
5 курс / Пульмонология и фтизиатрия / Clinical_Manifestations_and_Assessment_of_Respiratory
.pdf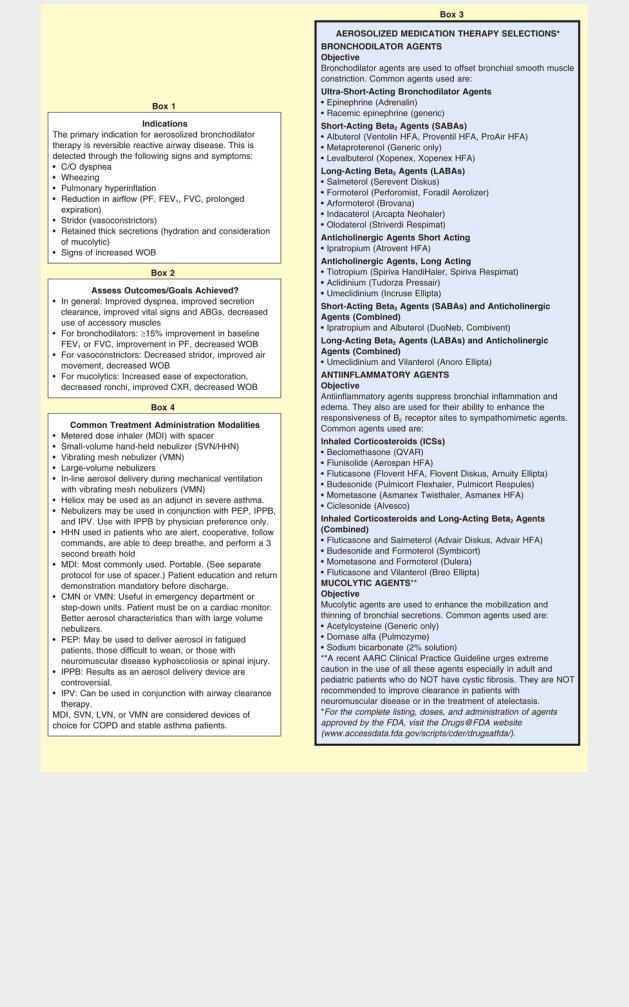
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
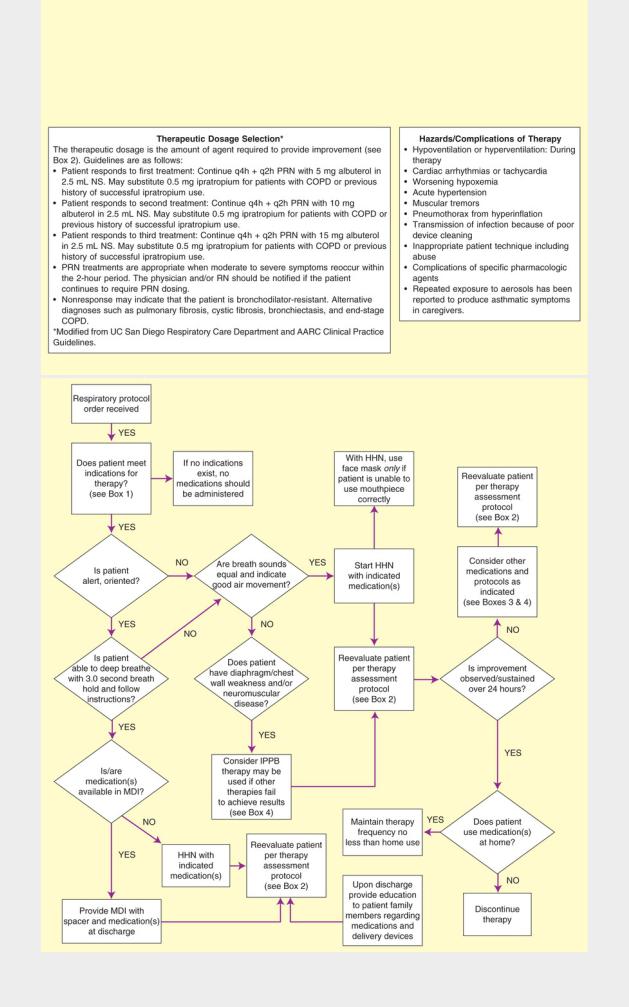
The AARC has developed protocols that are pertinent to the topic of Aerosolized Medication Therapy: IPPB Protocol, Secretion Clearance Protocol, Metered Dose Inhaler (MDI) Protocol, Small Volume Nebulizer (SVN) Protocol, Therapeutic Effective Dosage Protocol, DNA-ase Protocol, Inhaled Antibiotics Protocol, MDI Protocol for Ventilated

Patients, and several protocols for infants and pediatric patients (see Part XIII).
