infections. Hollinshead wrote in 1954, ‘‘It should be noted that with the widespread use of antibiotics, the anatomy of these spaces is necessarily becoming less important.’’4 But with the emergence of the
1805
Copyright © 2003, Mosby, Inc. All rights reserved.

1806 NECK
HIV pandemic within the past decades, the incidence of infections not well controlled by medical therapy has risen and the need to understand the fascial and spatial anatomy of the neck has again gained importance. Lastly, with the utilization of CT and MR imaging, it has been noted that the growth of some tumors appears to be restricted by certain fasciae, and knowledge of the anatomy of these fasciae allows one to predict such growth patterns.
This chapter reviews the major anatomic descriptions of the fasciae and spaces of the neck, mentions the various synonyms used for the fascia and spaces, points out areas of confusion and divergent description, and presents what the authors believe is the present understanding of this topic.1–15 Once the often complex anatomy of these fasciae is mastered, one can achieve a better understanding of the spread of both infections and some tumors in the neck.
THE FASCIAE
Traditionally, the fasciae of the neck are classified into two major divisions: superficial and deep. The superficial cervical fascia (SCF) is a fairly thick, well-defined, primarily fatty layer of relatively loose connective tissue that lies deep to the skin and superficial to the deep cervical fascia. The SCF covers the head, face, and neck and in its deeper portions contains the thin platysma muscles, the muscles of facial expression, and portions of the anterior and external jugular veins.
The deep cervical fascia (DCF) is more complex than the SCF and is made up of thinner but denser, better-defined discrete layers that are more deserving of the classic term fascial sheet. The DCF exists in the neck below the skull base and encloses the muscles of the neck, as well as the mandible and the muscles of mastication and deglutition.
The DCF is classically subdivided into three layers: (1) the superficial or investing layer of the deep cervical fascia (SLDCF), (2) the middle layer, which includes the pretracheal and visceral layers (MLDCF), and (3) the deep layer (DLDCF).2, 4 This terminology itself may lead to some confusion, as there is both an SCF and an SLDCF. Although these two layers border one another, they are distinctly separate entities.
In the literature, there is reasonable agreement, except for some minor variations, regarding the descriptions of the SCF, the SLDCF, and the DLDCF. Thus, most of the variations in the fascial descriptions concern the MLDCF, which is found between the more uniformly described SLDCF and DLDCF layers.
The Superficial Fascia
Deep to the skin and superficial to the SLDCF, the subcutaneous tissues of the head and neck are referred to as the SCF. This superficial fascia is not a fascial sheet in the classic sense, but rather a fatty, loose connective tissue in which are embedded the voluntary muscles of facial expression and the platysma muscles. The subcutaneous nerves, venules, and lymphatics are also within the SCF, and in some descriptions portions of the anterior and
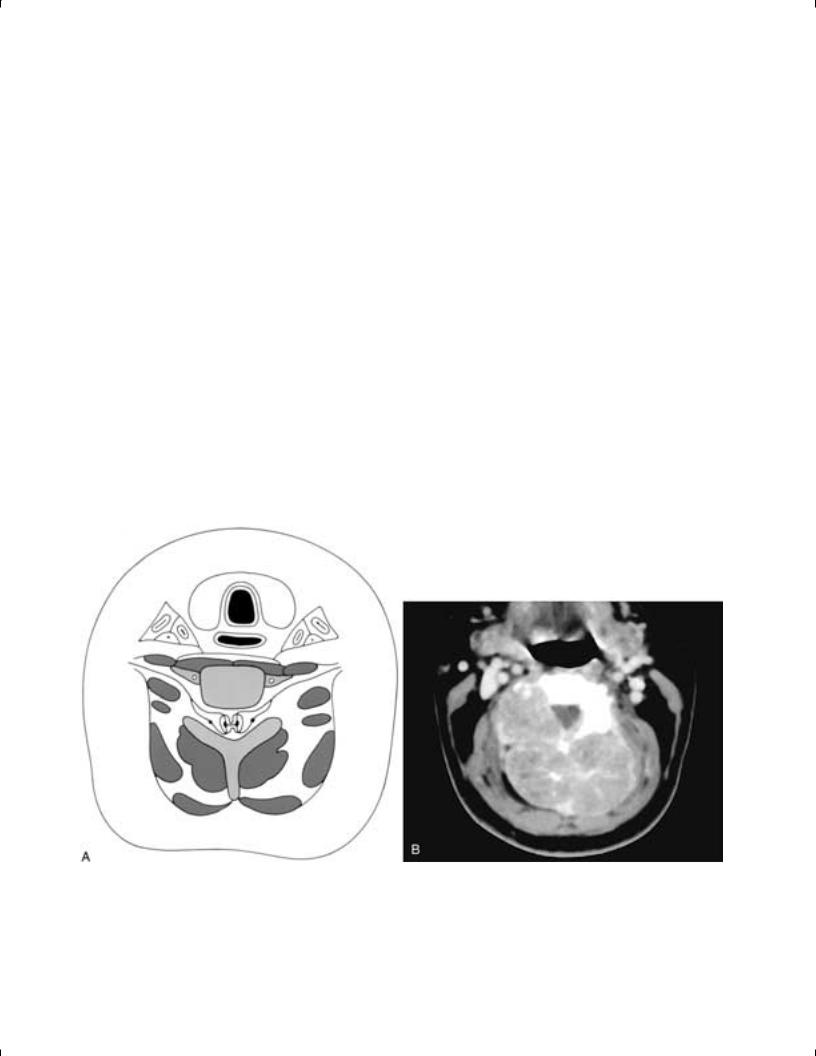
external jugular veins are included in the SCF (Drawings 1–5) (Fig. 34-1).2, 4
In the neck, the fat of the SCF is fairly loose. However, in the facial area the fat is much denser, except in the region of the eyelids, where it is fairly loose on both the superficial and deep aspects of the orbicularis oculi. In the scalp, the subcutaneous fat is dense and contains the epicranius (frontalis) muscle in its deep portion. Beneath the epicranial aponeurosis, between it and the periosteum of the calvarium, there is loose areolar tissue that permits motion of this muscle and, like the tissue about the eyelids, can hold large accumulations of fluid.2, 4
The skin, the SCF, and the platysma muscle function as a complex morphologic unit, interconnected by a system of fine connective tissue fibers and less well defined muscular elements called the superficial musculo-aponeurotic system (SMAS). Although the muscles of facial expression are often considered to be a separate functional unit, the SMAS interlinks these facial muscles with the dermis and amplifies the effect on the skin caused by the contractions of the facial muscles. The SMAS extends from the temporalis and frontalis muscles superiorly to the platysma muscle inferiorly. Thus, the SMAS has come to be considered an important functional unit in plastic surgery of the face and upper neck. Many surgeons consider the SMAS to be the most important component of a rhytidectomy and the factor that most contributes to a longer-lasting result.13
The Deep Cervical Fascia
Deep to the SCF, the DCF surrounds and encloses the musculature of the neck. The DCF is traditionally subdivided into three layers: the SLDCF, the MLDCF, and the DLDCF.
