
- •Rectal (medicine):
- •Classification:
- •Application location: Gastrointestinal/enteral:
- •Route from application to target:
- •Local or systemic effect:
- •Topical:
- •Enteral:
- •Parenteral:
- •Suppository:
- •Rectal suppositories:
- •Mode of insertion:
- •Vaginal suppositories:
- •Urethral suppositories:
- •Constituents:
- •Indications:
- •Artesunate suppositories:
- •Enema :
- •History:
- •Home usage:
- •Precautions:
- •Dry enema:
- •Nutrient enema:
- •Douche:
- •References:
DEPARTMENT
TECHNOLOGY OF DRUGS
THE PROJECT ON : ATL SUBJECT
DRUG DOSAGE FORMS OF RECTAL USE
PREPARED BY : Ammar Rashid
3rd group 1st group
CHECKED BY : assistant professor
For department of drug technology
Levachkova Yu.V
Definition:
Rectal medicines are medications prepared specifically for insertion into the rectum. They are compounded in many forms. Liquid rectal medicine solutions are given by enema. Creams, lotions and ointments are applied externally or inserted internally using an applicator. Suppositories are prepared by mixing medicine with a wax-like substance to form a semi-solid, bullet-shaped form that will melt after insertion into the rectum.
Purpose:
Rectal medications are administered for a localized effect on the rectum or for a systemic effect when a patient is vomiting, unable to swallow, or unconscious. Rectal medicine is most commonly used as a localized treatment for constipation or as a topical treatment for rectal inflammation orinfection. Rectal suppositories may be used for the treatment of fever, nausea, and pain; they may also be prescribed to induce sedation or bronchodilation, or to reduce the nausea and vomiting that can accompany chemotherapy. Medicated enemas may be used to cleanse the bowel, to combat bacteria, or to kill parasites.
Precautions:
Rectal medications must be used with caution in the cardiac patient who has arrhythmias or has recently had a myocardial infarction (i.e., heart attack). Insertion of a rectal medicine can cause vagus nerve stimulation and may trigger an arrhythmiauch as bradycardia. Rectal medicines should not be given to the patient with undiagnosed abdominal pain because peristalsis of the bowel can cause an inflamed appendix to rupture. Rectal medicines should be used cautiously in patients who have undergone recent surgery on the rectum, bowel, or prostate gland. If the patient has rectal bleeding or a prolapse of rectal tissue from the rectal opening, the medicine should be withheld and the physician consulted before administration. Rectal medicines should not be taken orally, and only medications labeled as rectal preparations should be placed in the rectum.
Description:
Administration of rectal medication should be done after the patient is positioned correctly. Lifting the upper buttocks will enable visualization of his or her rectal opening. External lotions, ointments or creams can be applied directly, using a gloved finger or a 4 gauze pad. Prior to administering internal rectal medicine, the tip of the suppository, enema catheter, or applicator should be lubricated with a water-soluble lubricant. To insert a rectal suppository, the lubricated, tapered end of the suppository should be placed at the rectal opening and gently pushed into the rectum. The suppository should be pushed continually toward the umbilicus until the full length of the nurse's gloved index finger has been inserted into the rectal opening (i.e., about 3 inches, or7.5 cm, for an adult patient). When inserting suppositories into children, the suppository should be pushed about 1 inch (2.5 cm) beyond the rectal opening, or up to the first knuckle of the nurses's index finger. When inserting suppositories into infants, the little finger should be inserted one-half inch (1.25 cm) beyond the rectal opening. The buttocks should be released and the finger removed.
Administration of internal rectal medicated cream or ointment requires placement of the applicator's lubricated tip at the rectal opening, gently pushing the applicator into the rectal opening about 3 inches (7.5 cm) for an adult (or as indicated on the applicator's directions). The correct dosage of medicine should then be squeezed into the rectum. After withdrawal of the applicator tip, the buttocks should be released.
To administer rectal medicine using an enema solution, the lubricated tip of the enema catheter must also be placed at the rectal opening. The tip of the catheter should then be gently advanced into the rectum, about 3 inches (7.5 cm) for an adult (or as indicated on the enema tubing). After the patient is alerted, the enema tubing should be opened, allowing the enema solution to flow into the rectum. A prepared enema should also be administered in this manner. When all of the solution has been administered, the enema catheter should be removed. Then, the buttocks should be released.
Preparation:
Before administering rectal medicine, the door to the room should be closed to assure patient privacy. The patient should be encouraged to empty his or her bladder and bowels before the procedure. After removing lower garments and underwear, the patient should be positioned in bed on his or her left side, with the top knee bent and pulled slightly upward. A waterproof pad should be placed under the patient's hips to protect the bedding, and a sheet should be draped over the patient to cover all of his or her body except the buttocks.