Also see Strickland, S. L., et al. (2015). AARC clinical practice guideline: Effectiveness of pharmacologic airway clearance therapies in hospitalized patients. Respiratory Care 60, 7, 1071-1077.
NOTE: Standard algorithmic protocol format is such that boxes = start, mandated action and/or end points and diamonds = a yes or no decision is required.
Table 10.1 illustrates common clinical manifestations (i.e., clinical indicators), initial assessments, and treatment selections routinely made by the TDP-practicing respiratory therapist.
TABLE 10.1
Clinical Manifestations, Assessments, and Treatment Selections Commonly Made by the Respiratory Therapist
Clinical Data (Indicators) |
Assessments |
Treatment Selections |
|||
Vital Signs |
|
|
|
|
|
↑ Breathing rate, blood pressure, |
Respiratory distress and dyspnea |
|
Treat underlying cause |
||
pulse |
|
|
|
|
|
Abnormal Airway Indicators |
|
|
|
||
Wheezing |
|
|
Bronchospasm |
|
Bronchodilator treatment |
Inspiratory stridor |
|
Laryngeal edema |
|
Racemic epinephrine |
|
Coarse crackles |
|
Secretions in large airways |
|
Airway clearance therapy |
|
Fine and medium crackles |
Secretions in distal airways |
|
Treat underlying cause, such as congestive heart |
||
|
|
|
|
|
failure |
|
|
|
|
|
Hyperinflation therapy |
Cough Effectiveness Indicators |
|
|
|
||
Strong cough |
|
|
Good ability to mobilize secretions |
|
None |
Weak cough |
|
|
Poor ability to mobilize secretions |
|
Airway clearance therapy |
Abnormal Secretion Indicators |
|
|
|
||
Amount: >25 mL/24 h |
Excessive bronchial secretions |
|
Airway clearance therapy |
||
White and translucent sputum |
Normal sputum |
|
None |
||
Yellow or opaque sputum |
Acute airway infection |
|
Treat underlying cause |
||
Green sputum |
|
Old, retained secretions and |
|
Airway clearance therapy |
|
Brown sputum |
|
infections |
|
Airway clearance therapy |
|
Red sputum |
|
Old blood |
|
Notify physician |
|
Frothy secretions |
|
Fresh blood |
|
Treat underlying cause, such as congestive |
|
|
|
|
Pulmonary edema |
|
heart failure |
|
|
|
|
|
Hyperinflation therapy |
Abnormal Lung Parenchyma Indicators |
|
||||
Bronchial breath sounds |
Atelectasis |
|
Hyperinflation therapy, oxygen treatment |
||
Dull percussion note |
|
Infiltrates or effusion |
|
Treat underlying cause |
|
Opacity on chest radiograph |
Fibrosis |
|
No specific treatment |
||
Restrictive pulmonary function |
Consolidation |
|
No specific, effective respiratory care treatment |
||
test values |
|
|
|
|
|
Depressed diaphragm on |
Air trapping and hyperinflation |
|
Treat underlying cause |
||
radiograph |
|
|
|
|
|
Abnormal Pleural Space Indicators |
|
||||
Hyperresonant percussion note |
Pneumothorax |
|
Evacuate air* and hyperinflation treatment |