As mentioned, the various descriptions in the literature of the SLDCF and the DLDCF are fairly uniform. However, the layers between the SLDCF and the DLDCF are more arbitrarily described—at times being assigned to the MLDCF, at other times referred to as derivations of the SLDCF or the DLDCF, and at still other times considered to be separate fasciae that are not ascribed to any of these layers. This discussion of the DCF will start by describing the less controversial SLDCF and DLDCF. Then the ‘‘middle regions’’ and layers will be discussed, exploring the labyrinth of fascial webs and partitions found in the perplexing zone that separates the SLDCF and DLDCF.
The Superficial Layer of the Deep Cervical
Fascia
The SLDCF is a well-defined sheet of fibrous tissue that completely encircles the neck, incorporating the sternocleidomastoid and trapezius muscles and attaching posteriorly to the vertebral spines and ligamentum nuchae. This layer extends cranially into the face and caudally into the pectoral and axillary regions. The SLDCF may be thought of as arising from the cervical vertebral spines and the ligamentum nuchae. It extends to the left and right sides of the neck, splits to enclose each trapezius muscle, and then
Copyright © 2003, Mosby, Inc. All rights reserved.
Chapter 34 Fascia and Spaces of the Neck 1807
crosses the posterior triangle of the neck. The SLDCF then splits again to enclose each sternocleidomastoid muscle and finally crosses the anterior midline of the neck in front of the strap muscles as a single fascia connecting the anterior borders of the sternocleidomastoid muscles (Drawings 2–9) (Fig. 34-2).
Caudally in the midline, the SLDCF splits into two layers, one attaching to the anterior aspect and one to the posterior aspect of the manubrium. This creates the variably sized suprasternal space of Burns (or Gruber), which primarily contains fat and a communicating vein between the left and right anterior jugular veins (Drawings 8, 9). This space either can extend nearly halfway up the neck or can be localized to just above the manubrium. The clinical importance of this space lies in the fact that if it is entered during a tracheostomy, inadvertent transection of the communicating vein may result in considerable blood loss.2, 14 Although of minor importance, even the small suprasternal space of Burns is somewhat controversial, as some authors describe the posterior layer of this space as being formed from the MLDCF.2 Lateral to the sternum, the SLDCF attaches to the superior margin of each clavicle
FIGURE 34-1 Axial diagram of the neck (A) showing the SCF with the platysma and portions of the anterior and external jugular veins within it. Axial CT scan of the neck (B) in an obese patient shows a large volume of subcutaneous fat in the SCF. Note that there is no specific organization to this fat into distinct areas, such as in a lipoma or as seen in Madelung’s disease (see Chapter 41). Axial contrast-enhanced CT scan (C) shows an area of subcutaneous thickening and injection overlying the left platysma muscle (arrow), which is also thickened. This is a localized cellulitis confined to the SCF layer.
along the entire extent of this bone. Even more laterally, the fascia attaches to the acromion and spine of each scapula. Most portions of the anterior and external jugular veins are considered to be embedded in the superficial surface of the SLDCF, rather than lying between it and the deeper fascial layers. As mentioned, small portions of these veins also extend into the SCF.
The literature also contains ambiguity regarding the origin of the fascia around the strap muscles (sternothyroid, sternohyoid, and thyrohyoid muscles). Although some authors believe this fascia to be part of the SLDCF, most authors refer to it as being part of the MLDCF.2, 4 However, the MLDCF has in turn been described as either encircling the strap muscles or as comprising only the most posterior layer of fascia, deep to the strap muscles.4 There is also some controversy over the origin of the fascial sling between the superior and inferior bellies of the omohyoid muscle. This sling is attached below to the clavicle and first rib and maintains the angulated course of this muscle. Some authors believe the sling is formed by the SLDCF, while most other authors believe it is formed by the sternohyoid-omohyoid layer of the MLDCF.2, 4 What is clearly apparent is that
Copyright © 2003, Mosby, Inc. All rights reserved.
1808 NECK
these are only differences in nomenclature, and there is no controversy over the presence and location of these fascial planes and slings.
Above the hyoid bone, the SLDCF extends to the lower border of the mandible, and as this fascia passes over the muscles below the floor of the mouth, it fuses with the fascial covering of each digastric muscle. Grodinsky and Holyoke consider the fasciae about the anterior belly of each digastric muscle, the mylohyoid, the geniohyoid, the hyoglossus, and the genioglossus muscles to be separate fasciae related to each of these muscles and not actually part of the SLDCF.2 However, more posteriorly these same authors considered the fascial sheaths of the posterior belly of the digastric muscles and the stylohyoid muscles to be direct derivatives of the SLDCF.
On either side of the neck in the submandibular triangle, a
portion of the SLDCF splits to form a thin, often flimsy capsule about each submaxillary gland (Drawing 10). Then, as the SLDCF reaches the mandible, the fascia divides into superficial and deep leaflets. These leaflets extend superiorly, enclosing the muscles of mastication and forming the masticator spaces.7, 12, 15, 16
The superficial leaflet, or fascial sheet, overlies the masseter muscle and attaches to the zygomatic arch. The fascia here splits once again to enclose the zygomatic arch and creates a small space on the cranial surface of the arch that is filled with fat. The superficial fascial leaflet then continues cranially to overlie the temporalis muscle, attaching along the temporal ridge cranially and dorsally and along the lateral orbital margin ventrally (Drawings 10–13).