After placing a bedpan within quick access, the nurse should explain the procedure to the patient. This explanation should include the importance of breathing slowly through the mouth to enhance relaxation of the rectal sphincter and to avoid oppositional pressure. The patient should be made aware that there may be an urge to push the medicine out, but that he or she should try to hold it for at least 105 minutes after instillation (30 minutes for suppositories), as most rectal medications need time to be absorbed. It is advisable for the professional to check the medication label each time the medicine is given, to avoid medication errors. It must be the right medicine and the right dose (strength), the right time, the right patient, and the right method. The expiration date on the label should be inspected. If the medicine is outdated, it should not be used.
The nurse should wash his or her hands and put on gloves. The foil wrap should be removed from the rectal preparation or suppository. To prepare internal rectal creams, lotions or ointments, the applicator should be examined so that the nurse can estimate the proper amount to instill after insertion. In preparation for rectal enema instillations, the directions on the package of premixed disposable enemas should be read. Most premixed disposable enemas come with the tip already lubricated. The cap from the tip should be removed, and air should be expelled from the apparatus before use. If liquid medicine solutions are given using a standard enema bag and tubing, the procedure for enema instillation should be followed.
Arrhythmian irregularity of the heartbeat.
Bradycardian abnormal slowing of the heart rate to fewer than 60 beats per minute.
Myocardial infarction cardiac condition caused by decreased blood flow and oxygen to the heart muscle; may cause tissue death and heart damage. Commonly known as a heart attack.
Peristalsishe wave-like muscular contractions of the intestinal walls that move food and refuse through the gastrointestinal system.
Prostate gland gland found in males, located below the bladder and around the urethra, that secretes the fluid for semen and controls the release of urine from the bladder.
Rectumhe last portion of the large intestine located just above the anal canal, where stool collects prior to evacuation from the body.
Vagus nervene of the paired cranial nerves that supplies motor and sensory enervation to the abdominal and thoracic organs.
Aftercare:
After administering rectal medicines, the nurse should remain near the patient in case there is a need for assistance with the bedpan, or to walk to the bathroom. If a suppository is expelled within the first few minutes of insertion, the tip should be relubricated and reinserted. Medicated enemas that are expelled immediately may need to be repeated, using fresh solution. Directions provided with a prepared enema should be followed, but the physician may need to be consulted. To assist the patient with retaining the medicine, the nurse can apply gentle pressure to the rectal opening, using a 4 gauze pad or by squeezing the buttocks together after rectal medicine instillation. A 4 gauze pad should also tucked between the buttocks to collect seepage; this may help the patient feel more secure. After the procedure is completed, the patient should be covered and instructed to remain still for 105 minutes (30 minutes if a suppository was inserted). This period will allow time for medication absorption. Items that can be reused, such as enema pouches, tubing, and applicator tips, should be cleaned with warm running water and allowed to air-dry. Ointments and creams need to be recapped and returned to the medicine boxes. Disposable items and gloves should be placed in an appropriate trash bag that can be sealed and discarded.
Complications:
Rectal medicines can cause tissue irritation or allergic reactions. If irritation, swelling, redness, bleeding or prolapse of the rectal tissue is apparent, or if the patient complains of pain or burning, the medication should be stopped and the physician notified.
Results:
When given correctly, rectal medications work within 300 minutes to relieve pain, nausea, constipation, or fever. Rectal ointments for swelling and irritation of hemorrhoids may reverse the condition within several days. Because of their liquid state, rectal enemas are absorbed quickly and work rapidly. Retention enemas are meant to be held for 30 minutes to achieve full therapeutic effect.
Health care team roles:
Rectal medicines are administered by a licensed nurse (R.N. or L.P.N.) in the health care setting. An alert and cooperative patient may be allowed to apply external and internal rectal ointments and suppositories under the direction of the nurse. The nurse, however, should assess the site and the effectiveness of the medicine. The patient or members of the patient's family can be taught to administer rectal medicines in the home setting.
Rectal (medicine):
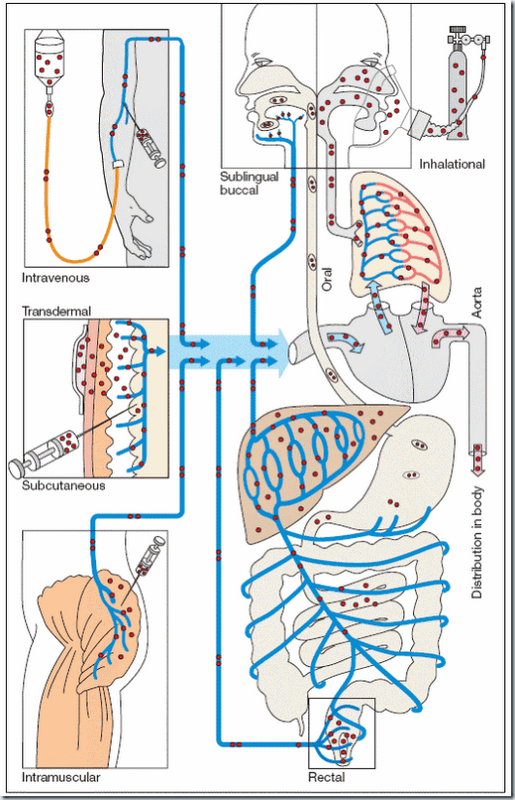
The rectal route of administration (ROA) is a way of administering drugs into the rectum to beabsorbed by the rectum's blood vessels[Note 1] and into the body's circulatory system which distributes the drug to the body's organs and various systems[Note 2] where the drug elicits its effects.