||
Dull percussion note |
|
Pleural effusion |
|
Evacuate fluid* and hyperinflation treatment |
|
Abnormalities of Chest Shape and Motion |
|
||||
Paradoxical movement of the chest |
Flail chest |
|
Mechanical ventilation† |
||
wall |
|
|
|
|
|
Barrel chest |
|
|
Air trapping (hyperinflation) |
|
Treat underlying cause, such as asthma |
Posterior and lateral curvature of |
Kyphoscoliosis |
|
Airway clearance therapy |
||
spine |
|
|
|
|
|
Arterial Blood Gases—Ventilatory |
|
||||
pH ↑, PaCO |
↓, |
↓ |
Acute alveolar hyperventilation |
|
Treat underlying cause |
2 |
|
|
|
|
|
pH N, PaCO |
↓, |
↓↓† |
Chronic alveolar hyperventilation |
|
Generally none |
2 |
|
|
|
|
|
|
|
|
|
|
|
pH ↓, PaCO |
↑, |
↑ |
Acute ventilatory failure |
|
Mechanical ventilation* |
2 |
|
|
|
|
|
|
|
|
|
|
|
pH N, PaCO |
↑, |
↑↑ |
Chronic ventilatory failure |
|
Low-flow oxygen, bronchial hygiene |
2 |
|
|
|
|
|
|
|
|
|
||
Sudden Ventilatory Changes on Chronic Ventilatory Failure (CVF) |
|
||||
pH ↑, PaCO |
↑, |
↑↑, PaO ↓ |
Acute alveolar hyperventilation on |
Treat underlying cause |
|
2 |
|
2 |
CVF |
|
|
pH ↓, PaCO ↑↑, |
↑ PaO ↓ |
Acute ventilatory failure on CVF |
Mechanical ventilation* |
||
|
|
|
|||
22
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/

Metabolic
pH ↑, PaCO |
N or ↑, |
↑, |
|
Metabolic alkalosis |
Give potassium†—Hypokalemia |
PaO2 N |
2 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Give chloride†—Hypochloremia |
pH ↓, PaCO |
N or ↓, |
↓, |
|
Metabolic acidosis |
Give oxygen—Lactic acidosis |
PaO2 ↓ |
2 |
|
|
|
|
|
|
|
|
|
|
pH ↓, PaCO |
N or ↓, |
↓, |
|
Metabolic acidosis |
Give insulin*—Ketoacidosis |
PaO2 N |
2 |
|
|
|
|
|
|
|
|
|
|
pH ↓, PaCO |
N or ↓, |
↓, |
|
Metabolic acidosis |
Renal therapy |
PaO2 N |
2 |
|
|
|
|
|
|
|
|
|
|
Indication for Mechanical Ventilation |
|
||||
pH ↑, PaCO |
↓, |
↓, PaO |
↓ |
Impending ventilatory failure |
Mechanical ventilation |
|
2 |
2 |
|
|
|
|
|
|
|
|
|
pH ↓, PaCO |
↑, |
↑, PaO |
↓ |
Ventilatory failure |
Mechanical ventilation |
|
2 |
2 |
|
|
|
|
|
|
|
|
|
pH ↓, PaCO |
↑, |
↑, PaO |
↓ |
Apnea |
Mechanical ventilation |
|
2 |
2 |
|
|
|
|
|
|
|
|
|
Oxygenation Status |
|
|
|
|
|
PaO2 <80 mm Hg |
|
|
Mild hypoxemia |
Oxygen therapy and treat underlying cause |
|
PaO2 <60 mm Hg |
|
|
Moderate hypoxemia |
|
|
PaO2 <40 mm Hg |
|
|
Severe hypoxemia |
|
|
Oxygen Transport Status |
|
|
|
||
↓ PaO2, anemia, ↓ cardiac output |
Inadequate oxygen transport |
Oxygen therapy and treat underlying cause |
|||
*These procedures should be performed only as ordered by the physician. It should be noted that some of the treatment options are not included in respiratory protocols and may not necessarily be administered by respiratory therapists.