Anteriorly, the fascia covering the masseter muscle curves medially to attach to the mandible and to the fascia of
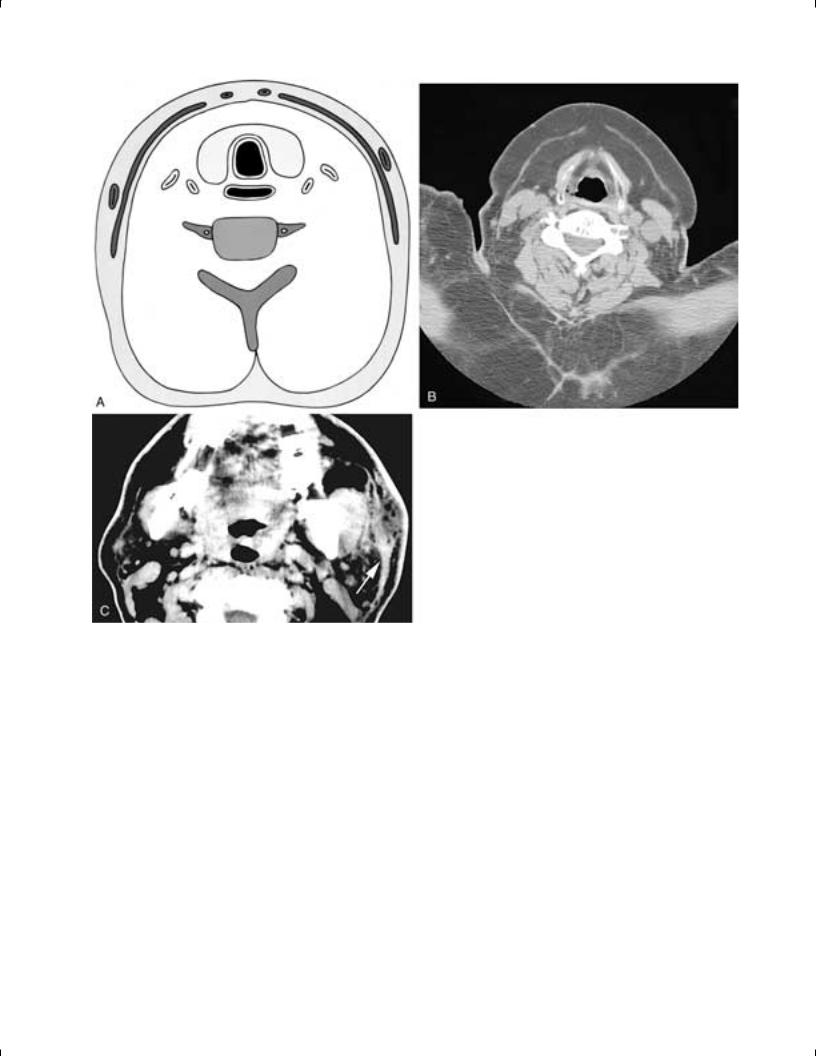
FIGURE 34-2 Axial drawing of the neck (A) shows the SLDCF extending from the spinous process ventral about the trapezius and sternocleidomastoid muscles and then extending over to the strap muscles. This layer is immediately deep to the SCF. The contributions of the SLDCF, the MLDCF, and the DLDCF to the carotid sheath can be seen. Axial contrast-enhanced CT scan (B) shows a left second branchial cleft cyst. Although the cyst, when small, was situated primarily along the anterior edge of the sternocleidomastoid muscle, as the cyst enlarged it was ‘‘pushed’’ back by the SLDCF (extending from this muscle toward the strap muscles) so that the majority of the mass is now deep to the muscle. Although the SLDCF itself is not seen, the effect of this fascia is evident. Axial T2-weighted MR image (C) of the neck shows a nonhomogeneous high signal intensity mass in the posterior right neck. Although this hemangioma bulges posteriorly, it is contained by the SLDCF as it extends from the sternocleidomastoid muscle to the spinous process of the cervical vertebra. As in B, although the SLDCF itself is not seen, the effect of this fascia is evident.
Copyright © 2003, Mosby, Inc. All rights reserved.
Chapter 34 Fascia and Spaces of the Neck 1809
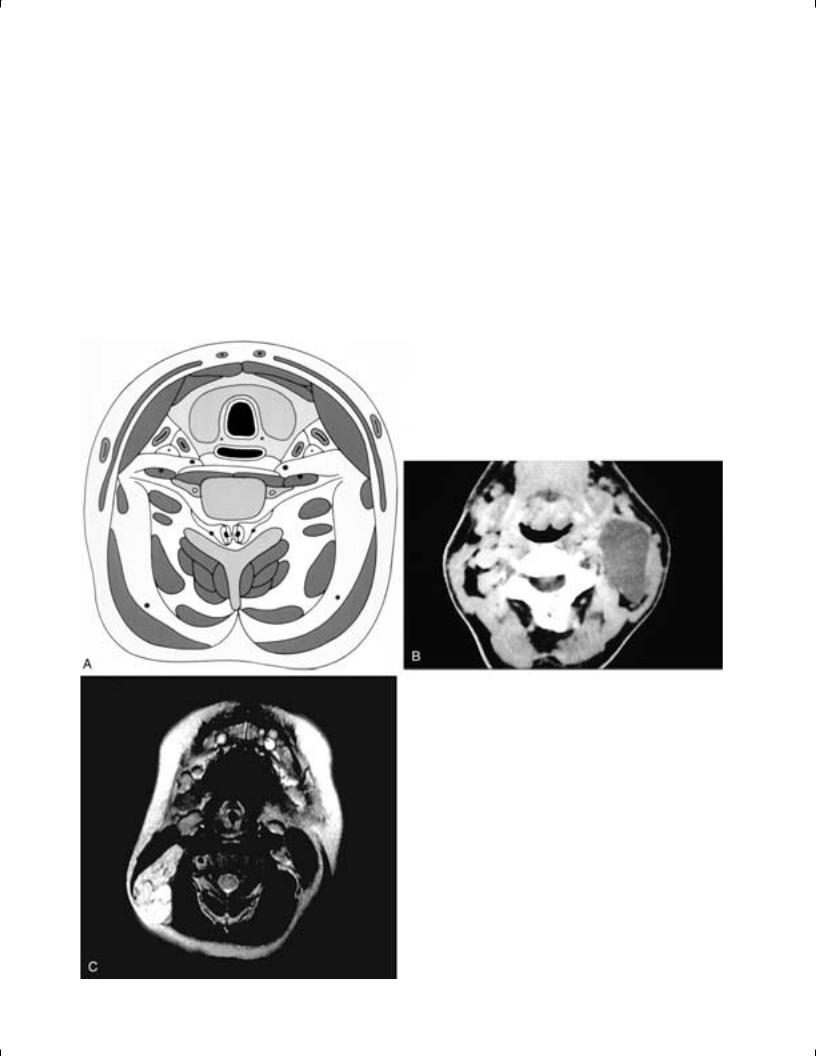
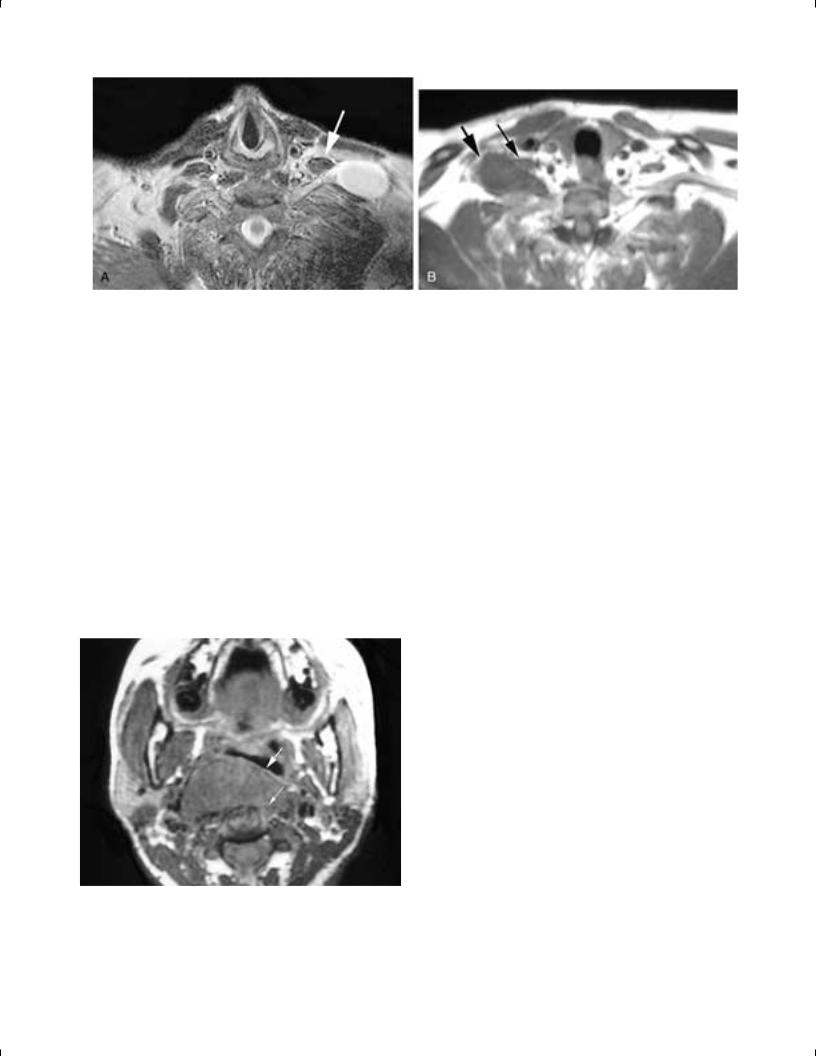
FIGURE 34-3 Coronal T1-weighted MR image (A) of a patient with a rhabdomyosarcoma in the left masticator space. Although this is an aggressive tumor, the deep (white arrow) and superficial (black arrow) leaflets of the SLDCF contain the tumor. In this instance, the integrity of the fascia belies the aggressive nature of the tumor. Axial T1-weighted MR image (B) shows an infiltrating mass in the right masticator space (arrowhead ). Both the superficial and deep layers of the masticator space fascia have been violated, attesting to the invasive nature of this breast carcinoma metastasis.
the temporalis tendon and muscle as it attaches to the coronoid process of the mandible.17 Fascia also extends from the temporalis muscle to the buccinator fascia near the pterygomandibular raphe. However, in some reports, a separate fascial leaflet is described as passing from the anterior margin of the masseter muscle directly to the buccinator fascia.17, 18 In one or another of these ways, the fascia covering the masseter muscle attaches to the buccinator fascia and to the maxilla, and in so doing it encloses a small fat pad referred to as the masticator fat pad. This fat pad is intimately associated with the masticator space, often being included as part of the space, and the fat has small projections into the pterygopalatine fossa as well as along the lateral pterygoid muscle. Thus, these various fasciae, either with or without the masticator fat pad, attach to the maxilla and to the buccinator fascia and, in so doing, close the masticator space anteriorly (Drawings 2 and 12) (Fig. 34-3).