A drug that is administered rectally will in general (depending on the drug) have a faster onset, higher bioavailability, shorter peak, and shorter duration than the oral route.
Another advantage of administering a drug rectally is that it tends to produce less nauseacompared to the oral route and also prevents any amount of the drug from being lost due toemesis (vomiting, "throwing up", or "puking") since the drug is in the rectum, not the stomach, and the contents of the rectum are not lost when there is emesis.
In addition the rectal route bypasses first-pass metabolism, meaning the drug will reach the circulatory system with significantly less alteration and in greater concentration
Classification:
Routes of administration are usually classified by application location (or exposition). The route or course the active substance takes from application location to the location where it has its target effect is usually rather a matter of pharmacokinetics (concerning the processes of uptake, distribution, and elimination of drugs). Nevertheless,some,routes,,especially,the transdermal or transmucosal routes, are commonly referred to routes of administration. The location of the target effect of active substances are usually rather a matter of pharmacodynamics(concerning e.g. the physiological effects of drugs[2]). Furthermore, there is also a classification of routes of administration that basically distinguishes whether the effect is local (in "topical" administration) or systemic (in "enteral" or "parenteral" administration).
Application location: Gastrointestinal/enteral:
Administration through the gastrointestinal tract is sometimes termed enteral or enteric administration (strictly meaning 'through theintestines'). Enteral/enteric,administration usually.includes oral[3] (through the mouth) and rectal (into the rectum)[3] administration, in the sense that these are taken up by the intestines. However, uptake of drugs administered orally may also occur already in the stomach, whygastrointestinal (along the gastrointestinal tract) may be a more fitting word for this route of administration. Furthermore, some application locations often classified as enteral, such as sublingual[3] (under the tongue) and sublabial or buccal (between the cheek and gums/gingiva), are taken up in the proximal part of the gastrointestinal tract without reaching the intestines. Strictly enteral administration (directly into the intestines) can be used for systemic administration, as well as local (sometimes termed topical), such as in enema where e.g. contrast media is infused into the intestines for imaging. However, in the classification system basically distinguishing substances by location of their effects, the term enteral is reserved for substances with systemic effects.
Many drugs as tablets, capsules, or drops are taken orally. Administration methods directly into the stomach include those by gastric feeding tube or gastrostomy. Substances may also be placed into the small intestines, as with a duodenal feeding tube and enteral nutrition.Some enteric coated tablets will not dissolve in stomach but it is directed to the intestine because the drug present in the enteric coated tablet causes irritation in the stomach.
Central nervous system:
epidural (synonym: peridural) (injection or infusion into the epidural space), e.g. epidural anesthesia
intracerebral (into the cerebrum) direct injection into the brain. Used in experimental research of chemicals[4] and as a treatment for malignancies of the brain.[5] The intracerebral route can also interrupt the blood brain barrier from holding up against subsequent routes.[6]
intracerebroventricular (into the cerebral ventricles) administration into the ventricular system of the brain. One use is as a last line of opioid treatment for terminal cancer patients with intractable cancer pain.[7]
Other locations
epicutaneous or topical (application onto the skin). It can be used both for local effect as in allergy testing and typical local anesthesia, as well as systemic effects when the active substance diffuses through skin in a transdermal route.
intradermal, (into the skin itself) is used for skin testing some allergens, and also for mantoux test for Tuberculosis
subcutaneous (under the skin), e.g. insulin. Skin popping is a slang term that includes this method of administration, and is usually used in association with recreational drugs.
nasal administration (through the nose) can be used for topically acting substances, as well as for insufflation of e.g. decongestant nasal sprays to be taken up along the respiratory tract. Such substances are also called inhalational, e.g. inhalational anesthetics.
intravenous (into a vein), e.g. many drugs, total parenteral nutrition
intraarterial (into an artery), e.g. vasodilator drugs in the treatment of vasospasm and thrombolytic drugs for treatment of embolism
intramuscular (into a muscle), e.g. many vaccines, antibiotics, and long-term psychoactive agents. Recreationally the colloquial term 'muscling' is used.[8]
intracardiac (into the heart), e.g. adrenaline during cardiopulmonary resuscitation (no longer commonly performed)
intraosseous infusion (into the bone marrow) is, in effect, an indirect intravenous access because the bone marrow drains directly into the venous system. This route is occasionally used for drugs and fluids in emergency medicine and pediatrics when intravenous access is difficult.
intrathecal (into the spinal canal) is most commonly used for spinal anesthesia and chemotherapy
intraperitoneal, (infusion or injection into the peritoneum) e.g. peritoneal dialysis
Intravesical infusion is into the urinary bladder.
intravitreal, through the eye
Intracavernous injection, an injection into the base of the penis
Intravaginal administration, in the vagina
Intrauterine
Extra-amniotic,administration,between the endometrium and fetal membranes