†Significant.
Severity Assessment
The frequency at which a respiratory therapy modality is to be administered is just as important to quality cost-efficient care as the current selection of the respiratory therapy modality itself. Often the frequency of treatment must be upregulated or down-regulated on a shift-by-shift, hour-to-hour, minute-to-minute, or even (in life-threatening situations) second-to-second basis. Such frequency changes must be made in response to a severity assessment.
In a good TDP program, the well-seasoned respiratory therapist routinely and systematically documents many severity assessments throughout each working day. For the new practitioner, however, a predesigned Severity Assessment Rating Form may be used to enhance this important part of the assessment process. One excellent, semiquantitative method of accomplishing this is illustrated in Table 10.2. The clinical application of severity assessment using this scale is provided in the following case example:
TABLE 10.2
Respiratory Care Protocol Severity Assessment
Item |
0 Points |
1 Point |
2 Points |
3 Points |
4 Points |
Respiratory history |
Negative for |
Smoking history |
Smoking history |
Pulmonary |
Severe or |
|
smoking or |
<1 pack a |
>1 pack a day |
disease |
exacerbation |
|
history not |
day |
|
|
|
|
available |
|
|
|
|
Surgery history |
No surgery |
General surgery |
Lower abdominal |
Thoracic or upper |
Thoracic with lung |
|
|
|
|
abdominal |
disease |
Level of |
Alert, oriented, |
Disoriented, |
Obtunded, |
Obtunded |
Comatose |
consciousness |
cooperative |
follows |
uncooperative |
|
|
|
|
commands |
|
|
|
Level of activity |
Ambulatory |
Ambulatory with |
Nonambulatory |
Paraplegic |
Quadriplegic |
|
|
assistance |
|
|
|
Respiratory pattern |
Normal rate 8– |
Respiratory rate |
Patient complains |
Dyspnea, use of |
Severe dyspnea, use |
|
20/min |
20–25/min |
of dyspnea |
accessory |
of accessory |
|
|
|
|
muscles, |
muscles, |
|
|
|
|
prolonged |
respiratory rate |
|
|
|
|
expiration |
>25, and/or |
|
|
|
|
|
swallow |
Breath sounds |
Clear |
Bilateral |
Bilateral fine, |
Bilateral |
Absent and/or |
|
|
crackles |
medium, or |
wheezing; fine, |
diminished |
|
|
|
coarse |
medium, or |
bilaterally and/or |
|
|
|
crackles |
coarse crackles |
severe wheezing; |
|
|
|
|
|
fine, medium, or |
|
|
|
|
|
coarse crackles |
Cough |
Strong, |
Excessive |
Excessive |
Thick bronchial |
Thick bronchial |
|
spontaneous, |
bronchial |
bronchial |
secretions and |
secretions but no |
|
nonproductive |
secretions |
secretions but |
weak cough |
cough |
|
|
and strong |
weak cough |
|
|
|
|
cough |
|
|
|
Chest radiograph |
Clear |
One lobe: |
Same lung, two |
One lobe in both |
Both lungs, more than |
|
|
Infiltrates, |
lobes: |
lungs: |
one lobe: |
|
|
atelectasis, |
Infiltrates, |
Infiltrates, |
Infiltrates, |
|
|
consolidation, |
atelectasis, |
atelectasis, |
atelectasis, |
|
|
or pleural |
consolidation, |