Just as the superficial leaflet of the SLDCF forms the outer boundary of the masticator space, the deep leaflet of the SLDCF extends cranially to form the medial or inner boundary of this space. The fascial covering of the medial pterygoid muscle is fairly thin, but does attach to the lower border of the mandible and thus can be considered a derivation of the SLDCF. A stronger fascia, the interpterygoid fascia (also probably derived from the SLSCF), attaches to the inner surface of the mandible, medial to the insertion of the medial pterygoid muscle. From here the interpterygoid fascia sweeps cranially to the superior edge of the medial pterygoid muscle, where the fascia covering the medial surface of the muscle fuses with the interpterygoid fascia. The resultant combined fascia continues up to the skull base and attaches along a line that extends from the root of the medial pterygoid plate to the sphenoid spine, just medial to the foramen ovale. The fascia then curves posterolaterally to reach the posterior glenoid fossa. The sphenomandibular ligament, which extends from the sphenoid spine to the ramus of the
mandible, is a localized thickening of the interpterygoid fascia.
The superficial and deep leaflets of the SLDCF also fuse along the dorsal border of the mandibular ramus. The space thus enclosed by these leaflets contains the muscles of mastication (the temporalis, masseter, and pterygoid muscles). It was first described by Juvara in 1870 and was first called the masticator space by Coller and Yglesias in 1935 (Drawings 2 and 10–13) (Fig. 34-3).2, 4, 7, 12
On either side of the neck, between the angle of the dorsal edge of the mandibular ramus and the ventral border of the sternocleidomastoid muscle, the SLDCF splits again to form the capsule of the parotid gland. The deep layer, in particular, is quite thin and flimsy and in the opinion of many investigators is actually deficient. The external carotid artery, with adherent prolongations from the carotid sheath, and the posterior facial vein (retromandibular vein) each perforate the parotid gland capsule and pass through the substance of this gland (Drawings 2 and 12).2 The SLDCF then attaches to the mastoid process of the skull and extends dorsally to attach to the external occipital protuberance.
The Deep Layer of the Deep Cervical Fascia
The DLDCF, like the superficial layer, can be considered to originate from the cervical vertebral spinous processes and the ligamentum nuchae. The fascia then extends to either side, covering and investing the muscles that form the floor of the posterior triangle of the neck. These muscles are, from dorsally to ventrally, the splenius capitis, the levator scapulae, and the posterior, middle, and anterior scalene muscles. The portion of the fascia that relates to the scalene muscles is often called the scalene fascia. On either side of the neck as the DLDCF extends between the middle and anterior scalene muscles, the fascia is reflected outward, forming a sleeve around
Copyright © 2003, Mosby, Inc. All rights reserved.
