
2 Journal of Cardiovascular Medicine 2017, Vol 00 No 00
Methods
Study population
We prospectively collected clinical data from all consecutive patients who had successful CRT device (CRT-P or CRT-D) implantation at a single UK tertiary centre between February 2008 and December 2011. All patients had CHF because of severe LVSD (LV ejection fraction <35%), QRS duration more than 120 ms and were receiving OMT. All except five patients had left bundle branch block. These data were collected as a prospective service evaluation as part of the Leeds Teaching Hospitals NHS Trust audit program.
Baseline assessment
Baseline clinical and demographic data including were collected prospectively for all patients including: New York Heart Association (NYHA) functional classification, aetiology, previous cardiac history including recent admissions, resting 12-lead electrocardiographic data, and blood test variables, including full blood count, serum creatinine, urea, and electrolytes. The presence of comorbidities including diabetes mellitus and airways disease were collected (determined at baseline from past medical history and/or treatment with hypoglycaemic medication and inhalers, respectively). Ischaemic aetiology was determined by the clinician assessing the patient on the basis of a detailed past medical history (atherosclerosis risk factors, angina symptoms, or previous myocardial infarction), or the presence of Q waves on ECG (if no bundle branch block) and taking into account available cardiovascular MRI, single-photon emission computed tomography, and angiography information. Pharmacotherapy data were collected regarding the use of aldosterone antagonists, angiotensin-converting enzyme inhibitors (ACEis), angiotensin receptor blockers (ARBs), b-blockers, digoxin, amiodarone, and loop diuretics. Doses of loop diuretic therapy were converted to furosemide equivalent.
Device implantation
CRT implantation was undertaken according to a standard approach. All patients received an apical right ventricular lead, and atrial lead if there was evidence of sinus rhythm on an electrocardiogram in the year preceding to implant and a lateral LV lead. The choice of CRT device (CRT-P or CRT-D) was left at the discretion of the implanting cardiologist following the relevant UK guidelines.14
Outcomes
The prespecified primary study end point was all-cause mortality. Survival status was established from electronic and paper medical records. Data were censored to 31 May 2014. A subgroup analysis was performed in patients with ischaemic cardiomyopathy.
Mode-specific mortality
A subgroup mode-specific mortality analysis was performed on a proportion of patients in this cohort who were also participating in a prospective observational cohort study (UK-HEART-2). In this subgroup, there were 323 patients (41%). All patients recruited to UK-HEART-2 were registered with the United Kingdom office of population, census, and surveys which provided details of death. The Leeds West Research Ethics Committee had provided ethical approval for the study and all patients had provided written informed consent. Two physicians reviewed all the available information from autopsy findings, medical records, and death certificates to evaluate all deaths. Modes of death were categorized into cardiovascular death and noncardiovascular. Cardiovascular deaths were further subclassified as progressive heart failure (death following documented haemodynamic or symptomatic deterioration), sudden death (if occurred within 1 h of change in symptoms or during sleep) or other cardiovascular death (e.g. myocardial infarction, cerebrovascular accident – if not occurring suddenly or associated with heart failure progression). Detailed classification criteria have been documented elsewhere.13 For the purpose of this study, data were censored to 31 May 2014.
Statistical analysis
Descriptive group data are presented as mean SD for continuous data and percentage (number) for categorical data. Groups were compared using Student’s t-test or Mann–Whitney U test for continuous variables and Pearson’s x2 statistic or Fisher’s exact test for categorical variables, using two-sided tests. Log-rank tests were used to compare unadjusted survival of groups. Multivariate Cox regression analyses were used to calculate adjusted mortality, estimate hazard ratios, and 95% confidence intervals (CIs). Adjusted analyses included combinations of age, sex, clinical variables (ischaemic aetiology, NYHA class, atrial fibrillation (AF), QRS duration, haemoglobin, creatinine, coronary artery bypass graft, and percutaneous coronary intervention) and therapeutic variables (ACEi/ARB, amiodarone, b-blocker, and digoxin). Propensity scores were estimated using a logistic model using all of these variables and one-to-one propensity score matching based on the log odds ratio was undertaken as a sensitivity analysis. All statistical tests were two-sided and called significant at the 5% level. Statistical analyses were performed with SPSS version 20 (SPSS Inc., Chicago, Illinois, USA) and propensity score matching with Stata version 13 (StataCorp, College Station, Texas, USA).