consolidation, |
consolidation, or |
|
|
effusion |
or pleural |
or pleural |
pleural effusion |
|
|
|
effusion |
effusion |
|
Arterial blood gases |
Normal |
Normal pH and |
Normal pH and |
Acute respiratory |
Acute respiratory |
and/or oxygen |
|
PaCO2 but |
PaCO2 but |
alkalosis, PaO2 |
failure, PaO2 <80 |
saturation |
|
PaO2 60–80 |
PaO2 40–60 |
<40 and/or |
and/or SpO2 <80% |
measured by |
|
and/or SpO2 |
and/or SpO2 |
SpO2 80%–84% |
|
pulse oximeter |
|
91%–96% |
85%–90% |
|
|
(SpO2) |
|
|
|
||
|
|
|
|
|
|
Severity Index |
|
|
|
|
|
Total Score |
|
Severity |
|
Treatment Frequency |
|
|
|
Assessment |
|
|
|
1–5 |
|
Unremarkable |
|
As needed |
|
6–15 |
|
Mild |
|
Two or three times a day |
|
16–25 |
|
Moderate |
|
Four times a day or as needed |
|
>26 |
|
Severe |
|
Two to four times a day and as needed; |
|
|
|
|
|
alert attending physician |
|
Severity Assessment Case Example
A 67-year-old man arrived in the emergency department in respiratory distress. The patient was well known to the therapist-driven protocol (TDP) team; he had been diagnosed with chronic bronchitis several years before this admission (3 points). The patient had no recent surgery history, and he was ambulatory, alert, and cooperative at the time of admission (0 points). He complained of dyspnea and was using his accessory muscles of inspiration (3 points). Auscultation revealed bilateral coarse crackles over both lung fields (3 points). His cough was weak and productive of thick gray sputum (3 points). A chest radiograph revealed pneumonia (consolidation) in the left lower lobe (3 points).
On room air his arterial blood gas values were pH 7.52, PaCO2 54,  41, and PaO2 52, suggesting an ABG-based
41, and PaO2 52, suggesting an ABG-based
diagnosis of acute alveolar hyperventilation superimposed on chronic ventilatory failure (3 points).
Using the Severity Assessment Form shown in Table 10.2, the following treatment selection and administration frequency would be appropriate:
Total score: 17 (moderate)
Treatment selection: Chest physical therapy
Frequency of administration: Four times a day; and as needed
The Essential Cornerstones of a Successful Therapist-Driven Protocol Program
Although there are many “assess and treat” respiratory care protocols (now more appropriately called Assess, Treat, and Teach Protocols) used throughout the health care industry today, the following respiratory protocols provide the essential
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
foundation of a successful TDP program3:
• Oxygen Therapy Protocol (Protocol 10.1, page 138)
Protocol 10.1
Oxygen Therapy Protocol1
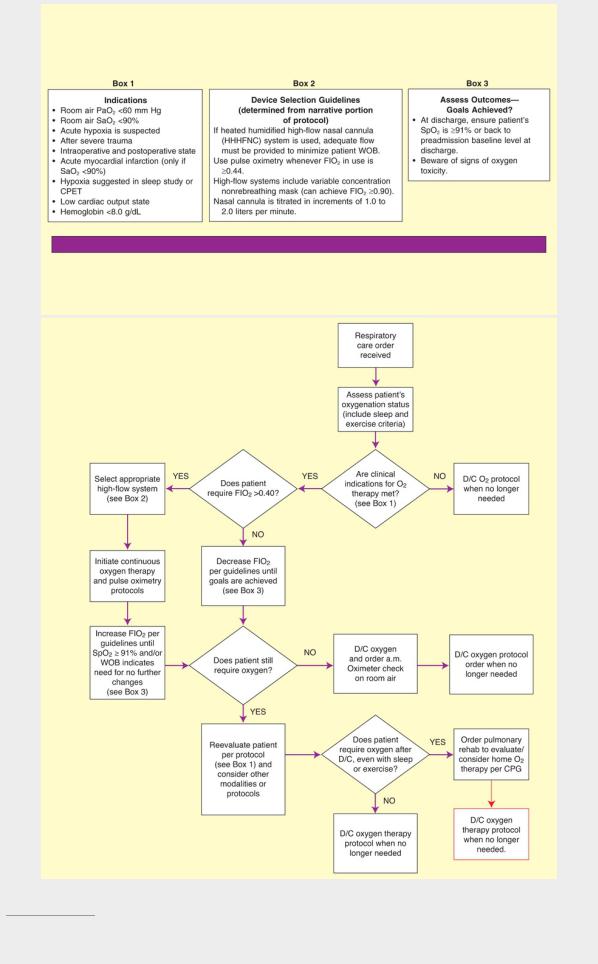
1The AARC has developed protocols pertinent to the topic of Oxygen Therapy. These include: Oxygen Protocol, Oxygen Protocol Addendum for Pulmonary Thromboendarterectomy (PET), Oxygen Delivery Device Protocol, Oxygen to Treat Pneumothorax Protocol, and Oximetry Protocol.