1810 NECK
the brachial plexus and subclavian artery, which are all situated between these muscles. More laterally, this sleeve becomes the axillary sheath (Drawings 2–5, 7–9, and 14–16) (Fig. 34-4).
More specifically, the posterior scalene muscle arises from the posterior tubercles of the transverse processes of C4–C6 and the middle scalene muscle arises from the posterior tubercles of the transverse processes of the C2–C7 cervical vertebrae. By comparison, the anterior scalene muscle arises from the anterior tubercles of the transverse processes of C3–C6, and the respective anterior cervical nerve roots exit through the sulci or canals between the anterior and posterior tubercles. More caudally in the neck, the subclavian artery also passes between the anterior and middle scalene muscles. Thus, as the DLDCF extends ventrally over the middle and posterior scalene muscles, this fascia attaches to the origins of these muscles on the posterior tubercles of the transverse processes of the cervical vertebrae. The DLDCF then is reflected outward over the anterior cervical nerve roots and the subclavian artery (Fig. 34-5). Ventrally, the DLDCF then attaches again to the anterior tubercles about the origins of the anterior scalene muscle. The fascia then extends around the anterior scalene muscles, where it splits into two layers, both of which cross the anterior surface of the cervical vertebral bodies essentially extending between the anterior tubercles of the transverse processes on either side.
The dorsal layer, or the prevertebral fascia, lies closest to
the vertebral bodies and covers the anterior surface of the longus capitis and colli muscles. This fascia extends from the skull base to the coccyx, and the proximal portion of each phrenic nerve lies deep to the prevertebral fascia on the anterior face of each anterior scalene muscle. The ventral layer, or alar fascia, lies anterior to the prevertebral fascia from which it is separated by loose connective tissue.2 The alar fascia extends from the skull base caudally to a level between the sixth cervical and the fourth thoracic vertebrae, usually at the level of the seventh cervical vertebra, at which point it merges with the more anterior visceral fascia (see the discussion of the MLDCF) (Drawings 2–5, 8, 9, and 15) (Fig. 34-6).4
Charpy originally described a small, sagittally oriented fascial sheet that, on either side of the neck, extended from the fusion line of the DLDCF on the anterior tubercles of the cervical vertebrae ventrally toward the fascia over the posterolateral pharyngeal wall. He called this fascia the cloison sagittale, or sagittal partition, and it in effect separated the midline retropharyngeal and danger spaces from the more lateral parapharyngeal spaces.1, 10
However, 7 years later, Dean referred to this sagittal partition as the alar fascia and thus created confusion in terminology.19 It was not until 19 years later that Grodinsky and Holyoke described the alar fascia as a coronally oriented fascial sheet that was parallel to and ventral to the prevertebral fascia.2 Today, this coronally oriented fascia is generally accepted as the alar fascia, while the fascia
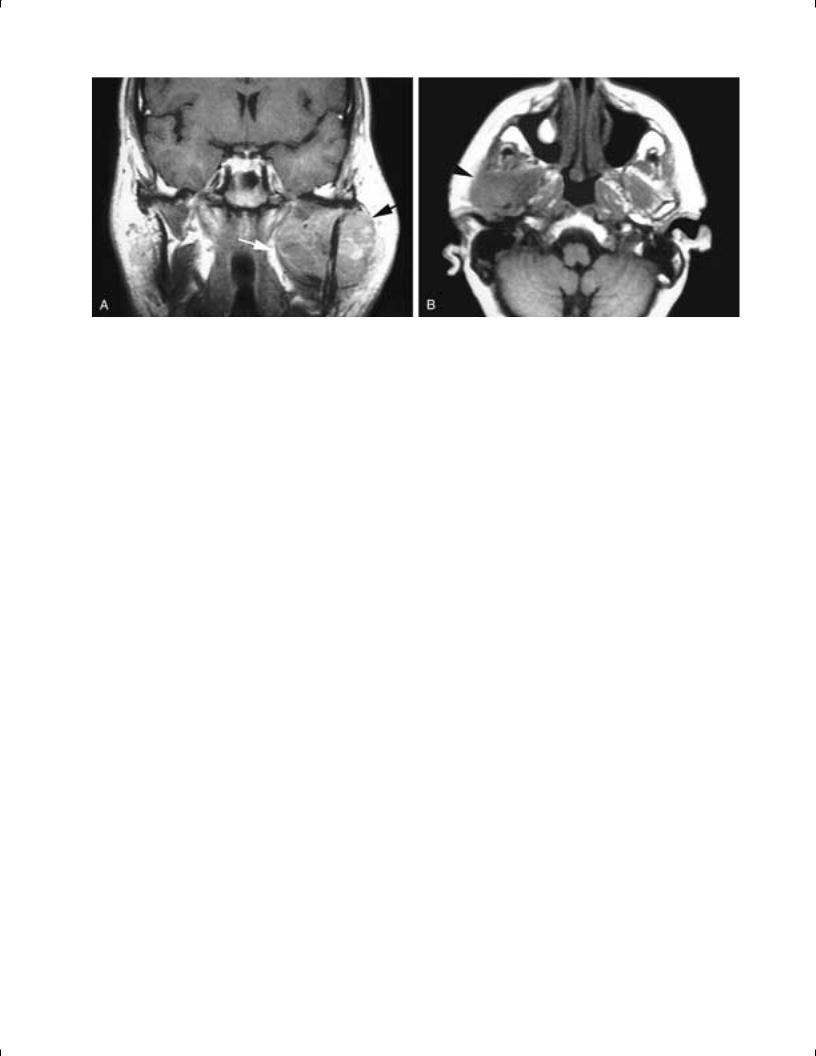
FIGURE 34-4 Axial drawing of the neck (A) shows the DLDCF extending from the spinous process over the muscles of the floor of the posterior triangle of the neck. After splitting to form the sheath about the brachial plexus and subclavian artery, the fascia attaches to the cervical vertebra. Ventrally, one layer of the DLDCF extends across the face of the flexor muscles of the cervical spine (prevertebral fascia). A second layer of fascia (alar fascia) also crosses the vertebral body and extends just ventral to the prevertebral fascia. These two layers form the boundaries of the danger space. Slips of fascia extend from the alar fascia (DLDCF) to contribute to the carotid sheath. Axial contrast-enhanced CT scan (B) of the neck shows a destructive lesion involving the right side of the cervical vertebra and all the muscles of the floor of the posterior triangles of the neck. Despite the aggressive nature of this metastatic breast cancer, the DLDCF contains the tumor.
Copyright © 2003, Mosby, Inc. All rights reserved.