Results
Baseline characteristics
A total of 795 patients had successful CRT device implantation with lateral lead position between February 2008 and December 2011. We failed to implant eight patients (in whom lateral vein was not present or unsuitable for lead placement) and a secondary procedure with
© 2017 Italian Federation of Cardiology. All rights reserved.
CRT-P v CRT-D in CHF Drozd et al. 3
ultimate success was required in ten patients. Overall mean age of patients with a successful implant was 73 years (SD 11). CRT-P was implanted in 544 patients (68%) and the remaining 251 patients (32%) received CRT-D. Baseline characteristics of the two groups are summarized in Table 1. LV pacing percentage was not different between patients who received CRT-D or CRT-P (94 versus 96%, P ¼0.30).
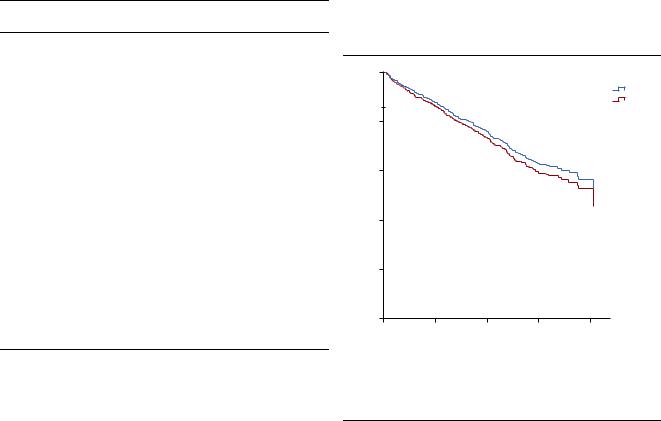
survival benefit in those patients implanted with a CRT- D compared with CRT-P (hazard ratio 1.09, 95% CI 0.84–1.41, P ¼0.51). After adjusting for baseline differences including aetiology, there was similarly no mortality difference (hazard ratio 1.16, CI 0.82–1.63, P ¼0.41; Fig. 1). Sensitivity analyses in the propensity matched groups showed similar results to adjusted analysis.
Patients who had a CRT-D device implanted were younger, more likely to be men, more likely to have ischaemic cardiomyopathy and have less symptomatic heart failure (NYHA class). They were less likely to have AF, had shorter QRS durations, higher haemoglobin, and lower creatinine. Revascularization (coronary artery bypass graft or percutaneous coronary intervention) was more common in individuals receiving CRT-D devices. Patients with a CRT-D device were also more likely to be taking ACEi/ ARB, amiodarone, b-blockers and less likely to be using digoxin compared with patients with CRT-P devices.
Mortality outcomes
Data for 2277 patient-years of follow-up are presented. During a mean follow-up of 1072 556 days, there were a total of 272 deaths (34.2%), 189 (35%) in the CRT-P group and 83 (33%) in the CRT-D group. There was no
Mortality outcomes in patients with ischaemic cardiomyopathy
In this cohort, 530 patients (66.7%) had CHF because of ischaemic aetiology. Baseline clinical characteristics of patients with ischaemic cardiomyopathy are summarized in Table 2. In patients with ischaemic cardiomyopathy, there was improved survival with CRT-D compared with CRT-P (hazard ratio 0.72, 95% CI 0.54–0.95, P ¼0.02); however, this was not significant after adjustment for age and sex (hazard ratio 0.85, 95% CI 0.61–1.17, P ¼0.31). After further adjustment for clinical and treatment variables that were different between the groups this remained nonsignificant (hazard ratio 1.1 95% CI 0.77–1.65, P ¼0.54; Fig. 2). Sensitivity analyses in the propensity-matched groups showed similar results to adjusted analysis. In 265 patients (33.3%) with nonischaemic cardiomyopathy, there was no survival benefit with CRT-D (hazard ratio 0.98, 95% CI 0.42–2.27, P ¼0.96) which persisted after adjustment (hazard ratio 0.78, CI 0.23–2.7, P ¼0.70).