• Airway Clearance Therapy Protocol (Protocol 10.2, page 140)
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
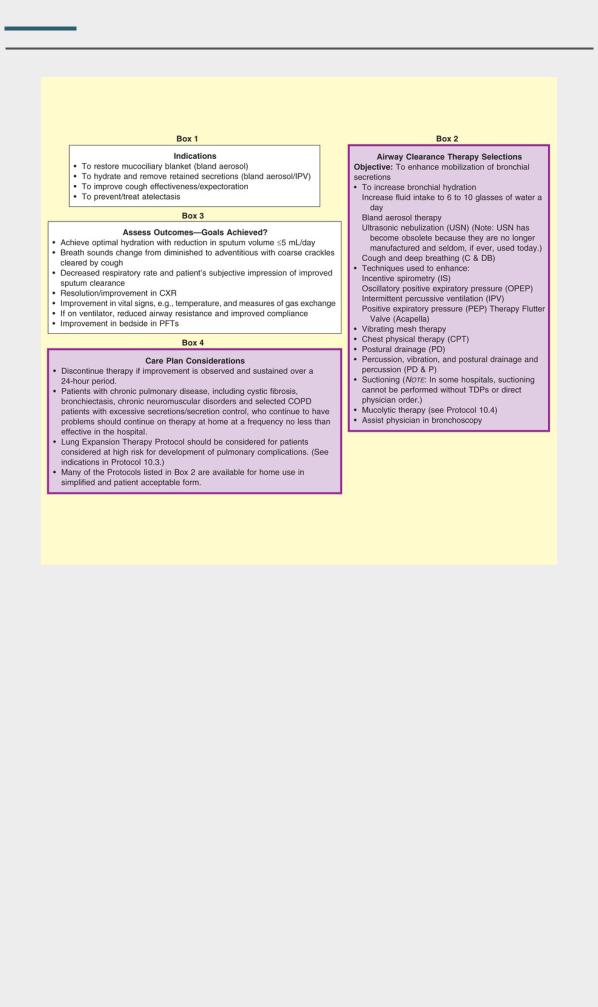
Protocol 10.2
Airway Clearance Therapy Protocol2
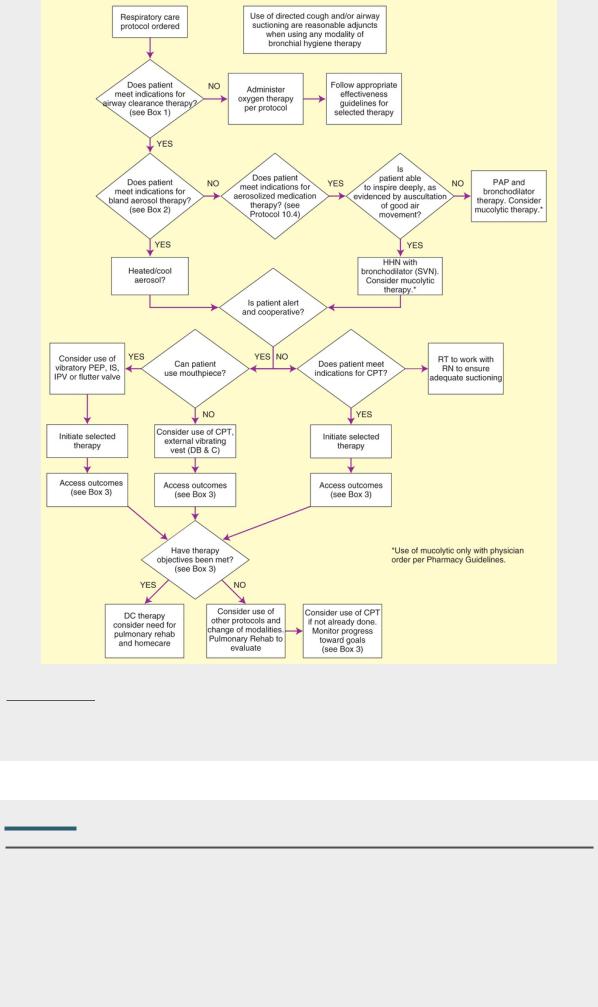
2The AARC has developed protocols that are pertinent to the topic of Airway Clearance Therapy. These include Secretion Clearance Protocol, Secretion Clearance Device Selection Protocol, Cough Assist Protocol, and Airway Management Protocol for Artificial Airways. Other KHN Protocols cross-referenced here include Suctioning Protocol (not shown) and Aerosolized Medication Protocol (see Protocol 10.4).