Chapter 34 Fascia and Spaces of the Neck 1811
FIGURE 34-5 Axial T1-weighted, contrast-enhanced MR image (A) shows a schwannoma of the left brachial plexus. The thickened proximal nerve is seen extending toward the spinal cord, directly dorsal to the anterior scalene muscle (arrow). The DLDCF extends from the adjacent muscles of the floor of the posterior triangle of the neck out over the brachial plexus as a sheath, which more caudally also contains the subclavian artery. Axial T1-weighted MR image (B) shows a schwannoma of the right brachial plexus (large arrow) situated just dorsal to the anterior scalene muscle (small thinner arrow). This case illustrates how the anterior scalene muscle is a good marker for identifying the location of the brachial plexus in this region of the neck.
described by Dean is probably best referred to as the cloison sagittale, as described by Charpy.
Sibson’s Fascia
On either side of the neck, the DLDCF extends laterally from the transverse process of the seventh cervical vertebra, covers the dome of the pleura, and then attaches to the medial surface of the first rib. This fascia, called Sibson’s fascia, serves as a plane of separation between the lower neck and the thorax .2, 4, 14
FIGURE 34-6 Axial T1-weighted MR image shows a mass involving the flexor muscles of the cervical spine (small thinner arrow) and pushing the pharyngeal constrictors forward (large arrow). This schwannoma was in the prevertebral space, pushing the danger and retropharyngeal spaces forward. Because the actual fascia (prevertebral, alar, and visceral) cannot be routinely seen on imaging, the involvement of the prevertebral muscles indicates the space of origin of the mass.
The Middle Layer of the Deep Cervical Fascia in the Infrahyoid Neck
As mentioned, the MLDCF is the most arbitrarily described of the fascial layers. Although originally described only as the fascia in the neck that takes its origin from the fascial covering of the omohyoid muscle, the term middle layer of the deep cervical fascia was subsequently used to describe the fascia associated with the strap muscles and the ‘‘visceral’’ fascia surrounding the esophageal and pharyngeal walls.
Hollinshead stated that the MLDCF most commonly is the fascia between the sternocleidomastoid muscles that passes behind the strap muscles, thus lying in front of the thyroid gland and trachea.4 This description and relationship gave rise to the term pretracheal fascia. However, Grodinsky and Holyoke considered the MLDCF to be more complex and composed of three layers.2 The first layer was called the sternohyoid-omohyoid layer, and it formed the sling of the omohyoid muscle and the fascia of the sternohyoid and omohyoid muscles. The second layer was called the sternothyroid-thyrohyoid layer, and it formed the fascia about these muscles. This layer was the one most analogous to the pretracheal fascia. The third layer was the deepest or most central of the three layers and was called the visceral or buccopharyngeal fascia (BPF). This last layer was closely adherent to the muscular walls of the esophagus and pharynx (Drawings 3–5, 7, 8, 15, and 16).
Whether one considers all of the fascia about the strap muscles to be formed by the MLDCF or the SLDCF, or instead believes that the MLDCF forms only the fascial layer deep to the strap muscles, is purely an academic issue. Regardless of the fascial derivation, the fascia about these muscles extends caudally behind the sternum to the origin of these muscles and then fuses with the fibrous pericardium as it is prolonged out along the great vessels and their adventitia in the superior mediastinum. This inferior fusion occurs at about the level of the fourth thoracic vertebra.
Copyright © 2003, Mosby, Inc. All rights reserved.
1812 NECK
Cranially, this fascia fuses with the thyroid cartilage and the hyoid bone. Laterally, the fascia fuses with and contributes to the carotid sheath on either side of the neck.
The term visceral fascia refers to the layer of the MLDCF that is adherent to the outer surface of the esophagus and pharynx. This fascia is best defined at the level of the upper pharynx, and in this location it is often referred to as the buccopharyngeal fascia, which not only adheres to the outer surface of the pharyngeal constrictors but extends ventrally via the pterygomandibular raphe over the buccinator muscles.
Confusion was introduced when Grodinsky and Holyoke also stated that below the level of the thyroid cartilage, the ‘‘visceral fascia’’ surrounded not only the esophagus, but also the trachea and thyroid gland. They described a space (their space 3) that contained a small amount of loose adipose tissue and existed between the outer surface of this visceral fascia and the fasciae covering the inner surface of the strap muscles ventrally (SLDCF and/or MLDCF), the carotid sheaths laterally (all layers of the DCF contribute to this sheath), and the alar fascia (DLDCF) dorsally (Drawings 3–5, 7 and 8). However, Grodinsky and Holyoke referred to the structures within their visceral fascia (including the esophagus, trachea, and thyroid gland) as being in a visceral space (see discussion in the section on The Fascial Spaces).
Other authors, including Hollinshead, found it difficult to consider the loose, often incomplete connective tissue about the esophagus, trachea, and thyroid gland as a layer of fascia.4 They considered the fascia immediately about the cervical esophagus and pharynx either to be the only true visceral fascia or to be analogous to the subperitoneal connective tissue of the serous coat of the thoracic esophagus and the bowel.4 The trachea was considered to have its own fascia, and the thyroid gland capsule was considered to develop from the thyroid anlagen. These authors, in general, considered the visceral fascia of the esophagus and pharynx to be the deep division of the MLDCF and the fascia about the trachea, thyroid gland, and surrounding loose connective tissue not to be part of the MLDCF. Today, this is the view that is most commonly held.
Again, these are problems of nomenclature. There is no dispute that in the lower neck there is a thyroid gland capsule, a filmy loose connective tissue around the thyroid gland, trachea and cervical esophagus that is incomplete or absent in many people but that has a fairly consistent thickening on each side between the posterior margin of the thyroid gland and the esophagus. There also is a betterdefined fascia about the cervical esophagus (which extends cranially to surround the pharynx) and a surrounding, less well defined connective tissue zone.
The Middle Layer of the Deep Cervical Fascia in the Suprahyoid Neck
Although the controversies concerning the fasciae in the infrahyoid neck are of limited clinical concern, the fasciae of the suprahyoid neck figure prominently in discussions of the clinically important retropharyngeal and parapharyngeal spaces. Critical to any discussion of this fasciae is an
understanding of the anatomy of the cranial portion of the pharynx, the attachments of the tensor and levator veli palatini muscles to the skull base, and the relationship of these muscles to the eustachian tube as the visceral fascia attaches to and surrounds these structures.