Table 1 Baseline characteristics of cardiac resynchronization therapy |
|
|
|
|
|
|
|||||||
with pacemaker and cardiac resynchronization therapy with |
|
Mode-specific mortality |
|
|
|||||||||
defibrillator patients |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
|
|
In this cohort, 323 patients (41%) were also enrolled in |
||||||
|
Total cohort |
CRT-P |
CRT-D |
|
|||||||||
|
P valuea |
the UK-HEART-2 study. There were a total of 89 deaths |
|||||||||||
|
(n ¼795) |
(n ¼544) |
(n ¼251) |
||||||||||
Age (years) |
73.3 10.6 |
75.1 10.3 |
69.3 10.0 |
0.001 |
Fig. 1 |
|
|
|
|
||||
Male sex |
79 |
(633) |
74 |
(400) |
93 |
(232) |
<0.001 |
|
|
|
|
|
|
Clinical factors |
|
|
|
|
|
|
|
|
100 |
|
|
|
|
Ischaemic aetiology |
67 |
(532) |
54 |
(284) |
90 |
(226) |
<0.001 |
|
|
|
|
|
|
|
|
|
|
|
CRT-P |
||||||||
NYHA class |
|
|
|
|
|
|
<0.001 |
|
|
|
|
|
|
I |
2 |
(18) |
2 |
(10) |
3 |
(8) |
|
|
|
|
|
|
CRT-D |
II |
20 |
(162) |
15 |
(73) |
36 |
(89) |
|
|
80 |
|
|
|
|
III |
63 |
(505) |
74 |
(364) |
57 |
(141) |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|||||||
IV |
7 |
(53) |
9 |
(45) |
3 |
(8) |
|
|
|
|
|
|
|
AF |
31 |
(249) |
35 |
(191) |
23 |
(58) |
<0.001 |
|
|
|
|
|
|
COPD |
11 |
(88) |
11 |
(600) |
11 |
(28) |
1.00 |
|
|
|
|
|
|
Diabetes mellitus |
25 |
(198) |
24 |
(128) |
27 |
(67) |
0.38 |
(%) |
60 |
|
|
|
|
Heart rate (bpm) |
67 17 |
66.8 18.2 |
66.7 13.6 |
0.10 |
40 |
|
|
|
|
||||
Creatinine (mmol/l) |
128 5.0 |
130.9 61.0 |
121.8 36.9 |
0.01 |
Survival |
|
|
|
|
||||
QRS duration (ms) |
154 26 |
156.4 27.0 |
150.0 24.4 |
0.002 |
|
|
|
|
|
|
|||
Haemoglobin (g/dl) |
13.1 3.9 |
12.9 1.7 |
13.5 6.4 |
0.04 |
|
|
|
|
|
|
|||
Treatment factors |
|
|
|
|
|
|
|
|
|
|
|
|
|
Elective procedure |
75 |
(600) |
78 |
(423) |
75 |
(187) |
0.32 |
|
|
|
|
|
|
CABG |
27 |
(212) |
20 |
(109) |
41 |
(103) |
<0.001 |
|
|
|
|
|
|
PCI |
14 |
(108) |
9 |
(51) |
23 |
(57) |
<0.001 |
|
20 |
|
|
|
|
Valvular surgery |
7 |
(59) |
8 |
(44) |
6 |
(15) |
0.31 |
|
|
|
|
|
|
ACEi/ARB use |
86 |
(683) |
84 |
(452) |
92 |
(230) |
0.001 |
|
|
|
Adjusted HR = 1.16 (0.82-1.63) |
|
|
Amiodarone use |
9 |
(70) |
5 |
(28) |
17 |
(42) |
<0.001 |
|
|
|
|
||
Anticoagulation use |
35 |
(281) |
37 |
(200) |
32 |
(81) |
0.20 |
|
|
|
P = 0.41 |
|
|
b-blocker use |
78 |
(619) |
74 |
(397) |
88 |
(221) |
<0.001 |
|
0 |
|
|
|
|
Digoxin use |
17 |
(134) |
20 |
(105) |
12 |
(29) |
0.01 |
|
|
|
|
|
|
|
0 |
500 |
1000 |
1500 |
3000 |
||||||||
Furosemide dose (mg) |
58 53 |
58.2 54.9 |
58.1 49.0 |
0.97 |
|
||||||||
|
|
|
Follow-up (days) |
|
|||||||||
Values are given as % of patients (number) or mean SD. a P value between CRT-P versus CRT-DACEi/ARB, ACE inhibitor or angiotensin receptor blocker; AF, atrial fibrillation; CABG, coronary artery bypass graft; COPD, chronic obstructive pulmonary disease; CRT-D, cardiac resynchronization therapy with defibrillator; CRT-P, cardiac resynchronization therapy with pacemaker; NYHA, New York Heart Association; PCI, percutaneous coronary intervention.
Adjusted survival curve for all-cause mortality comparing CRT-D versus CRT-P. CRT-D, cardiac resynchronization therapy with defibrillator; CRT-P, cardiac resynchronization therapy with pacemaker; HR, hazard ratio.
© 2017 Italian Federation of Cardiology. All rights reserved.
