
KAPLAN_USMLE_STEP_1_LECTURE_NOTES_2018_BIOCHEMISTRY_and_GENETICS
.pdf
Chapter 10 ● Vitamins
Vision
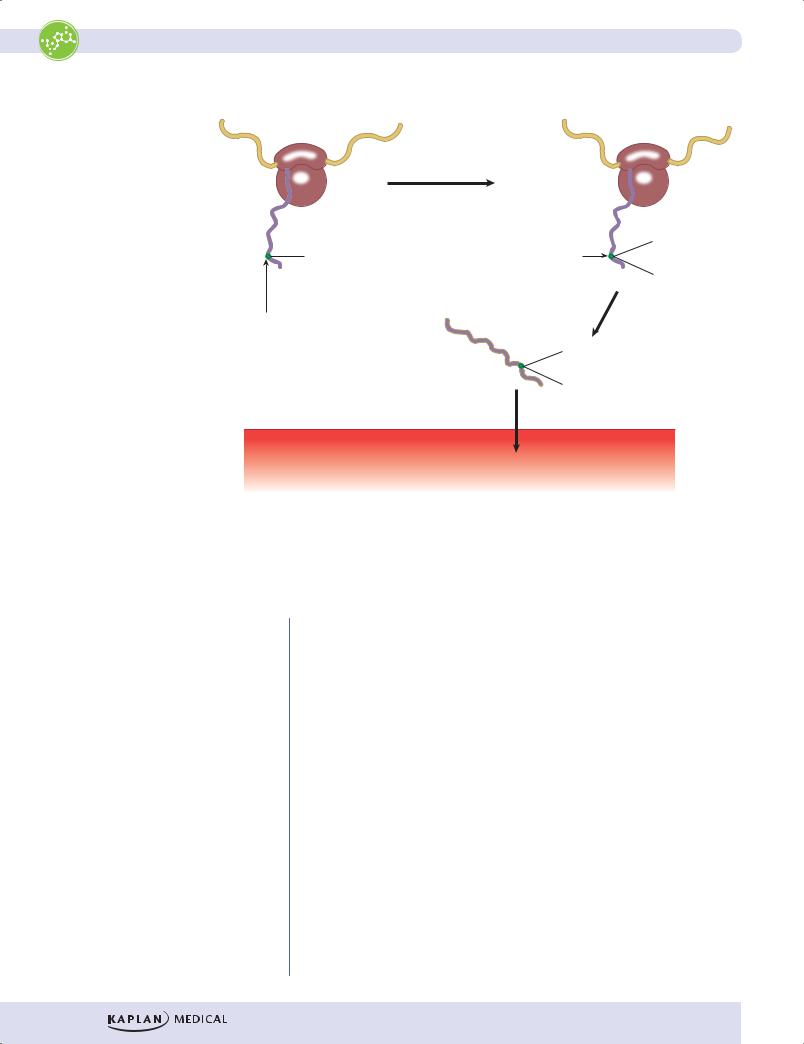
When first formed, all the double bonds in the conjugated double bond system in retinal are in the trans configuration. This form, all-trans retinal is not active. The conversion of all-trans retinal to the active form cis-retinal takes place in the pigmented epithelial cells. Cis-retinal is then transferred to opsin in the rod cells forming the light receptor rhodopsin. It functions similarly in rod and cone cells. When exposed to light, cis-retinal is converted all-trans retinal. A diagram of the signal transduction pathway for light-activated rhodopsin in the rod cell is shown in Figure I-10-2, along with the relationship of this pathway to rod cell anatomy and changes in the membrane potential. Note the following points:
•Rhodopsin is a 7-pass receptor coupled to the trimeric G protein transducin (Gt).
•When light is present, the pathway activates cGMP phosphodiesterase, which lowers cGMP.
•Rhodopsin and transducin are embedded in the disk membranes in the outer rod segment.
•cGMP-gated Na+ channels in the cell membrane of the outer rod segment respond to the decrease in cGMP by closing and hyperpolarizing the membrane.
•The rod cell is unusual for an excitable cell in that the membrane is partially depolarized (~ –30 mV) at rest (in darkness) and hyperpolarizes on stimulation.
Because the membrane is partially depolarized in the dark, its neurotransmitter glutamate is continuously released. Glutamate inhibits the optic nerve bipolar cells with which the rod cells synapse. By hyperpolarizing the rod cell membrane, light stops the release of glutamate, relieving inhibition of the optic nerve bipolar cell and thus initiating a signal into the brain.
155

Part I ● Biochemistry
Outer |
Rhodopsin |
Intradisk space |
|
|
|||
|
|
|
|
|
|
||
rod |
|
|
|
|
|
|
|
segment |
|
|
|
|
|
|
|
|
|
α |
|
β |
cGMP |
|
|
|
|
|
γ |
PDE |
Light |
|
|
|
Cytoplasm |
|
Gt |
|
Light |
cGMP |
|
|
|
|
|
|
Dark |
|
|
|
|
|
|
|
5´GMP |
+ |
|
|
|
|
|
(inactive) |
cGMP |
||
|
Light |
|
|
|
|
|
Na+ |
|
|
|
|
|
|
|
|
|
–30 |
|
|
|
|
|
|
|
Membrane |
|
|
|
|
|
|
|
potential |
|
|
|
|
|
|
Inner |
(meV) |
|
|
|
|
Cell membrane |
|
–35 |
|
|
|
|
|||
rod |
3 sec |
|
|
|
|
|
|
segment |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Bipolar
cell
Light
Figure I-10-2. Light-Activated Signal Transduction in the Retinal Rod Cell
156