The superior pharyngeal constrictor muscle attaches dorsally to the skull base at the midline pharyngeal tubercle via an aponeurosis. From this point, on either side, the muscle arches caudally to attach to the lower portion of the medial pterygoid plate. This arching shape results in a gap on either side of the midline between the skull base and the upper surface of the superior constrictor muscle. This gap is almost entirely filled by the thick pharyngobasilar fascia, which can be considered as the cranial continuation of this muscle and which helps define and restrict the shape of the nasopharynx.2, 4 On either side, just under the skull base and dorsal to the posterior edge of the medial pterygoid plate, the pharyngobasilar fascia is deficient, creating a space known as the sinus of Morgagni, through which passes the cartilaginous portion of the eustachian tube and the levator veli palatini muscle (Drawings 2 and 13–16).
The levator veli palatini muscle arises from the undersurface of the petrous apex and the medial lamina of the cartilaginous eustachian tube. This muscle then passes through the sinus of Morgagni in the pharyngobasilar fascia, descending submucosally along the inner surface of the pharyngeal constrictor to finally reach the soft palate. Once through the sinus of Morgagni, the levator veli palatini muscle has been described as being enclosed in a fascial space ‘‘la loge peristaphyline interne’’ (box or space of the levator palatini) that is formed by small medial and lateral leaves of the BPF at the skull base, the skull base itself, the eustachian tube, and the pharyngobasilar fascia. The muscle moves freely within this fascial space, is partly responsible for maintaining the patency of the eustachian tube, and is an integral part of the pharyngeal wall. It is best considered as a part of the pharynx and is innervated by the pharyngeal plexus (Fig. 34-7).
The tensor veli palatini muscle arises from a scaphoid fossa and spine of the sphenoid bone near the base of the medial pterygoid plate and from the lateral lamina of the cartilaginous eustachian tube. It then descends lateral to the pharyngeal constrictor, between the medial pterygoid plate and the medial pterygoid muscle, which arises in the pterygoid fossa. Its tendon then wraps around the hamulus of the medial pterygoid plate, and the muscle inserts into the palatine aponeurosis. The tensor veli palatini muscle, which remains outside of the pharynx, is best considered to be part of the muscles of mastication and is supplied by the fifth cranial nerve. This muscle also helps maintain the patency of the eustachian tube and, as noted, is really part of the deglutitional group of muscles.
The visceral fascia or BPF extends from the skull base and follows the outer surface of the pharyngobasilar fascia and the pharyngeal constrictors. This fascia is firmly adherent to the muscular wall of the pharynx and the esophagus, and no real space exists between this fascia and the viscera. However, this potential space has caused some confusion in the literature because it has also been referred to as the visceral space. Today the visceral space is generally considered to be the space between the BPF and the alar fasciae (see the discussion in the section on The Fascial
Copyright © 2003, Mosby, Inc. All rights reserved.
Chapter 34 Fascia and Spaces of the Neck 1813
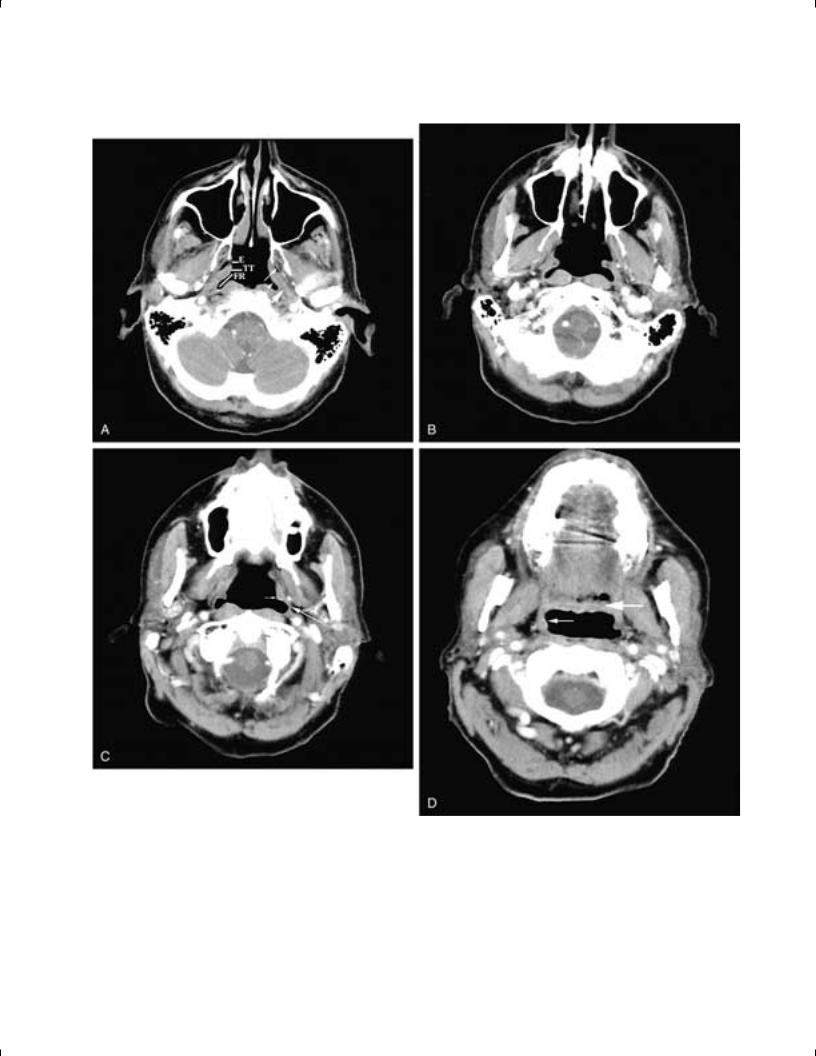
FIGURE 34-7 Axial sequential contrast-enhanced CT scans extending from cranially (A) to caudally (D). In A, the fossa of Rosenmueller (FR), the torus tubarius (TT ), and the opening of the eustachian tube (E ) are shown. The tensor velli palatini muscle (small arrow) is seen lateral to the pharyngeal constrictors (arrowhead ). The tensor muscle remains outside the pharynx until its tendon extends around the hamulus of the medial pterygoid plate to reach the soft palate. The levator velli palatini muscle (large arrow) is seen extending from the skull base to lie within the pharyngeal constrictors. In B, the levator velli palatini muscle is seen extending caudally from the torus tubarius. In C, the tapering levator velli palatini muscle (small arrow) is seen within the pharyngeal constrictors (large arrow). In D, the caudal levator velli palatini muscle (small arrow) is seen heading toward the soft palate (large arrow), all within the pharyngeal constrictors.
Copyright © 2003, Mosby, Inc. All rights reserved.
1814 NECK
Spaces) (Fig. 34-8). This current usage is virtually the opposite of that of Grodinsky and Holyoke.