• Lung Expansion Therapy Protocol (Protocol 10.3, page 142)
Protocol 10.3
Lung Expansion Therapy Protocol3 (Hyperinflation Therapy)
Данная книга находится в списке для перевода на русский язык сайта https://meduniver.com/
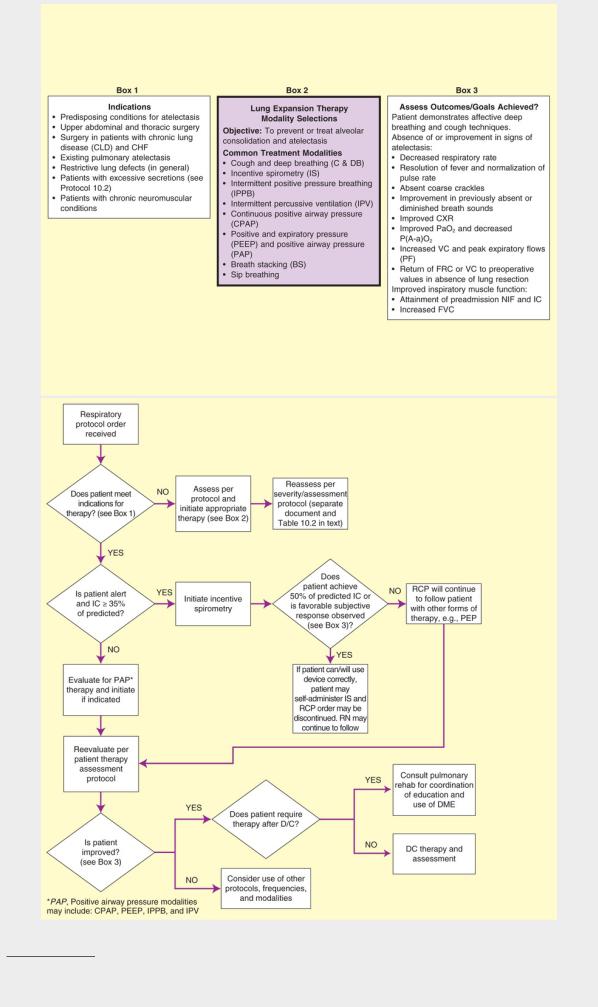
3The AARC has developed protocols that are pertinent to the topic of Lung Expansion Therapy. These include Secretion Clearance Protocols Atelectasis Prophylaxis, Prophylactic Protocol Addendum for Post-Operative Laparotomy, Chest Trauma, and Rib Fracture, IPPB Protocol, Cough Assist Protocol, and Airway Management