Chapter 10 ● Vitamins
Vitamin K Deficiency
A 79-year-old man living alone called his 72-year-old sister and then arrived at the hospital by ambulance complaining of weakness and having a rapid heartbeat. His sister said that he takes no medications and has a history of poor nutrition and poor hygiene. Physical examination confirmed malnourishment and dehydration. A stool specimen was positive for occult blood. He had a prolonged prothrombin time (PT), but his liver function tests (LFTs) were within normal range. He was given an injection of a vitamin that corrected his PT in 2 days.
Poor nutrition and malnourishment, lack of medications, occult blood in the stool specimen, prolonged PT, and normal LFTs are all consistent with vitamin K deficiency. Without vitamin K, several blood clotting factors (prothrombin, X, IX, VII) are not γ-carboxylated on glutamate residues by the γ-glutamyl carboxylase during their synthesis (cotranslational modification) in hepatocytes. The PT returned to normal 2 days after a vitamin K injection.
Vitamin K deficiency should be distinguished from vitamin C deficiency.
Table I-10-3. Vitamin K versus Vitamin C Deficiency
|
Vitamin K Deficiency |
|
Vitamin C Deficiency |
|
|
|
|
|
|
|
|
|
Easy bruising, bleeding |
|
Easy bruising, bleeding |
||
|
|
|
|
|
|
|
Normal bleeding time |
|
Increased bleeding time |
||
|
|
|
|
|
|
|
Increased PT |
|
Normal PT |
||
|
|
|
|
|
|
|
Hemorrhagic disease with no |
|
• |
Gum hyperplasia, inflammation, |
|
|
connective tissue problems |
|
|
loss of teeth |
|
|
|
|
• Skeletal deformity in children |
||
|
|
|
• |
Poor wound healing |
|
|
|
|
• |
Anemia |
|
|
|
|
|
|
|
|
Associated with: |
|
Associated with: |
||
|
• Fat malabsorption |
|
• Diet deficient in citrus fruit, green |
||
|
• Long-term antibiotic therapy |
|
|
vegetables |
|
|
|
|
|
|
|
•Breast-fed newborns
•Infant whose mother was taking anticonvulsant therapy during pregnancy
159

Chapter 10 ● Vitamins
Review Questions
Select the ONE best answer.
1.Retinitis pigmentosa (RP) is a genetically heterogeneous disease characterized by progressive photoreceptor degeneration and ultimately blindness. Mutations in more than 20 different genes have been identified in clinically affected patients. Recent studies have mapped an RP locus to the chromosomal location of a new candidate gene at 5q31. One might expect this gene to encode a polypeptide required for the activity of a(n)
A.receptor tyrosine kinase
B.cGMP phosphodiesterase
C.phospholipase C
D.adenyl cyclase
E.protein kinase C
2.A 27-year-old woman with epilepsy has been taking phenytoin to control her seizures. She is now pregnant, and her physician is considering changing her medication to prevent potential bleeding episodes in the infant. What biochemical activity might be deficient in the infant if her medication is continued?
A.Hydroxylation of proline
B.Glucuronidation of bilirubin
C.Reduction of glutathione
D.γ-Carboxylation of glutamate
E.Oxidation of lysine
3.A 75-year-old woman is seen in the emergency room with a fractured arm. Physical examination revealed multiple bruises and perifollicular hemorrhages, periodontitis, and painful gums. Her diet consists predominately of weak coffee, bouillon, rolls, and plain pasta. Lab results indicated mild microcytic anemia. Which of the following enzymes should be less active than normal in this patient?
A.Homocysteine methyltransferase
B.γ-Glutamyl carboxylase
C.Dihydrofolate reductase
D.ALA synthase
E.Prolyl hydroxylase
161
Part I ● Biochemistry
Answers
1.Answer: B. Only phosphodiesterase participates as a signaling molecule in the visual cycle of photoreceptor cells.
2.Answer: D. Phenyl hydantoins decrease the activity of vitamin K, which is required for the γ-carboxylation of coagulation factors (II, VII, IX, X), as well as proteins C and S.
3.Answer: E. The patient has many signs of scurvy from a vitamin C deficiency. The diet, which contains no fruits or vegetables, provides little vitamin C. Prolyl hydroxylase requires vitamin C, and in the absence of hydroxylation, the collagen α-chains do not form stable, mature collagen. The anemia may be due to poor iron absorption in the absence of ascorbate.
162
Energy Metabolism 11
Learning Objectives
Explain information related to metabolic sources of energy
Interpret scenarios about metabolic energy storage and fuel metabolism
Answer questions about patterns of fuel metabolism in tissues
METABOLIC SOURCES OF ENERGY
Energy is extracted from food via oxidation, resulting in the end products carbon dioxide and water. This process occurs in 4 stages.
In stage 1, metabolic fuels are hydrolyzed in the gastrointestinal (GI) tract to a diverse set of monomeric building blocks (glucose, amino acids, and fatty acids) and absorbed.
In stage 2, the building blocks are degraded by various pathways in tissues to a common metabolic intermediate, acetyl-CoA.
•Most of the energy contained in metabolic fuels is conserved in the chemical bonds (electrons) of acetyl-CoA.
•A smaller portion is conserved in reducing nicotinamide adenine dinucleotide (NAD) to NADH or flavin adenine dinucleotide (FAD) to FADH2.
•Reduction indicates the addition of electrons that may be free, part of a hydrogen atom (H), or a hydride ion (H–).
In stage 3, the citric acid (Krebs, or tricarboxylic acid [TCA]) cycle oxidizes acetyl-CoA to CO2. The energy released in this process is primarily conserved by reducing NAD to NADH or FAD to FADH2.
The final stage is oxidative phosphorylation, in which the energy of NADH and FADH2 is released via the electron transport chain (ETC) and used by an ATP synthase to produce ATP. This process requires O2.
163