Descriptions of the most superior visceral fascial attachments vary, with most authors indicating that the BPF has an intimate association with the eustachian tube and the levator veli palatini muscle. The BPF splits to enclose the more cranial portion of the levator muscle, and a lateral leaflet is sometimes described in association with the lateral margin of the tensor veli palatini muscle. According to most authors, a well-defined, fairly thick fascial sheet arises directly from the posteroinferior edge of the tensor veli palatini muscle and extends caudally and posterolaterally from this muscle to the styloid process and the styloid muscles, fusing inferiorly with the fascia covering the styloglossus muscle.9, 16, 20 This fascial sheet thus closes the gap between the tensor veli palatini, the skull base (from the sphenoid spine along the medial side of the foramen ovale to the root of the medial pterygoid plate), and the styloid process with its associated musculature. Anteriorly this fascia reaches the pterygomandibular raphe and there fuses with the interpterygoid fascia as well as the BPF.
In the English literature this important fascia has been described by Gaughran, who referred to it as the vascular fascia because it contains the ascending palatine artery and vein.9 Other names given to this fascia include the nerve-vessel sheath of Weintraub, the lame vasculaire, and the lateral aponeurosis of the pharynx.9, 21, 22
As to the origin of this fascia, it is clearly located between the SLDCF and the DLDCF and it is immediately contiguous with the BPF, which is derived from the MLDCF. However, the subclassification of the DCF into three different layers is not usually applied to the region above the hyoid bone and is rarely utilized in the area under the skull base. Some authors believe it to be part of the MLDCF; other authors describe it as an independent fascial layer. In either case, its derivation is less important than knowledge of its existence and its location. In this discussion, we will refer to this fascia by the anatomi-
cally descriptive name tensor-vascular-styloid fascia. This fascia plays a key role in the descriptions of the parapharyngeal space, as discussed in Chapter 38 (Drawings 2, 13–16).
THE CAROTID SHEATH
Most authors have described the primary fascial contributions to the middle and lower carotid sheath as coming from the SLDCF (from the fascia covering the sternocleidomastoid muscle) and from the DLDCF (from the alar fascia). There also may be contributions to the sheath from the MLDCF about the strap muscles (this fascia is variously thought to come from either the SLDCF or the MLDCF). Overlapping of these fascial contributions occurs in some areas, giving added strength to that portion of the carotid sheath, while in other areas there may be focal dehiscences, especially along the medial wall (Drawings 2–5, 8, 15 and 16).
The upper portion of the carotid sheath remains a composite compartment formed by the various regional fasciae. Typically, the upper carotid sheath is described as being formed by the SLDCF (represented by contributions from the adjacent muscular investing fasciae) that forms the lateral wall, the DLDCF (represented by the alar and/or prevertebral fasciae) that forms the posterior wall, the cloison sagittale (either part of the DLDCF or the MLDCF) that forms the medial wall, and the stylopharyngeal aponeurosis or the tensor-vascular-styloid fascia (MLDCF) that forms the anterior wall (see the discussion below).
There is general agreement among anatomists and surgeons that in the neck, caudal to the carotid artery bifurcation, the carotid sheath is a complete, well-defined structure. However, more cranially, many authors describe the internal carotid artery as being in an incomplete sheath with variable areas of dehiscence (Fig. 34-9).
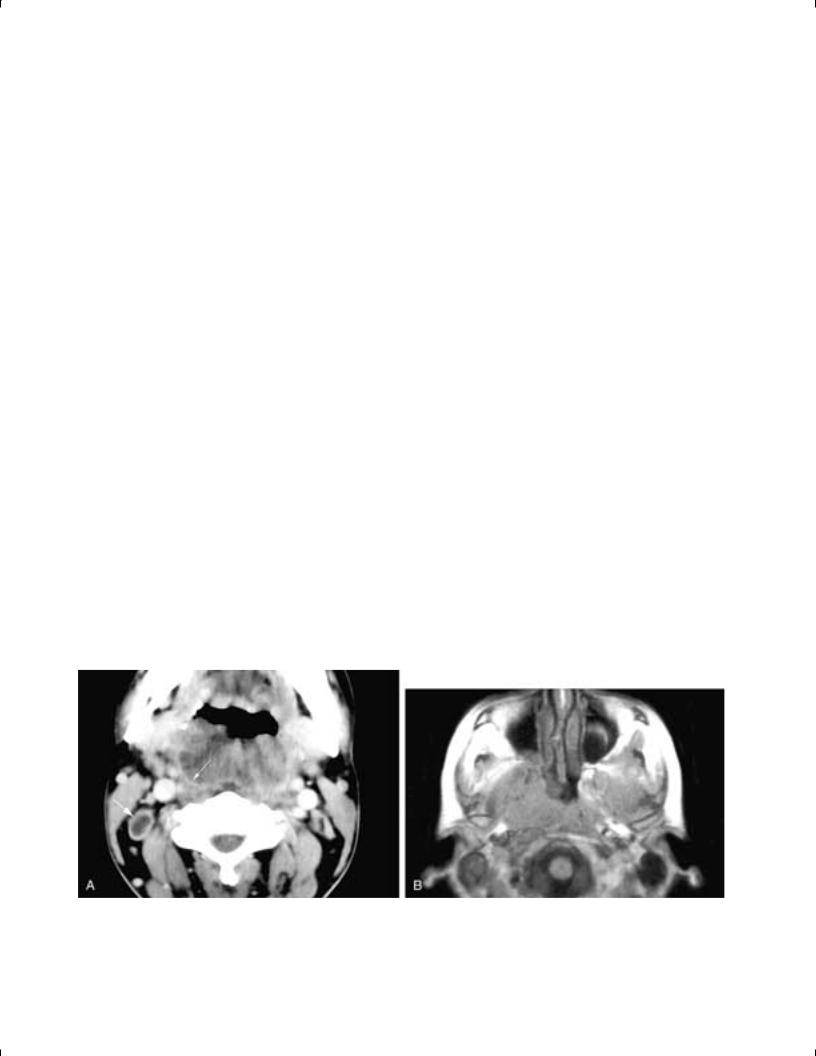
FIGURE 34-8 Axial contrast-enhanced CT scan (A) shows a large, bulky tumor in the pharynx. The visceral fascia around the pharyngeal constrictor muscles can be seen containing the tumor (small arrow). This imaging appearance is not uncommon with pharyngeal tumors and often belies the malignant nature of the tumor. However, a necrotic right level II node is present (large arrow), attesting to the aggressive nature of the cancer. Axial T1-weighted MR image (B) shows an infiltrative nasopharyngeal tumor that has violated the visceral fascia. The penetration of this fascia signifies the aggressive nature of the carcinoma.
Copyright © 2003, Mosby, Inc. All rights reserved.
